Abstract
Rationale
What is the difference between aripiprazole and brexpiprazole?
Objectives
This systematic review, network meta-analysis of randomized trials evaluated the efficacy and safety/tolerability of aripiprazole and brexpiprazole for treating acute schizophrenia.
Methods
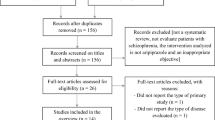
We searched Scopus, MEDLINE, and Cochrane Library from inception until May 22, 2019. The response rate was set as the primary outcome. Other outcomes were discontinuation rate and incidence of individual adverse events. The risk ratio (RR) and 95% credible interval (95%CrI) were calculated.
Results
Fourteen studies were identified (n = 3925). Response rates of both aripiprazole and brexpiprazole were superior to that of the placebo (RR [95%CrI]: aripiprazole = 0.84 [0.78, 0.92], brexpiprazole = 0.84 [0.77, 0.92]). Aripiprazole and brexpiprazole were associated with a lower incidence of all-cause discontinuation (0.80 [0.71, 0.89], 0.83 [0.72, 0.95]), adverse events (0.67 [0.47, 0.97], 0.64 [0.46, 0.94]), and inefficacy (0.56 [0.40, 0.77], 0.68 [0.48, 0.99]) compared with the placebo. Although brexpiprazole was associated with a lower incidence of schizophrenia as an adverse event compared with the placebo (0.57 [0.37, 0.85]), aripiprazole and brexpiprazole were associated with a higher incidence of weight gain compared with the placebo (2.12 [1.28, 3.68], 2.14 [1.35, 3.42]). No significant differences were found in other individual adverse events, such as somnolence, akathisia, extrapyramidal symptoms, and dizziness between aripiprazole or brexpiprazole and placebo. Any outcome between aripiprazole and brexpiprazole were not different.
Conclusions
Differences in short-term efficacy and safety for acute schizophrenia were not apparent between aripiprazole and brexpiprazole. Future studies are warranted to evaluate whether there are differences in the long-term outcome between treatments.


Similar content being viewed by others
References
2002 S9 (2002) Center for drug evaluation and research. Application number 21–436. Medical review(s). https://www.fdagov
Belgamwar RB, El-Sayeh HG (2011) Aripiprazole versus placebo for schizophrenia. Cochrane Database Syst Rev: CD006622
Brooks S, Gelman A (1998) General methods for monitoring convergence of iterative simulations. J Comput Graph Stat 7:434–455
Cantillon M, Prakash A, Alexander A, Ings R, Sweitzer D, Bhat L (2017) Dopamine serotonin stabilizer RP5063: a randomized, double-blind, placebo-controlled multicenter trial of safety and efficacy in exacerbation of schizophrenia or schizoaffective disorder. Schizophr Res 189:126–133
Citrome L, Ota A, Nagamizu K, Perry P, Weiller E, Baker RA (2016) The effect of brexpiprazole (OPC-34712) and aripiprazole in adult patients with acute schizophrenia: results from a randomized, exploratory study. Int Clin Psychopharmacol 31:192–201
Cochrane (2011) Cochrane Handbook for Systematic Reviews of Interventions
Correll CU, Skuban A, Ouyang J, Hobart M, Pfister S, McQuade RD, Nyilas M, Carson WH, Sanchez R, Eriksson H (2015) Efficacy and safety of brexpiprazole for the treatment of acute schizophrenia: a 6-week randomized, double-blind, placebo-controlled trial. Am J Psychiatry 172:870–880
Correll CU, Skuban A, Hobart M, Ouyang J, Weiller E, Weiss C, Kane JM (2016) Efficacy of brexpiprazole in patients with acute schizophrenia: review of three randomized, double-blind, placebo-controlled studies. Schizophr Res 174:82–92
Cutler AJ, Marcus RN, Hardy SA, O'Donnell A, Carson WH, McQuade RD (2006) The efficacy and safety of lower doses of aripiprazole for the treatment of patients with acute exacerbation of schizophrenia. CNS Spectr 11:691–702 quiz 719
DerSimonian R, Laird N (1986) Meta-analysis in clinical trials. Control Clin Trials 7:177–188
Dias S, Welton NJ, Caldwell DM, Ades AE (2010) Checking consistency in mixed treatment comparison meta-analysis. Stat Med 29:932–944
Durgam S, Cutler AJ, Lu K, Migliore R, Ruth A, Laszlovszky I, Nemeth G, Meltzer HY (2015) Cariprazine in acute exacerbation of schizophrenia: a fixed-dose, phase 3, randomized, double-blind, placebo- and active-controlled trial. J Clin Psychiatry 76:e1574–e1582 FDA https://www.fda.gov/
Guy W (1976) ECDEU assessment manual for psychopharmacology: US Department of Health, Education and Welfare Publication (ADM). National Institute of Mental Health, Rockville, pp 76–338
Higgins J, Green S (2011) Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. In: Collaboration TC (ed). http://handbook.cochrane.org
Huhn M, Nikolakopoulou A, Schneider-Thoma J, Krause M, Samara M, Peter N, Arndt T, Backers L, Rothe P, Cipriani A, Davis J, Salanti G, Leucht S (2019) Comparative efficacy and tolerability of 32 oral antipsychotics for the acute treatment of adults with multi-episode schizophrenia: a systematic review and network meta-analysis. Lancet 394:939–951
Ishigooka J, Iwashita S, Tadori Y (2018) Efficacy and safety of brexpiprazole for the treatment of acute schizophrenia in Japan: a 6-week, randomized, double-blind, placebo-controlled study. Psychiatry Clin Neurosci
Kane JM, Carson WH, Saha AR, McQuade RD, Ingenito GG, Zimbroff DL, Ali MW (2002) Efficacy and safety of aripiprazole and haloperidol versus placebo in patients with schizophrenia and schizoaffective disorder. J Clin Psychiatry 63:763–771
Kane JM, Meltzer HY, Carson WH Jr, RD MQ, Marcus RN, Sanchez R, Aripiprazole Study Group (2007) Aripiprazole for treatment-resistant schizophrenia: results of a multicenter, randomized, double-blind, comparison study versus perphenazine. J Clin Psychiatry 68:213–223
Kane JM, Skuban A, Ouyang J, Hobart M, Pfister S, McQuade RD, Nyilas M, Carson WH, Sanchez R, Eriksson H (2015) A multicenter, randomized, double-blind, controlled phase 3 trial of fixed-dose brexpiprazole for the treatment of adults with acute schizophrenia. Schizophr Res 164:127–135
Kay SR, Fiszbein A, Opler LA (1987) The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull 13:261–276
Kishi T, Oya K, Matsui Y, Nomura I, Sakuma K, Okuya M, Matsuda Y, Fujita K, Funahashi T, Yoshimura R, Iwata N (2018) Comparison of the efficacy and safety of 4 and 2 mg/day brexpiprazole for acute schizophrenia: a meta-analysis of double-blind, randomized placebo-controlled trials. Neuropsychiatr Dis Treat 14:2519–2530
Kishi T, Ikuta T, Matsui Y, Inada K, Matsuda Y, Mishima K, Iwata N (2019) Effect of discontinuation v. maintenance of antipsychotic medication on relapse rates in patients with remitted/stable first-episode psychosis: a meta-analysis. Psychol Med 49:772–779
Kishimoto T, Hagi K, Nitta M, Kane JM, Correll CU (2019) Long-term effectiveness of oral second-generation antipsychotics in patients with schizophrenia and related disorders: a systematic review and meta-analysis of direct head-to-head comparisons. World Psychiatry 18:208–224
Leucht S, Tardy M, Komossa K, Heres S, Kissling W, Salanti G, Davis JM (2012) Antipsychotic drugs versus placebo for relapse prevention in schizophrenia: a systematic review and meta-analysis. Lancet 379:2063–2071
Leucht S, Cipriani A, Spineli L, Mavridis D, Orey D, Richter F, Samara M, Barbui C, Engel RR, Geddes JR, Kissling W, Stapf MP, Lassig B, Salanti G, Davis JM (2013) Comparative efficacy and tolerability of 15 antipsychotic drugs in schizophrenia: a multiple-treatments meta-analysis. Lancet 382:951–962
Leucht S, Leucht C, Huhn M, Chaimani A, Mavridis D, Helfer B, Samara M, Rabaioli M, Bacher S, Cipriani A, Geddes JR, Salanti G, Davis JM (2017) Sixty years of placebo-controlled antipsychotic drug trials in acute schizophrenia: systematic review, Bayesian meta-analysis, and meta-regression of efficacy predictors. Am J Psychiatry 174:927–942
Leucht S, Chaimani A, Leucht C, Huhn M, Mavridis D, Helfer B, Samara M, Cipriani A, Geddes JR, Salanti G, Davis JM (2018) 60years of placebo-controlled antipsychotic drug trials in acute schizophrenia: meta-regression of predictors of placebo response. Schizophr Res 201:315–323
Leucht S, Crippa A, Siafis S, Patel MX, Orsini N, Davis JM (2019) Dose-response meta-analysis of antipsychotic drugs for acute schizophrenia. Am J Psychiatry: appiajp201919010034
Maeda K, Sugino H, Akazawa H, Amada N, Shimada J, Futamura T, Yamashita H, Ito N, McQuade RD, Mork A, Pehrson AL, Hentzer M, Nielsen V, Bundgaard C, Arnt J, Stensbol TB, Kikuchi T (2014) Brexpiprazole I: in vitro and in vivo characterization of a novel serotonin-dopamine activity modulator. J Pharmacol Exp Ther 350:589–604
McEvoy JP, Daniel DG, Carson WH Jr, McQuade RD, Marcus RN (2007) A randomized, double-blind, placebo-controlled, study of the efficacy and safety of aripiprazole 10, 15 or 20 mg/day for the treatment of patients with acute exacerbations of schizophrenia. J Psychiatr Res 41:895–905
Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Bmj 339:b2535
Murray RM, Quattrone D, Natesan S, van Os J, Nordentoft M, Howes O, Di Forti M, Taylor D (2016) Should psychiatrists be more cautious about the long-term prophylactic use of antipsychotics? Br J Psychiatry 209:361–365
NCT00905307 (n.d.) Study to evaluate the efficacy, safety, and tolerability of oral OPC-34712 and aripiprazole for treatment of acute schizophrenia (STEP 203). Clinical Trialsgov
NCT01810380 (n.d.) Brexpiprazole in patients with acute schizophrenia. Clinical Trialsgov
Pillinger T, McCutcheon RA, Vano L, Mizuno Y, Arumuham A, Hindley G, Beck K, Natesan S, Efthimiou O, Cipriani A, Howes OD (2020) Comparative effects of 18 antipsychotics on metabolic function in patients with schizophrenia, predictors of metabolic dysregulation, and association with psychopathology: a systematic review and network meta-analysis. Lancet Psychiatry 7:64–77 PMDA https://www.pmda.go.jp/english/index.html
Potkin SG, Saha AR, Kujawa MJ, Carson WH, Ali M, Stock E, Stringfellow J, Ingenito G, Marder SR (2003) Aripiprazole, an antipsychotic with a novel mechanism of action, and risperidone vs placebo in patients with schizophrenia and schizoaffective disorder. Arch Gen Psychiatry 60:681–690
Salanti G, Higgins JP, Ades AE, Ioannidis JP (2008) Evaluation of networks of randomized trials. Stat Methods Med Res 17:279–301
Simon V, van Winkel R, De Hert M (2009) Are weight gain and metabolic side effects of atypical antipsychotics dose dependent? A literature review. J Clin Psychiatry 70:1041–1050
van Valkenhoef G, Lu G, de Brock B, Hillege H, Ades AE, Welton NJ (2012) Automating network meta-analysis. Res Synth Methods 3:285–299
Acknowledgments
We thank Otsuka Pharmaceutical Co., Ltd. (Tokyo, Japan 〒101-8535) for providing unpublished information and data for this study.
Author information
Authors and Affiliations
Contributions
Dr. Kishi had full access to all of the data in the study and takes full responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design, analysis, and interpretation of data: T. Kishi.
Statistical analysis: T. Kishi and T. Ikuta.
Acquisition of data: T. Kishi, Y. Matsuda, and K. Sakuma.
Drafting of the manuscript: All of the authors.
Study supervision: N. Iwata.
Corresponding author
Ethics declarations
Conflict of interest
The authors have declared that there are no potential conflicts of interest in relation to the subject of this study. We have had the following interests within the last 3 years.
Dr. Kishi has received speaker’s honoraria from Daiichi Sankyo, Dainippon Sumitomo, Eisai, Eli Lilly, Janssen, Kyowa, Otsuka, Pfizer, Meiji, MSD, Sumitomo Pharmaceuticals (Suzhou), Yoshitomi, and Tanabe-Mitsubishi and has received a Health Labour Sciences Research Grant, Grant-in-Aid for Scientific Research (C), and a Fujita Health University School of Medicine research grant.
Dr. Ikuta received speaker’s honoraria from Eli Lilly, Daiichi Sankyo, and Dainippon Sumitomo and is a consultant for Dainippon Sumitomo.
Dr. Matsuda has received speaker’s honoraria from Dainippon Sumitomo, Eisai, Otsuka, Tanabe-Mitsubishi, and Pfizer and has received a grant-in-aid for Young Scientists (B).
Dr. Sakuma has received speaker’s honoraria from Eisai, Kissei, Meiji, Otsuka, and Torii and has received a grant-in-aid for Young Scientists (B).
Dr. Iwata has received speaker’s honoraria from Astellas, Dainippon Sumitomo, Eli Lilly, GlaxoSmithKline, Janssen, Yoshitomi, Otsuka, Meiji, Shionogi, Novartis, and Pfizer and has received research grants from Daiichi Sankyo, Dainippon Sumitomo, Meiji, and Otsuka.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kishi, T., Ikuta, T., Matsuda, Y. et al. Aripiprazole vs. brexpiprazole for acute schizophrenia: a systematic review and network meta-analysis. Psychopharmacology 237, 1459–1470 (2020). https://doi.org/10.1007/s00213-020-05472-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00213-020-05472-5