Abstract
Summary
This study presents the clinical and biochemical profiles of patients with PHPT between 2005 and 2016 at our center. Most PHPT patients in China show symptomatic features. The number of symptomatic and asymptomatic patients increased during that time, and the number of individuals with parathyroid carcinoma is now increasing.
Introduction
Over the last decade, the prevalence of primary hyperparathyroidism (PHPT) has increased sharply, and the number of individuals with parathyroid cancer is still trending upward. Little is known about the clinical outlook of the disease over the last decade in China. The aim of this study was to describe the clinical characteristics of PHPT patients at our center from January 2005 to December 2016.
Methods
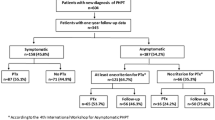
Two hundred sixty patients with PHPT visiting Shanghai Jiao Tong University Affiliated Sixth People’s Hospital were enrolled retrospectively. The clinical manifestations and biochemical abnormalities of these patients were analyzed.
Results
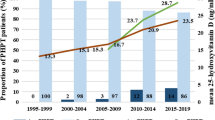
Among all patients, 73.1% had symptomatic PHPT, while the number of symptomatic and asymptomatic patients increased 1 to 2.5 times and 1.5 to 3 times, respectively, from 2005 to 2016. Bone pain and single adenoma were the most frequent signs and pathological results. The patients with parathyroid carcinoma over the last 5 years accounted for 90% (9/10) of all parathyroid carcinoma patients from 2005 to 2016, and parathyroid carcinoma patients had higher levels of serum calcium, parathyroid hormone (PTH), and serum creatinine (P < 0.05) than parathyroid hyperplasia and parathyroid adenoma patients.
Conclusions
Most patients with PHPT in China still exhibit classic clinical and biochemical features. Both symptomatic and asymptomatic patients have increased over the last 12 years. Although the proportion of parathyroid carcinoma was small, a noticeable upward tendency was observed at our center.

Similar content being viewed by others
References
Marcocci C, Cetani F (2011) Clinical practice. Primary hyperparathyroidism. N Engl J Med 365(25):2389–2397. https://doi.org/10.1056/NEJMcp1106636
Fraser WD (2009) Hyperparathyroidism. Lancet 374(9684):145–158. https://doi.org/10.1016/S0140-6736(09)60507-9
Bilezikian JP, Silverberg SJ (2004) Clinical practice. Asymptomatic primary hyperparathyroidism. N Engl J Med 350(17):1746–1751. https://doi.org/10.1056/NEJMcp032200
Pallauf A, Schopohl J, Makeschin M, Kirchner T, Reincke M (2015) Lethal generalized calcinosis and hypercalcemic crisis in primary hyperparathyroidism. J Clin Endocrinol Metab 100(1):17–18. https://doi.org/10.1210/jc.2014-2813
Larian B, Alavi S, Roesler J, Namazie A, Blackwell K, Calcaterra TC, Wang MB (2001) The role of hyperplasia in multiple parathyroid adenomas. Head Neck 23(2):134–139. https://doi.org/10.1002/1097-0347(200102)23:2<134::AID-HED1008>3.0.CO;2-J
Arnold A, Staunton CE, Kim HG, Gaz RD, Kronenberg HM (1988) Monoclonality and abnormal parathyroid hormone genes in parathyroid adenomas. N Engl J Med 318(11):658–662. https://doi.org/10.1056/nejm198803173181102
Bilezikian JP, Brandi ML, Eastell R, Silverberg SJ, Udelsman R, Marcocci C, Potts JT Jr (2014) Guidelines for the management of asymptomatic primary hyperparathyroidism: summary statement from the fourth international workshop. J Clin Endocrinol Metab 99(10):3561–3569. https://doi.org/10.1210/jc.2014-1413
Zhao L, Liu JM, He XY, Zhao HY, Sun LH et al (2013) The changing clinical patterns of primary hyperparathyroidism in Chinese patients: data from 2000 to 2010 in a single clinical center. J Clin Endocrinol Metab 98(2):721–728. https://doi.org/10.1210/jc.2012-2914
Yeh MW, Ituarte PH, Zhou HC, Nishimoto S, Liu IL (2013) Incidence and prevalence of primary hyperparathyroidism in a racially mixed population. J Clin Endocrinol Metab 98(3):1122–1129. https://doi.org/10.1210/jc. 2012-4022
Walker MD, Cong E, Lee JA, Kepley A, Zhang C, McMahon DJ, Silverberg SJ (2015) Vitamin D in primary hyperparathyroidism: effects on clinical, biochemical, and densitometric presentation. J Clin Endocrinol Metab 100(9):3443–3451. https://doi.org/10.1210/jc.2015-2022
Ahsan T, Erum U, Inam Pal KM, Jabeen R, Qureeshi SG, Rehman UL, Banu Z (2017) The many guises of primary hyperparathyroidism: an unchanged scenario. J Pak Med Assoc 67(4):580–585
Castellano E, Tassone F, Attanasio R, Gianotti L, Pellegrino M, Borretta G (2016) Primary hyperparathyroidism as defined in the Italian Society of Endocrinology’s Consensus Statement: prevalence and clinical features. J Endocrinol Investig 39(3):349–354. https://doi.org/10.1007/s40618-015-0412-6
Usta A, Alhan E, Cinel A, Turkyilmaz S, Erem C (2015) A 20-year study on 190 patients with primary hyperparathyroidism in a developing country: Turkey experience. Int Surg 100(4):648–655. https://doi.org/10.9738/INTSURG-D-14-00094.1
Tannenbaum C, Clark J, Schwartzman K, Wallenstein S, Lapinski R, Meier D, Luckey M (2002) Yield of laboratory testing to identify secondary contributors to osteoporosis in otherwise healthy women. J Clin Endocrinol Metab 87(10):4431–4437. https://doi.org/10.1210/jc.2002-020275
Ghosh S, Collier A, Clark D, Storey C, Malik I (2010) Social deprivation and primary hyperparathyroidism. Endocr Pract 16(6):982–985. https://doi.org/10.4158/EP09331.OR
Glenn JA, Yen TW, Javorsky BR, Rose BG, Carr AA et al (2016) Association between body mass index and multigland primary hyperparathyroidism. J Surg Res 202(1):132–138. https://doi.org/10.1016/j.jss.2015.12.05
Varshney S, Bhadada SK, Saikia UN, Sachdeva N, Behera A, Arya AK, Sharma S, Bhansali A, Mithal A, Rao SD (2013) Simultaneous expression analysis of vitamin D receptor, calcium-sensing receptor, cyclin D1, and PTH in symptomatic primary hyperparathyroidism in Asian Indians. Eur J Endocrinol 169(1):109–116. https://doi.org/10.1530/EJE-13-0085
Carsote M, Paduraru DN, Nica AE, Valea A (2016) Parathyroidectomy: is vitamin D a player for a good outcome? J Med Life 9(4):348–352
Walker MD, Saeed I, Lee JA, Zhang C, Hans D, Lang T, Silverberg SJ (2016) Effect of concomitant vitamin D deficiency or insufficiency on lumbar spine volumetric bone mineral density and trabecular bone score in primary hyperparathyroidism. Osteoporos Int 27(10):3063–3071. https://doi.org/10.1007/s00198-016-3637-0
Viccica G, Cetani F, Vignali E, Miccoli M, Marcocci C (2017) Impact of vitamin D deficiency on the clinical and biochemical phenotype in women with sporadic primary hyperparathyroidism. Endocrine 55(1):256–265. https://doi.org/10.1007/s12020-016-0931-8
Ryhanen EM, Leijon H, Metso S, Eloranta E, Korsoff P et al (2017) A nationwide study on parathyroid carcinoma. Acta Oncol 56(7):1–13. https://doi.org/10.1080/0284186X.2017.1306103
Lee PK, Jarosek SL, Virnig BA, Evasovich M, Tuttle TM (2007) Trends in the incidence and treatment of parathyroid cancer in the United States. Cancer 109(9):1736–1741. https://doi.org/10.1002/cncr.22599
Goswamy J, Lei M, Simo R (2016) Parathyroid carcinoma. Curr Opin Otolaryngol Head Neck Surg 24(2):155–162. https://doi.org/10.1097/MOO.0000000000000234
Brown S, O'Neill C, Suliburk J, Sidhu S, Sywak M, Gill A, Robinson B, Delbridge L (2011) Parathyroid carcinoma: increasing incidence and changing presentation. ANZ J Surg 81(7-8):528–532. https://doi.org/10.1111/j.1445-2197.2010.05594.x
Stern S, Mizrachi A, Strenov Y, Knaanie A, Benbassat C, Shpitzer T, Bachar G (2017) Parathyroid adenoma: a comprehensive biochemical and histological correlative study. Clin Otolaryngol 42(2):381–386. https://doi.org/10.1111/coa.12761
Inic Z, Inic M, Jancic S, Paunovic I, Tatic S, Tausanovic K, Zivavljevic V, Zegarac M, Inic I, Dunjdjerovic D (2015) The relationship between proliferation activity and parathyroid hormone levels in parathyroid tumors. J BUON 20(2):562–566
Funding
This study was funded by the National Natural Science Foundational of China (81670718).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Ethical approval
Scientific approval was obtained from the SIDIAP Scientific Committee, and ethics approval was granted by the relevant board (CEIC IDIAP Jordi Gol). All procedures performed in the studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
For this type of study, formal consent was not required.
Rights and permissions
About this article
Cite this article
Sun, B., Guo, B., Wu, B. et al. Characteristics, management, and outcome of primary hyperparathyroidism at a single clinical center from 2005 to 2016. Osteoporos Int 29, 635–642 (2018). https://doi.org/10.1007/s00198-017-4322-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-017-4322-7