Abstract
Objectives
Our primary objective was to determine rectal prolapse (RP) and pelvic organ prolapse (POP) reoperation rates and postoperative < 30-day complications after combined RP and POP surgery at a single institution.
Methods
This was an IRB-approved retrospective cohort study of all female patients who received combined RP and POP surgery at a single tertiary care center from 2008 to 2019. Recurrence was defined as the need for subsequent repeat RP or POP surgery at any point after the index surgery. Surgical complications were separated into Clavien-Dindo classes.
Results
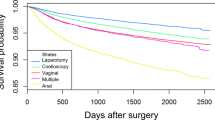
Sixty-three patients were identified, and 18.3% (12/63) had < 30-day complications (55% Clavien-Dindo grade 1; 27% Clavien-Dindo grade 2; 18% Clavien-Dindo grade 4). Of patients undergoing combined abdominal RP and POP repair, no postoperative < 30-day complications were noted in the MIS group compared to 37.5% of those patients in the laparotomy group (p < 0.01). Overall, in those patients who underwent combined RP and POP surgery, the need for subsequent RP surgery for recurrent RP was 14% and the need for subsequent POP surgery for recurrent POP was 4.8% (p = 0.25).
Conclusion
In this cohort of women undergoing combined RP and POP surgery, a higher proportion required subsequent RP surgery compared to those requiring subsequent POP surgery, although this was not statistically significant. Almost one-fifth of patients undergoing combined RP and POP surgery experienced a < 30-day surgical complication, regardless of whether the approach was perineal or abdominal. For those patients undergoing abdominal repair, < 30-day complications were more likely in those patients who had a laparotomy compared to those who had a minimally invasive surgery.

Similar content being viewed by others
References
Felt-Bersma RJ, Tiersma ES, Cuesta MA. Rectal prolapse, rectal intussusception, rectocele, solitary rectal ulcer syndrome, and enterocele. Gastroenterol Clin N Am. 2008;37(3):645–68.
Cannon JA. Evaluation, diagnosis, and medical management of rectal prolapse. Clin Colon Rectal Surg. 2017;30(1):16–21.
Tou S, Brown SR, Nelson RL. Surgery for complete rectal prolapse in adults. Cochrane Database Syst Rev. 2015;24(11):CD001758.
Bump RC, Mattiasson A, Bø K, et al. The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol. 1996;175(1):10–7.
Jelovsek JE, Maher C, Barber MD. Pelvic organ prolapse. Lancet. 2007;369(9566):1027–38.
Hagen S, Stark D. Conservative prevention and management of pelvic organ prolapse in women. Cochrane Database Syst Rev. 2011;07(12):CD003882.
Altman D, Zetterstrom J, Schultz I, et al. Pelvic organ prolapse and urinary incontinence in women with surgically managed rectal prolapse: a population-based case-control study. Dis Colon Rectum. 2006;49:28–35.
Jallad K, Gurland B. Multidisciplinary approach to the treatment of concomitant rectal and vaginal prolapse. Clin Colon Rectal Surg. 2016;29(2):101–5.
Jallad K, Ridgeway B, Paraiso MF, et al. Long-term outcomes after ventral rectopexy with sacrocolpo- or hysteropexy for the treatment of concurrent rectal and pelvic organ prolapse. Female Pelvic Med Reconstr Surg. 2018;24(5):336–40.
Unger CA, Paraiso MFR, Jelovsek JE, et al. Perioperative adverse events after minimally invasive abdominal sacrocolpopexy. Am J Obstet Gynecol. 2014;211:547.e1–2.
VanderPas Lamb S, Massengill J, et al. Safety of combined abdominal sacral colpopexy and sigmoid resection with suture rectopexy. Female Pelvic Med Reconstr Surg. 2015;21(1):18–24.
Geltzeiler C, Birnbaum E, Silviera M, et al. Combined rectopexy and sacrocolpopexy is safe for correction of pelvic organ prolapse. Int J Color Dis. 2018;33(10):1453–9.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240(2):205–13.
Senapati A, Gray RG, Middleton LJ, et al. PROSPER: a randomised comparison of surgical treatments for rectal prolapse. Color Dis. 2013 Jul;15(7):858–68.
Emile SH, Elfeki H, Shalaby M, et al. Outcome of laparoscopic ventral mesh rectopexy for full-thickness external rectal prolapse: a systematic review, meta-analysis, and meta-regression analysis of the predictors for recurrence. Surg Endosc. 2019;33(8):2444–55.
Jelovsek JE, Barber MD, Brubaker L, et al. Effect of uterosacral ligament suspension vs sacrospinous ligament fixation with or without perioperative behavioral therapy for pelvic organ vaginal prolapse on surgical outcomes and prolapse symptoms at 5 years in the OPTIMAL randomized clinical trial. JAMA. 2018;319(15):1554–65.
Siddiqui NY, Grimes CL, Casiano ER, et al. Mesh sacrocolpopexy compared with native tissue vaginal repair: a systematic review and meta-analysis. Obstet Gynecol. 2015;125(1):44–55.
Kim DS, Tsang CB, Wong WD, Lowry AC, Goldberg SM, Madoff RD. Complete rectal prolapse: evolution of management and results. Dis Colon Rectum. 1999;42(4):460–9.
Madiba TE, Baig MK, Wexner SD. Surgical management of rectal prolapse. Arch Surg. 2005;140(1):63–73.
Campbell P, Cloney L, Jha S. Abdominal versus laparoscopic sacrocolpopexy: a systematic review and meta-analysis. Obstet Gynecol Surv. 2016;71(7):435–42.
Freeman RM, Pantazis K, Thomson A, et al. A randomised controlled trial of abdominal versus laparoscopic sacrocolpopexy for the treatment of post-hysterectomy vaginal vault prolapse: LAS study. Int Urogynecol J. 2013;24(3):377–84.
Author information
Authors and Affiliations
Contributions
SL Wallace: Project development, Data Collection and management, Data analysis, Manuscript writing/editing.
R Syan: Project development, Data Collection and management, Data analysis, Manuscript writing/editing.
EA Enemchukwu: Project development, Data analysis, Manuscript writing/editing.
K Mishra: Project development, Data analysis, Manuscript writing/editing.
E Sokol: Project development, Data analysis, Manuscript writing/editing.
B Gurland: Project development, Data analysis, Manuscript writing/editing.
Corresponding author
Ethics declarations
Conflict of interest
The authors report no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This study was approved by the Stanford Ethics Institutional Review Board (IRB).
Rights and permissions
About this article
Cite this article
Wallace, S.L., Syan, R., Enemchukwu, E.A. et al. Surgical approach, complications, and reoperation rates of combined rectal and pelvic organ prolapse surgery. Int Urogynecol J 31, 2101–2108 (2020). https://doi.org/10.1007/s00192-020-04394-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-020-04394-2