Abstract
Introduction and hypothesis
Pelvic organ prolapse is a common problem affecting women, but there is currently a lack of research focusing on patient experience of pessary changes. This study was aimed at capturing the patient perspective of pessary changes and formally assessing pain during pessary removal and insertion.
Methods
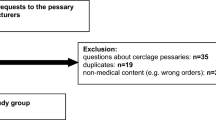
A service evaluation request was granted by South Tees Hospitals NHS Trust. Patients undergoing pessary change (ring, shelf, or Gellhorn) in gynaecology outpatient clinics over a 6-month period were asked to rate their pain scores on a ten-point numerical pain-rating scale. Other associated data were collected.
Results
Out of 213 women, 58.2% reported that pessary removal was more painful than insertion, 30.5% reported equal pain, and 10.8% reported that insertion was more painful than removal. Pain scores were significantly higher for removal (mean 4.37, median 4, IQR 4–7) than for insertion (mean 2.66, median 2, IQR 2–4, p <0.001). Ring pessaries were significantly less painful to both remove and insert than shelf and Gellhorn pessaries. Smaller pessaries were more painful to both remove and insert. There was no significant difference in pain scores reported by those with or without diagnosed vulval conditions.
Conclusions
Pessary removal causes most women moderate pain, which should be communicated to patients beforehand. Ring pessaries are significantly less painful to change than other pessary types. Clinicians should consider pain as a factor in their decision-making surrounding pessary choice and when counselling patients. Future research should focus on ways to reduce pain during pessary removal.


Similar content being viewed by others
Abbreviations
- HRT:
-
Hormone replacement therapy
- NRS:
-
Numerical rating scale
- POP:
-
Pelvic organ prolapse
References
Bugge C, Adams EJ, Gopinath D, et al. Pessaries (mechanical devices) for managing pelvic organ prolapse in women. Cochrane Database Syst Rev. 2020;11(11):CD004010. https://doi.org/10.1002/14651858.CD004010.pub4.
Smith TA, Poteat TA, Shobeiri SA. Pelvic organ prolapse: an overview. JAAPA. 2014;27(3):20–4; quiz 33. https://doi.org/10.1097/01.JAA.0000443963.00740.4d.
Hendrix SL, Clark A, Nygaard I, Aragaki A, Barnabei V, McTiernan A. Pelvic organ prolapse in the Women's Health Initiative: gravity and gravidity. Am J Obstet Gynecol. 2002;186(6):1160–6. https://doi.org/10.1067/mob.2002.123819.
Abdel-Fattah M, Familusi A, Fielding S, Ford J, Bhattacharya S. Primary and repeat surgical treatment for female pelvic organ prolapse and incontinence in parous women in the UK: a register linkage study. BMJ Open. 2011;1(2):e000206. https://doi.org/10.1136/bmjopen-2011-000206.
Cundiff GW, Weidner AC, Visco AG, Bump RC, Addison WA. A survey of pessary use by members of the American Urogynecologic Society. Obstet Gynecol. 2000;95(6 Pt 1):931–5. https://doi.org/10.1016/s0029-7844(00)00788-2.
Palumbo MV. Pessary placement and management. Ostomy Wound Manage. 2000;46(12):40–5.
Badri H. Tips & tricks: vaginal pessary insertion & removal techniques. IUGA Spotlight. 2020.
National Institute for Health and Care Excellence (NICE). Urinary incontinence and pelvic organ prolapse in women: management. NICE Guideline. 2019;NG123.
de Albuquerque Coelho SC, Brito LGO, de Araujo CC, Juliato CRT. Factors associated with unsuccessful pessary fitting in women with symptomatic pelvic organ prolapse: systematic review and metanalysis. Neurourol Urodyn. 2020;39(7):1912–21. https://doi.org/10.1002/nau.24458.
Sarma S, Ying T, Moore KH. Long-term vaginal ring pessary use: discontinuation rates and adverse events. BJOG. 2009;116(13):1715–21. https://doi.org/10.1111/j.1471-0528.2009.02380.x.
Moore KH, Lammers K, Allen W, Parkin K, Te West N. Does monthly self-management of vaginal ring pessaries reduce the rate of adverse events? A clinical audit. Eur J Obstet Gynecol Reprod Biol. 2022;16:100164. https://doi.org/10.1016/j.eurox.2022.100164.
Taege SK, Adams W, Mueller ER, Brubaker L, Fitzgerald CM, Brincat C. Anesthetic cream use during office pessary removal and replacement: a randomized controlled trial. Obstet Gynecol. 2017;130(1):190–7. https://doi.org/10.1097/aog.0000000000002098.
Chiengthong K, Ruanphoo P, Chatsuwan T, Bunyavejchevin S. Effect of vaginal estrogen in postmenopausal women using vaginal pessary for pelvic organ prolapse treatment: a randomized controlled trial. Int Urogynecol J. 2022;33(7):1833–8. https://doi.org/10.1007/s00192-021-04821-y.
Dessie SG, Armstrong K, Modest AM, Hacker MR, Hota LS. Effect of vaginal estrogen on pessary use. Int Urogynecol J. 2016;27(9):1423–9. https://doi.org/10.1007/s00192-016-3000-1.
Bulchandani S, Toozs-Hobson P, Verghese T, Latthe P. Does vaginal estrogen treatment with support pessaries in vaginal prolapse reduce complications? Post Reprod Health. 2015;21(4):141–5. https://doi.org/10.1177/2053369115614704.
De Albuquerque Coelho SC, Giraldo PC, Brito LGO, Juliato CRT. ESTROgen use for complications in women treating pelvic organ prolapse with vaginal PESSaries (ESTRO-PESS)—a randomized clinical trial. Int Urogynecol J. 2021;32(6):1571–8. https://doi.org/10.1007/s00192-020-04654-1.
Baranidharan GWA, Wilson S, Cameron P, Tan T. Outcome measures. Faculty of Pain Medicine of the Royal College of Anaesthetists. 2019.
Harvard. The pain of measuring pain. 2018. Available from: https://www.health.harvard.edu/pain/the-pain-of-measuring-pain. Accessed 11/5/2023
Acknowledgements
We wish to acknowledge Sister Colette Anderson, Sister Karla Kennedy and registered nurses Linda Rozsas and Jenny Hill, who deliver pessary clinic care and assisted in data collection. We wish to thank all patients who took the time to complete the service evaluation questionnaire.
Author information
Authors and Affiliations
Contributions
C. Renouf: project development, data collection, data analysis, manuscript writing and editing; P. Ballard: project development, data collection, data analysis and manuscript editing; A. Khunda: data collection, data analysis and manuscript editing; V. Kershaw: manuscript editing; S. Shawer: manuscript editing; J. Rees: data analysis and manuscript editing.
Corresponding author
Ethics declarations
Conflicts of interest
Aethele Khunda has received educational grants from Medtronic, Axonic, Olympus and international conference organising committees. Victoria Kershaw has received educational grants to attend courses from Medtronic and Olympus. The other authors declare that they have no conflicts of interest.
Informed consent
Written informed consent was obtained from the patient for publication of this original article.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix 1: Proforma questionnaire
Appendix 1: Proforma questionnaire
-
1.
Are you using any vaginal HRT: No/Oestrogen cream/Vagifem (please circle)
-
2.
If yes, how often: Once a week/Twice a week/Other (please circle or write)
-
3.
Have you been diagnosed with a specific vulval skin condition: No/Lichen sclerosus/Other
-
4.
a. Is this your first pessary change: Yes/No. b. How long have you used pessaries for? (years)
-
5.
How painful did you find the removal of your ring/shelf/Gellhorn pessary (on a 0–10 scale): 0 = no pain, 10 = worse pain, like labour pain
-
6.
Size of the removed pessary
-
7.
Trauma to the perineum: No/Yes, estimated size of tear (mm)
-
8.
How painful did you find the (re-)insertion of your pessary (on a 0–10 scale): 0 = no pain, 10 = worse pain, like labour pain
-
9.
Size of the newly inserted ring/shelf/Gellhorn pessary
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Renouf, C., Ballard, P., Khunda, A. et al. Patient experience of pain during vaginal pessary removal and insertion: a service evaluation study. Int Urogynecol J 35, 327–332 (2024). https://doi.org/10.1007/s00192-023-05643-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-023-05643-w