Abstract
Summary
We examined cross-sectional associations of metabolic syndrome and its components with male bone turnover, density and structure. Greater bone mass in men with metabolic syndrome was related to their greater body mass, whereas hyperglycaemia, hypertriglyceridaemia or impaired insulin sensitivity were associated with lower bone turnover and relative bone mass deficits.
Introduction
Metabolic syndrome (MetS) has been associated with lower bone turnover and relative bone mass or strength deficits (i.e. not proportionate to body mass index, BMI), but the relative contributions of MetS components related to insulin sensitivity or obesity to male bone health remain unclear.
Methods
We determined cross-sectional associations of MetS, its components and insulin sensitivity (by homeostatic model assessment-insulin sensitivity (HOMA-S)) using linear regression models adjusted for age, centre, smoking, alcohol, and BMI. Bone turnover markers and heel broadband ultrasound attenuation (BUA) were measured in 3129 men aged 40–79. Two centres measured total hip, femoral neck, and lumbar spine areal bone mineral density (aBMD, n = 527) and performed radius peripheral quantitative computed tomography (pQCT, n = 595).
Results
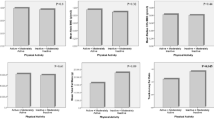
MetS was present in 975 men (31.2 %). Men with MetS had lower β C-terminal cross-linked telopeptide (β-CTX), N-terminal propeptide of type I procollagen (PINP) and osteocalcin (P < 0.0001) and higher total hip, femoral neck, and lumbar spine aBMD (P ≤ 0.03). Among MetS components, only hypertriglyceridaemia and hyperglycaemia were independently associated with PINP and β-CTX. Hyperglycaemia was negatively associated with BUA, hypertriglyceridaemia with hip aBMD and radius cross-sectional area (CSA) and stress–strain index. HOMA-S was similarly associated with PINP and β-CTX, BUA, and radius CSA in BMI-adjusted models.
Conclusions
Men with MetS have higher aBMD in association with their greater body mass, while their lower bone turnover and relative deficits in heel BUA and radius CSA are mainly related to correlates of insulin sensitivity. Our findings support the hypothesis that underlying metabolic complications may be involved in the bone’s failure to adapt to increasing bodily loads in men with MetS.
Similar content being viewed by others
References
Alberti KG, Eckel RH, Grundy SM et al (2009) Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation 120:1640–1645
Reaven GM (2011) Insulin resistance: the link between obesity and cardiovascular disease. Med Clin North Am 95:875–892
von Muhlen D, Safii S, Jassal SK, Svartberg J, Barrett-Connor E (2007) Associations between the metabolic syndrome and bone health in older men and women: the Rancho Bernardo Study. Osteoporos Int 18:1337–1344
Kinjo M, Setoguchi S, Solomon DH (2007) Bone mineral density in adults with the metabolic syndrome: analysis in a population-based U.S. sample. J Clin Endocrinol Metab 92:4161–4164
Szulc P, Varennes A, Delmas PD, Goudable J, Chapurlat R (2010) Men with metabolic syndrome have lower bone mineral density but lower fracture risk—the MINOS study. J Bone Miner Res 25:1446–1454
Hernandez JL, Olmos JM, Pariente E, Martinez J, Valero C, Garcia-Velasco P, Nan D, Llorca J, Gonzalez-Macias J (2010) Metabolic syndrome and bone metabolism: the Camargo Cohort study. Menopause 17:955–961
Esposito K, Chiodini P, Capuano A, Colao A, Giugliano D (2013) Fracture risk and bone mineral density in metabolic syndrome: a meta-analysis. J Clin Endocrinol Metab 98:3306–3314
Vanderschueren D, Laurent MR, Claessens F, Gielen E, Lagerquist MK, Vandenput L, Borjesson AE, Ohlsson C (2014) Sex steroid actions in male bone. Endocr Rev 35:906–960
Muka T, Trajanoska K, Kiefte-de Jong JC et al (2015) The association between metabolic syndrome, bone mineral density, hip bone geometry and fracture risk: the Rotterdam Study. PLoS One 10:e0129116
Evans AL, Paggiosi MA, Eastell R, Walsh JS (2015) Bone density, microstructure and strength in obese and normal weight men and women in younger and older adulthood. J Bone Miner Res 30:920–928
Schwartz AV, Vittinghoff E, Bauer DC et al (2011) Association of BMD and FRAX score with risk of fracture in older adults with type 2 diabetes. JAMA 305:2184–2192
Johansson H, Kanis JA, Oden A et al (2014) A meta-analysis of the association of fracture risk and body mass index in women. J Bone Miner Res 29:223–233
Chan MY, Frost SA, Center JR, Eisman JA, Nguyen TV (2014) Relationship between body mass index and fracture risk is mediated by bone mineral density. J Bone Miner Res 29:2327–2335
Farr JN, Drake MT, Amin S, Melton LJ 3rd, McCready LK, Khosla S (2014) In vivo assessment of bone quality in postmenopausal women with type 2 diabetes. J Bone Miner Res 29:787–795
Yu EW, Putman MS, Derrico N, Abrishamanian-Garcia G, Finkelstein JS, Bouxsein ML (2015) Defects in cortical microarchitecture among African-American women with type 2 diabetes. Osteoporos Int 26:673–679
Shen J, Nielson CM, Marshall LM, Lee DC, Keaveny TM, Orwoll ES (2015) The association between BMI and QCT-derived proximal hip structure and strength in older men: a cross-sectional study. J Bone Miner Res 30:1301–1308
Ishii S, Cauley JA, Greendale GA, Nielsen C, Karvonen-Gutierrez C, Ruppert K, Karlamangla AS (2014) Pleiotropic effects of obesity on fracture risk: the Study of Women’s Health Across the Nation. J Bone Miner Res 29:2561–2570
Lee DM, Pye SR, Tajar A et al (2013) Cohort profile: the European Male Ageing Study. Int J Epidemiol 42:391–401
Boonen S, Pye SR, O’Neill TW et al (2011) Influence of bone remodelling rate on quantitative ultrasound parameters at the calcaneus and DXA BMDa of the hip and spine in middle-aged and elderly European men: the European Male Ageing Study (EMAS). Eur J Endocrinol 165:977–986
Vanderschueren D, Pye SR, O’Neill TW et al (2013) Active vitamin D (1,25-dihydroxyvitamin D) and bone health in middle-aged and elderly men: the European Male Aging Study (EMAS). J Clin Endocrinol Metab 98:995–1005
Rosenquist C, Qvist P, Bjarnason N, Christiansen C (1995) Measurement of a more stable region of osteocalcin in serum by ELISA with two monoclonal antibodies. Clin Chem 41:1439–1445
Levy JC, Matthews DR, Hermans MP (1998) Correct homeostasis model assessment (HOMA) evaluation uses the computer program. Diabetes Care 21:2191–2192
Katz A, Nambi SS, Mather K, Baron AD, Follmann DA, Sullivan G, Quon MJ (2000) Quantitative insulin sensitivity check index: a simple, accurate method for assessing insulin sensitivity in humans. J Clin Endocrinol Metab 85:2402–2410
Ward KA, Pye SR, Adams JE et al (2011) Influence of age and sex steroids on bone density and geometry in middle-aged and elderly European men. Osteoporos Int 22:1513–1523
Antonio L, Wu FC, O’Neill TW et al (2015) Associations between sex steroids and the development of metabolic syndrome: a longitudinal study in European Men. J Clin Endocrinol Metab 100:1396–1404
Miller CG, Herd RJ, Ramalingam T, Fogelman I, Blake GM (1993) Ultrasonic velocity measurements through the calcaneus: which velocity should be measured? Osteoporos Int 3:31–35
Yeap BB, Chubb SA, Flicker L, McCaul KA, Ebeling PR, Beilby JP, Norman PE (2010) Reduced serum total osteocalcin is associated with metabolic syndrome in older men via waist circumference, hyperglycemia, and triglyceride levels. Eur J Endocrinol 163:265–272
Yusuf E (2012) Metabolic factors in osteoarthritis: obese people do not walk on their hands. Arthritis Res Ther 14:123
Clemens TL, Karsenty G (2011) The osteoblast: an insulin target cell controlling glucose homeostasis. J Bone Miner Res 26:677–680
Parajuli A, Liu C, Li W et al. Bone’s responses to mechanical loading are impaired in type 1 diabetes. Bone 81:152–160
Yeap BB, Alfonso H, Paul Chubb SA et al (2014) Higher serum undercarboxylated osteocalcin and other bone turnover markers are associated with reduced diabetes risk and lower estradiol concentrations in older men. J Clin Endocrinol Metab 100:63–71
Confavreux CB, Szulc P, Casey R, Varennes A, Goudable J, Chapurlat RD (2014) Lower serum osteocalcin is associated with more severe metabolic syndrome in elderly men from the MINOS cohort. Eur J Endocrinol 171:275–283
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Funding
The European Male Ageing Study was funded by the Commission of the European Communities Fifth Framework Programme, Quality of Life and Management of Living Resources, Grant QLK6-CT-2001-00258, by Arthritis Research UK, by the Research Foundation Flanders grants G.0171.03 and G.0854.13N and KU Leuven grant GOA/15/017. This report includes independent research supported by the UK National Institute for Health Research Biomedical Research Unit Funding Scheme. The views expressed in this publication are those of the author(s) and not necessarily those of the NHS, the National Institute for Health Research or the Department of Health. The work of K.A.W. was conducted within the core programme of the MRC Nutrition and Bone Health Group at MRC Human Nutrition Research, funded by the UK Medical Research Council (Programme number U105960371). M.R.L. is a PhD Fellow of the Research Foundation Flanders. D.V. is a senior clinical investigator supported by the Clinical Research Fund of the University Hospitals Leuven, Belgium.
Conflicts of interest
All authors have completed the ICMJE uniform disclosure form at http://www.icmje.org/coi_disclosure.pdf and declare the following: Dr. Laurent has received lecture fees from Flanders’ Agricultural Marketing Board (VLAM) and reports consultancy for Novartis and Alexion. Dr. Huhtaniemi has consulted for and/or received research funding from Ferring, Novartis and Takeda. Dr. Wu has consulted for Besins Healthcare and Repros Inc., and received research funding from Besins Healthcare and Bayer Schering. All other authors declare that they have no conflict of interest.
Additional information
The European Male Ageing Study (EMAS) Group: The principal investigator of EMAS is Prof. F. C. W. Wu. Participating centres: Florence (Gianni Forti, Luisa Petrone, Giovanni Corona); Leuven (Dirk Vanderschueren, Steven Boonen (deceased), Herman Borghs); Łódź (Krzysztof Kula, Jolanta Slowikowska-Hilczer, Renata Walczak-Jedrzejowska); London (Ilpo Huhtaniemi); Malmö (Aleksander Giwercman); Manchester (Frederick C.W. Wu, Alan J. Silman, Terence W. O’Neill, Joseph D. Finn, Philip Steer, Abdelouahid Tajar, David M. Lee, Stephen R. Pye); Santiago de Compostela (Felipe Casanueva, Mary Lage, Ana I Castro); Szeged (György Bartfai, Imre Földesi, Imre Fejes); Tartu (Margus Punab, Paul Korrovitz); and Turku (Min Jiang)
M. R. Laurent, M. J. Cook, S. R. Pye and T. W. O’Neill contributed equally to this work.
Rights and permissions
About this article
Cite this article
Laurent, M.R., Cook, M.J., Gielen, E. et al. Lower bone turnover and relative bone deficits in men with metabolic syndrome: a matter of insulin sensitivity? The European Male Ageing Study. Osteoporos Int 27, 3227–3237 (2016). https://doi.org/10.1007/s00198-016-3656-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-016-3656-x