Abstract
Purpose
The aim of this study is to provide a summary of the existing literature on the association between hypotension during intensive care unit (ICU) stay and mortality and morbidity, and to assess whether there is an exposure-severity relationship between hypotension exposure and patient outcomes.
Methods
CENTRAL, Embase, and PubMed were searched up to October 2022 for articles that reported an association between hypotension during ICU stay and at least one of the 11 predefined outcomes. Two independent reviewers extracted the data and assessed the risk of bias. Results were gathered in a summary table and studies designed to investigate the hypotension-outcome relationship were included in the meta-analyses.
Results
A total of 122 studies (176,329 patients) were included, with the number of studies varying per outcome between 0 and 82. The majority of articles reported associations in favor of ‘no hypotension’ for the outcomes mortality and acute kidney injury (AKI), and the strength of the association was related to the severity of hypotension in the majority of studies. Using meta-analysis, a significant association was found between hypotension and mortality (odds ratio: 1.45; 95% confidence interval (CI) 1.12–1.88; based on 13 studies and 34,829 patients), but not for AKI.
Conclusion
Exposure to hypotension during ICU stay was associated with increased mortality and AKI in the majority of included studies, and associations for both outcomes increased with increasing hypotension severity. The meta-analysis reinforced the descriptive findings regarding mortality but did not yield similar support for AKI.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
In this systematic review containing 122 articles (176,329 patients), exposure to hypotension during intensive care unit stay correlated with elevated mortality rates. Furthermore, the majority of the included studies reported associations between hypotension and increased acute kidney injury (AKI) rates, with the strength of the associations intensifying for both outcomes as hypotension severity increased. The associations between hypotension and patient outcomes were especially pronounced when mean arterial pressure fell below 60 mmHg and systolic blood pressure dropped below 90 mmHg for mortality, and when mean arterial pressure dropped below 55 mmHg for AKI. |
Introduction
Maintaining adequate perfusion pressure in vital organs is a pivotal aspect of critical care management. Since bedside tissue perfusion monitoring remains difficult, blood pressure is often used as a surrogate measure. Although continuous blood pressure monitoring is widely used in the intensive care unit (ICU) [1], maintaining normotensive thresholds in the critically ill remains challenging. The reported incidences of hypotension vary widely due to heterogeneity in studied patient populations and hypotension definitions used, thereby complicating study comparison [2,3,4]. Reported definitions differ in the parameter(s) used (e.g., systolic blood pressure [SBP] and mean arterial pressure [MAP]), the type of threshold used (absolute or relative), and the required duration of the pressure drop. Consequently, 140 distinct definitions of hypotension are reported in the literature [5]. However, in the ICU a MAP below 65 mmHg is most frequently used [6].
The relationship between hypotension during the ICU stay and organ damage has been described in numerous, primarily (retrospective) observational, studies [3, 4, 7, 8]. Smischney et al. additionally demonstrated that the strength of this association increased with incremental depth of hypotension, suggesting an exposure–severity relationship between hypotension and patient outcomes [4]. The effect of hypotension during ICU stay on the incidence of hypoperfusion-related complications has not been studied in a randomized clinical trial (RCT) to date. Several RCTs, all with neutral findings, have tested the effect of assigning patients to higher or lower blood pressure targets on mortality or vegetative state [9,10,11]. Notably, in these trials the average blood pressure in the lower blood pressure target groups was above 65 mmHg, and therefore, higher than the commonly used thresholds to define hypotension [6].
Although hypotension has been extensively studied in ICU patients, a summary of available literature outlining patient outcomes affected by hypotension exposure during ICU stay does not exist. Understanding how different definitions of hypotension influence the strength of the associations between hypotension and these outcomes could aid ICU physicians in selecting appropriate blood pressure targets. In this systematic review with meta-analyses, we aim to assess existing literature on the associations between exposure to hypotension during ICU stay and mortality and morbidity. We hypothesize that exposure to hypotension is associated with patient mortality and morbidity, regardless of the studied patient population, and that the strength of this association increases with both decreasing blood pressure thresholds and prolonged exposure to hypotension.
Methods
Systematic review
This systematic review followed the methodology outlined in the Cochrane Handbook for systematic review and PRISMA guidelines. The PRISMA checklist is provided in supplementary Table 1. The study protocol was registered prospectively in the International Prospective Register of Systematic Reviews (PROSPERO) under number CRD42020213244. A clinical librarian helped search PubMed, Embase, and the Cochrane Central Register of Controlled Trials (CENTRAL) for relevant articles up to October 17th 2022. Search terms included medical subject headings (MeSH), free terms, and synonyms for 'intensive care unit,' 'hypotension,' and the outcomes of interest. The complete search strategy is available in supplementary Text 1.
Two independent reviewers screened titles, abstracts, and full texts using the review program Rayyan [12]. Any discrepancies were resolved through discussion with a third reviewer. We included studies in adult patients (> 16 years old) that reported an association between hypotension (as defined by the authors) during ICU stay, and mortality and morbidity, and excluded case reports, literature studies, articles not written in English, and those without full texts or lacking a definition of hypotension. Articles were additionally excluded if the full text or the definition of hypotension could not be obtained despite contacting the authors, if hypotension exposure during procedures (e.g., renal replacement therapy) was studied, or if the sample size was inadequate, defined as less than one event of the outcome of interest in the hypotension or no hypotension group. To avoid overlapping data, we included only the article with the least potential for bias when multiple articles presented findings from the same patient cohort. When the potential for bias was equal, the study with the most frequently used hypotension definition was selected.
Data extraction
Blinded data extraction was performed in duplicate using a predefined template. Subsequently, the data extraction sheets were merged, and in the event of any discrepancies, the original article was re-evaluated. The following data were collected: study design, patient characteristics, hypotension definition, outcome definition, type of blood pressure measurement, and outcome data.
Quality assessment
Prior to conducting the analyses, we critically appraised included articles in duplicate (JaS and BR, SR, or VK) using the Cochrane risk of bias tool for randomized controlled trials [13] and the Newcastle–Ottawa Scale (NOS) for non-randomized studies [14]. The NOS is a grading system with a scale of 0–9 based on four selection criteria, two comparability criteria, and three outcome criteria, with higher scores suggesting a smaller potential for bias. Quality assessors were blinded to each other’s quality assessment.
Objectives
The pre-specified patient outcomes included mortality, acute kidney injury (AKI), myocardial infarction, ischemic cerebrovascular accident (iCVA), delirium, poor cognitive functioning, ICU length of stay, duration of mechanical ventilation, quality of life, post intensive care syndrome (PICS), and World Health Organisation Disability Assessment Schedule (WHODAS) score. We included articles reporting an association between hypotension during ICU stay and at least one of the outcomes mentioned above, regardless of the reported definition of the outcome (e.g., ICU mortality or in-hospital mortality). The primary objective of this systematic review was to provide a descriptive overview of reported associations between exposure to hypotension and the predefined outcomes. Only studies specifically designed to study this relationship, including RCTs and observational studies that conducted a confounder-adjusted analysis to determine an unbiased estimate of the hypotension-outcome association, were used for the primary objective. Secondary objectives were to determine the aggregated direction of the association per patient outcome by pooling the (adjusted) results of individual studies in a meta-analysis, to assess whether there is an exposure-severity relationship between hypotension exposure and patient outcomes within studies that compared multiple levels of hypotension exposure, and to identify harm thresholds for hypotension when applicable.
Meta-analyses
Studies were eligible for inclusion in the meta-analyses if they were designed to study the relationship between hypotension and one of the predefined patient outcomes. Observational studies additionally had to report a confounder-adjusted outcome measure (e.g., adjusted odds ratio [OR]) and the list of confounders included in the analysis. Meta-analysis was conducted if at least three studies per predefined outcome reported the same outcome measure (OR, relative risk [RR], or hazard ratio [HR]). When studies reported multiple confounder-adjusted outcome measures, the outcome measure most frequently reported by other studies was selected for meta-analyses (e.g., adjusted OR for mortality and HR for myocardial injury). If a study reported outcome data for multiple definitions for hypotension (e.g., MAP < 65 mmHg and SBP < 90 mmHg) or for multiple outcome definitions (e.g., in-hospital mortality and ICU mortality), the data corresponding to the definition that was most frequently reported in other included articles were used in the meta-analyses. Studies reporting an association for multiple outcomes (e.g., mortality and AKI) were included in each corresponding meta-analysis. We used the inverse variance method to conduct random-effect meta-analyses, thereby incorporating the assumption that different studies estimate distinct, yet related, study effects [15]. However, fixed-effect meta-analysis was used when fewer than six articles were available per outcome, as an accurate estimation of the between-study variance could not be obtained. The percentage of variance due to between-study variation was estimated by the I2 statistic. Funnel plots were used to examine potential publication bias. We opted for Peter’s test, a modified version of Macaskill’s test [16], to assess for funnel plot asymmetry since we expected considerable between-study variation, as indicated by previous systematic reviews on intraoperative hypotension [17,18,19]. Subgroup meta-analysis per pre-defined ICU patient population was conducted if at least three studies reported data on the same patient population.
Sensitivity meta-analyses
Two sensitivity analyses were conducted to assess the influence of decisions made during the design of this systematic review and meta-analysis on the associations found. In our first sensitivity analysis, we added studies that were not specifically designed to study the relationship between hypotension and patient outcomes, but nonetheless reported a hypotension-related outcome measure obtained from multivariable analysis. The second sensitivity analysis included all studies from which an OR (adjusted or unadjusted) could be extracted or calculated and was conducted to minimize the exclusion of studies caused by heterogeneity in reported outcome measures.
Effect of perceived hypotension severity on mortality and acute kidney injury
We conducted exploratory meta-analyses by stratifying studies based on the severity of hypotension studied. The large variation in hypotension definitions reported in literature complicates the ranking of hypotension definitions. Currently, there is no consensus on the definition of hypotension, and the difference in the potential harmfulness of using MAP versus SBP-based definitions is unknown. We, therefore, asked an expert panel of nine intensivists to rank the reported definitions of hypotension in terms of perceived severity by clinical experts. The expert panel ranked the definitions on a scale from 1 to 9, with 9 being the most severe definition of hypotension (see supplementary Table 2). Multiple definitions could receive the same rank if thought to be equally severe. The median ranking score per definition was used to stratify studies into three groups of perceived severity of hypotension: mild (rank 1–3), moderate (rank 4–6), and severe hypotension (rank 7–9). However, the limited variety in hypotension definitions reported by studies designed to study the hypotension-outcome relationship did not allow for this exploratory analysis. We, therefore, opted to include all studies that reported a hypotension-related outcome measure obtained from multivariable analysis (similar to the studies included in our first sensitivity analysis) in this exploratory meta-analysis.
Results
Study characteristics
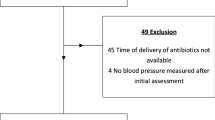
A total of 4865 unique articles were identified in PubMed, Embase, and CENTRAL. We excluded 4334 articles based on title and abstract, 397 based on full text, and 12 because no full text was obtained after contacting the corresponding authors. The PRISMA flow diagram for this systematic review is available in Fig. 1. In total, 122 articles (176,329 patients) were included in this systematic review, of which 18 were included in the primary meta-analyses, and 91 were included in sensitivity analyses. The majority of articles were cohort studies, eight were (quasi) RCTs, three case-controls, and one was propensity score matched. There was a large heterogeneity in the studied patient populations, and women were underrepresented in the majority of studies. The number of studies per outcome ranged from 82 for mortality and zero for PICS and WHODAS scores. A summarized overview of all included articles with relevant outcome data is available in the supplementary Table 3. All non-randomized studies had a NOS score of four or higher, and the potential for bias in the included RCTs ranged from “low” to “some concern” (supplementary Table 4). Over 40 different definitions for hypotension were reported. These definitions varied in terms of the type of parameter reported (e.g., SBP or patients requiring vasopressor therapy) and the threshold used (e.g., SBP < 100 mmHg or > 30% decrease from baseline).
PRISMA flow diagram of included studies. Of the two articles analyzing the Medical Information Mart for Intensive Care (MIMIC) cohort and reporting data on mortality [8, 20], one could be included in the meta-analysis [8]. The article with the highest NOS score was used in the summary table [20]. Three articles analyzed the MIMIC database for acute kidney injury outcomes [7, 46, 47]. The article with the lowest NOS score was excluded [46], the article with the highest NOS score could not be included in the meta-analysis and was thus only used in the summary table [7], and the third article was used in our sensitivity meta-analysis [47]. Of the two other articles [10, 48] reporting mortality, acute kidney, poor cognitive functioning, duration of mechanical ventilation and quality of life data from The 65 Trial, the article with the earliest publication date was included [10]
Mortality
Out of the 82 included articles (144,623 patients) that reported outcome data for this parameter, 18 (62,804 patients) were specifically designed to study the hypotension-mortality relationship [2,3,4, 9,10,11, 20,21,22,23,24,25,26,27,28,29,30,31]. Twelve (67%) of these studies, conducted in eight distinct patient populations, reported an association in favor of ‘no hypotension’, and none in favor of hypotension. Five articles reported associations for increasing severity of hypotension [3, 4, 20, 21, 26], four of which reported increasing associations with mortality for incremental depth or duration of hypotension [3, 4, 20, 21]. A MAP below 60 mmHg was associated with mortality in all six studies reporting outcome data for this definition of hypotension [3, 4, 21, 22, 26, 30] and a SBP below 90 mmHg in three of the four studies [2, 22, 25]. A total of 13 articles (34,829 patients) were included in the meta-analysis (Fig. 2), where an association between hypotension and mortality was found with an OR of 1.45 (95% confidence interval [CI] 1.12–1.88; I2 = 94%) [2, 9,10,11, 21,22,23,24,25, 28,29,30,31]. There was no sign of publication bias based on the funnel plot (supplementary Fig. 1) and Peter’s test (t = − 1.05, df = 11, p-value 0.317). Sensitivity meta-analysis including RCTs and all observational studies that reported an adjusted odds ratio for hypotension (30 studies, 48,086 patients), regardless of the studies’ objectives, or including studies from which an OR (adjusted or unadjusted) could be extracted or calculated (65 studies, 67,909 patients), increased the strength of the association (see supplementary Fig. 2A, B).
Forest plot for mortality. The forest plot is based on 13 articles (34,829 patients) designed to study the hypotension-mortality relationship. This includes randomized controlled trials and observational studies that conducted a confounder-adjusted analysis specifically to study this relationship [2, 9,10,11, 21,22,23,24,25, 28,29,30,31]. A random-effects meta-analysis based on the inverse variance method was conducted. All blood pressure thresholds are displayed in mmHg. CI confidence interval, h hour, ICU intensive care unit, MAP mean arterial pressure, min minute, SBP systolic blood pressure, vasopr. vasopressor. *Within 30 min post endotracheal intubation. †Or transfer or death. ‡Or until 5 days after randomization
Acute kidney injury
We included 36 articles (76,614 patients) on AKI, of which 14 (24,714 patients) were dedicated to studying the hypotension-AKI relationship [3, 4, 7, 9,10,11, 26, 32,33,34,35,36,37,38]. Of the 14 studies, eight (57%) reported an association in favor of ‘no hypotension’ and none in favor of ‘hypotension’. Studies with an association in favor of ‘no hypotension’ were conduct in four distinct patient populations. Six articles investigated the effect of incremental depth or duration of hypotension on AKI, with five of them finding stronger associations as the severity of hypotension increased [3, 4, 7, 32, 33]. A MAP below 55 mmHg was associated with AKI in three of the four articles studying this definition [3, 4, 7]. Meta-analysis including six articles (13,765 patients) did not demonstrate an association between hypotension and AKI (OR 1.17; 95% CI 0.97–1.41; I2 = 54%; see Fig. 3) [3, 9,10,11, 33, 38]. No funnel plot asymmetry was noted (supplementary Fig. 1) and Peter’s test was not statistically significant (t = 1.49, df = 4, p-value 0.210), indicating absence of potential publication bias. No associations were found using subgroup meta-analysis stratified per patient population (supplementary Fig. 3A). Sensitivity analyses including all studies reporting an adjusted odds ratio (13 studies, 15,269 patients) or including all studies from which an OR (adjusted or unadjusted) could be obtained (27 studies, 28,852 patients), resulted in an association in favor of ‘no hypotension’ (see supplementary Fig. 3B, C).
Forest plot for acute kidney injury. The forest plot is based on articles designed to study the hypotension-acute kidney injury relationship. This includes randomized controlled trials and observational studies that conducted a confounder-adjusted analysis specifically to study this relationship [3, 9,10,11, 33, 37, 38]. A random-effects meta-analysis based on the inverse variance method was conducted. All blood pressure thresholds are displayed in mmHg. AKI acute kidney injury, CI confidence interval, creat. serum creatinine, h hour, ICU intensive care unit, KDIGO Kidney Disease Improving Global Outcomes criteria, MAP mean arterial pressure, RRT renal replacement therapy, vasopr. vasopressor. *Or transfer or death. †Or until 5 days after randomization
Myocardial injury
The association between myocardial injury and ICU hypotension was reported in seven articles (15,414 patients), three of which (14,717 patients) reported outcome data from an analysis dedicated to study the hypotension-myocardial injury relationship [3, 4, 35]. Two of the hypotension-specific studies reported an association in favor of ‘no hypotension’, and none in favor of hypotension. Duration and depth of hypotension did not impact the association with myocardial injury [3, 4]. The heterogeneity in reported outcome measures resulted in an insufficient number of studies to conduct the main meta-analysis. Sensitivity meta-analysis based on studies reporting an adjusted HR for hypotension (three studies, 6158 patients), regardless of the studies’ objectives, resulted in an association in favor of ‘no hypotension’ (supplementary Fig. 4).
Ischemic cerebrovascular accident
A total of two articles (3637 patients) reported on the association with iCVA, one of which (3169 patients) conducted a confounder-adjusted analysis to isolate the hypotension-iCVA relationship [4]. In this study, no association between hypotension and iCVA was found.
Delirium
Three (1932 patients) out of six (3119 patients) included studies were designed to study the hypotension-delirium relationship [39,40,41]. One reported an association in favor of 'no hypotension,' while none favored hypotension.
Poor cognitive functioning
Eleven articles (9490 patients) reported on cognitive functioning, of which three studies (2144 patients) conducted an analysis to determine the confounder-adjusted association with hypotension [10, 11, 42]. The lowest MAP measured in the first six hours of ICU stay was associated with poor cognitive functioning in one study and none of the articles reported an outcome in favor of hypotension [42]. No main meta-analysis was conducted as all studies reported a different outcome measure, but a sensitivity meta-analysis including four studies (1293 patients) reporting an adjusted RR for hypotension, regardless of the study’s objectives, resulted in an association in favor of ‘no hypotension’ (supplementary Fig. 5).
Length of ICU stay
We included nine articles (7580 patients) on the association between hypotension and length of ICU stay, two of which (3206 patients) were specifically designed to study this relationship [10, 31]. No significant associations were found.
Duration of mechanical ventilation
Two articles (748 patients) on hypotension and duration of mechanical ventilation were included, one of which (479 patients) conducted a hypotension specific analysis but no significant associations were reported.
Quality of life
Two articles (1858 patients) studied the association with quality of life, one of which (1462 patients) was designed to study this association. No association with hypotension was reported by this study.
Effect of severity of hypotension exposure on mortality and morbidity
Our exploratory subgroup analysis did not demonstrate a relation between the perceived hypotension severity as ranked by intensivists and the strength of association with mortality and AKI (supplementary Fig. 6A, B).
Discussion
Exposure to hypotension during ICU stay was associated with increased mortality and morbidity in the majority of articles included in this systematic review. The descriptive findings for mortality were underscored by our meta-analysis and sensitivity analyses but conflicting results were found for the association with AKI. The number of studies for other outcomes was insufficient to conduct our main meta-analysis. Incremental depth or duration of hypotension resulted in a stronger association with poor patient outcomes in the majority of studies reporting outcome data for multiple gradations of hypotension exposure, suggesting an exposure-severity relationship. Hypotension definitions most consistently associated with mortality and AKI were a MAP below 60 mmHg or SBP below 90 mmHg and MAP below 55 mmHg, respectively.
Our results are in line with three systematic reviews on the relationship between intraoperative hypotension and postoperative mortality and AKI [17,18,19]. Among these reviews, two conducted meta-analyses that, much like our own review, relied on cohort and case–control studies [18, 19]. Wijnberge et al.’s review additionally reported a stronger association between hypotension and morbidity for severe hypotension compared to mild and moderate hypotension [18]. This observation found support in the work of Wesselink et al., who, instead of conducting a meta-analysis, created a synthesis table by organizing studies based on the severity of hypotension studied and presenting their associations with postoperative adverse outcomes [17]. The strength of the association progressively correlated with the depth of the hypotensive event in their systematic review. We found similar results within studies comparing multiple definitions for hypotension, but our exploratory meta-analyses based on the perceived severity of hypotension as ranked by intensivists did not support this exposure-severity relationship. However, the number of studies ranked as mild and severe hypotension was, with three or less, limited. In addition, we could not fully assess the impact of potential confounding factors on the association between hypotension severity and patient outcomes, primarily due to the heterogeneity in the reporting of these potential confounders (e.g., ICU patient population and disease severity score).
Randomized trials studying the effect of hypotension on mortality and morbidity are limited due to challenges in maintaining predefined blood pressure targets and the absence of consensus on the definition for hypotension. This systematic review included four RCTs that assigned patients to different blood pressure targets [9,10,11, 24]. Although these trials showed a clear distinction in average blood pressure values in both study arms, the average MAP in the lower target group of all RCTs exceeded the commonly used hypotension definitions of MAP < 65 mmHg and SBP < 90 mmHg. Consequently, exposure to hypotension in the lower target groups might have been limited compared to the observational studies included in this systematic review. Furthermore, assigning patients to a higher blood pressure threshold does not necessarily prevent hypotensive events. Patients in both the higher and lower blood pressure target group may have had similar exposure to critically low blood pressure, even if the average blood pressure of one group was substantially higher. Moreover, maintaining higher blood pressure thresholds required higher vasopressor dosages [9, 11], which is independently associated with poor patient outcomes [43, 44]. This may have contributed to the neutral findings of blood pressure target RCTs, and the absence of an association between hypotension and AKI in our main meta-analysis, as halve of the included studies were RCTs.
Our systematic review has limitations that affect the interpretation and clinical applicability of the findings. Most studies included did not primarily aim to study the relationship between hypotension and patient outcomes, but rather sought predictors of patient outcomes. As a result, reported adjusted ORs, RRs, and HRs were often not adjusted for biases specifically relevant to the hypotension-patient outcomes relationship, resulting in a relatively small number of studies included in the assessment of our primary objective. Moreover, differing patient populations, outcome definitions, and reported outcome data among studies hindered interpretation of the results. We aimed to address some differences by limiting our sensitivity meta-analyses to articles from which an OR could be extracted or calculated and by stratifying studies per ICU patient population but the number of studies reporting on the same patient population was insufficient for subgroup meta-analysis in all outcomes except AKI. Adding to the complexity was the wide range of reported hypotension definitions. While most studies mentioned the threshold for hypotension, the minimally required event duration or time spent below a certain threshold was often not specified. This hinders data synthesis and the ranking of hypotension severity, as hypotensive events with a MAP of 55 mmHg for one minute might be less harmful compared to a MAP of 60 mmHg for 1 h. Therefore, we only assessed the exposure-severity relation within studies and based the hypotension ranking of our exploratory meta-analysis on expert opinion. Employing this hypotension ranking method was deemed the best available approach to conduct an exposure-effect meta-analysis, but this method has not been validated. Consequently, the results of the exploratory analysis should be interpreted with caution. Furthermore, clinical context information of hypotensive events was limited. This means that both a patient with a temporary SBP < 90 mmHg due to an anesthetic drug bolus and a patient with a persistent SBP < 90 mmHg due to distributive shock were labeled as hypotensive, despite differences in disease severity, event etiology, duration, and potential damage caused. These factors collectively contributed to extensive heterogeneity. Additionally, most articles did not provide information on patient exposure to hypotension prior to ICU admission. Thus, the associations described in this review are not exclusively attributable to hypotension during ICU stay. Lastly, exposure to hypotension may have a causal effect on mortality, but it is essential to recognize that hypotension severity also serves as a marker of illness severity. As a result, the prognosis differs among patients with varying degrees of hypotension exposure. Therefore, a precise estimate of the causal effect of hypotension on outcomes cannot be obtained through meta-analysis due to the inability to meet the consistency or Stable Unit Treatment Value Assumption required for causal effect estimation [45]. Nonetheless, the observed relationship between exposure and severity within studies highlights that sustained interventions to modify hypotension can substantially change patient outcomes. Future intervention trials should concentrate on causally treating each hypotensive event or even preventing hypotension, instead of merely comparing blood pressure targets. Observational studies should distinctly define both the threshold and duration of hypotensive events, should assess the relationship between hypotension and outcome for multiple hypotension definitions, and should explore hypotension exposure as a continuous variable rather than binary before we can fully comprehend the causality between hypotension during ICU stay and patient outcomes.
Conclusion
In conclusion, exposure to hypotension during ICU stay was associated with an increase in mortality. The majority of included studies additionally reported associations between hypotension exposure and acute kidney injury. Furthermore, the associations for both outcomes increased with increasing hypotension severity in studies comparing multiple levels of hypotension exposure. The direction of the associations found between hypotension and patient outcomes was particularly consistent for a mean arterial pressure below 60 mmHg and systolic blood pressure below 90 mmHg for mortality and mean arterial pressure below 55 mmHg for acute kidney injury. Interventional studies targeting specific patient populations and outcomes are essential to fully comprehend the causality between hypotension during ICU stay and patient outcomes.
Data availability
The data that support the findings of this study are available from the authors upon reasonable request.
References
van der Ven WH, Schuurmans J, Schenk J, Roerhorst S, Cherpanath TGV, Lagrand WK, Thoral P, Elbers PWG, Tuinman PR, Scheeren TWL, Bakker J, Geerts BF, Veelo DP, Paulus F, Vlaar APJ (2022) Monitoring, management, and outcome of hypotension in Intensive Care Unit patients, an international survey of the European Society of Intensive Care Medicine. J Crit Care 67:118–125. https://doi.org/10.1016/j.jcrc.2021.10.008
Trzeciak S, Jones AE, Kilgannon JH, Milcarek B, Hunter K, Shapiro NI, Hollenberg SM, Dellinger P, Parrillo JE (2009) Significance of arterial hypotension after resuscitation from cardiac arrest. Crit Care Med 37:2895–2903. https://doi.org/10.1097/CCM.0b013e3181b01d8c
Maheshwari K, Nathanson BH, Munson SH, Khangulov V, Stevens M, Badani H, Khanna AK, Sessler DI (2018) The relationship between ICU hypotension and in-hospital mortality and morbidity in septic patients. Intensive Care Med 44:857–867. https://doi.org/10.1007/s00134-018-5218-5
Smischney NJ, Shaw AD, Stapelfeldt WH, Boero IJ, Chen Q, Stevens M, Khanna AK (2020) Postoperative hypotension in patients discharged to the intensive care unit after non-cardiac surgery is associated with adverse clinical outcomes. Crit Care 24:682. https://doi.org/10.1186/s13054-020-03412-5
Bijker JB, van Klei WA, Kappen TH, van Wolfswinkel L, Moons KG, Kalkman CJ (2007) Incidence of intraoperative hypotension as a function of the chosen definition: literature definitions applied to a retrospective cohort using automated data collection. Anesthesiology 107:213–220. https://doi.org/10.1097/01.anes.0000270724.40897.8e
Schenk J, van der Ven WH, Schuurmans J, Roerhorst S, Cherpanath TGV, Lagrand WK, Thoral P, Elbers PWG, Tuinman PR, Scheeren TWL, Bakker J, Geerts BF, Veelo DP, Paulus F, Vlaar APJ (2021) Definition and incidence of hypotension in intensive care unit patients, an international survey of the European Society of Intensive Care Medicine. J Crit Care 65:142–148. https://doi.org/10.1016/j.jcrc.2021.05.023
Lehman LW, Saeed M, Moody G, Mark R (2010) Hypotension as a risk factor for acute kidney injury in ICU patients. Comput Cardiol 37:1095–1098
Vincent JL, Nielsen ND, Shapiro NI, Gerbasi ME, Grossman A, Doroff R, Zeng F, Young PJ, Russell JA (2018) Mean arterial pressure and mortality in patients with distributive shock: a retrospective analysis of the MIMIC-III database. Ann Intensive Care 8:107. https://doi.org/10.1186/s13613-018-0448-9
Asfar P, Meziani F, Hamel JF, Grelon F, Megarbane B, Anguel N, Mira JP, Dequin PF, Gergaud S, Weiss N, Legay F, Le Tulzo Y, Conrad M, Robert R, Gonzalez F, Guitton C, Tamion F, Tonnelier JM, Guezennec P, Van Der Linden T, Vieillard-Baron A, Mariotte E, Pradel G, Lesieur O, Ricard JD, Hervé F, du Cheyron D, Guerin C, Mercat A, Teboul JL, Radermacher P (2014) High versus low blood-pressure target in patients with septic shock. N Engl J Med 370:1583–1593. https://doi.org/10.1056/NEJMoa1312173
Lamontagne F, Richards-Belle A, Thomas K, Harrison DA, Sadique MZ, Grieve RD, Camsooksai J, Darnell R, Gordon AC, Henry D, Hudson N, Mason AJ, Saull M, Whitman C, Young JD, Rowan KM, Mouncey PR (2020) Effect of reduced exposure to vasopressors on 90-day mortality in older critically ill patients with vasodilatory hypotension: a randomized clinical trial. JAMA 323:938–949. https://doi.org/10.1001/jama.2020.0930
Kjaergaard J, Møller JE, Schmidt H, Grand J, Mølstrøm S, Borregaard B, Venø S, Sarkisian L, Mamaev D, Jensen LO, Nyholm B, Høfsten DE, Josiassen J, Thomsen JH, Thune JJ, Obling LER, Lindholm MG, Frydland M, Meyer MAS, Winther-Jensen M, Beske RP, Frikke-Schmidt R, Wiberg S, Boesgaard S, Madsen SA, Jørgensen VL, Hassager C (2022) Blood-pressure targets in comatose survivors of cardiac arrest. N Engl J Med 387:1456–1466. https://doi.org/10.1056/NEJMoa2208687
Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A (2016) Rayyan—a web and mobile app for systematic reviews. Syst Rev 5:210. https://doi.org/10.1186/s13643-016-0384-4
Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, Cates CJ, Cheng HY, Corbett MS, Eldridge SM, Emberson JR, Hernán MA, Hopewell S, Hróbjartsson A, Junqueira DR, Jüni P, Kirkham JJ, Lasserson T, Li T, McAleenan A, Reeves BC, Shepperd S, Shrier I, Stewart LA, Tilling K, White IR, Whiting PF, Higgins JPT (2019) RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ 366:l4898. https://doi.org/10.1136/bmj.l4898
Wells GA, Wells G, Shea B, Shea B, O'Connell D, Peterson J, Welch, Losos M, Tugwell P, Ga SW, Zello GA, Petersen JA (2014) The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Environ Sci
Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (2022) Cochrane handbook for systematic reviews of interventions version 6.3 (updated February 2022)
Peters JL, Sutton AJ, Jones DR, Abrams KR, Rushton L (2006) Comparison of two methods to detect publication bias in meta-analysis. JAMA 295:676–680. https://doi.org/10.1001/jama.295.6.676
Wesselink EM, Kappen TH, Torn HM, Slooter AJC, van Klei WA (2018) Intraoperative hypotension and the risk of postoperative adverse outcomes: a systematic review. Br J Anaesth 121:706–721. https://doi.org/10.1016/j.bja.2018.04.036
Wijnberge M, Schenk J, Bulle EB, Vlaar APJ, Maheshwari K, Hollmann MW, Binnekade JM, Geerts BF, Veelo DP (2021) Association of intraoperative hypotension with postoperative morbidity and mortality: systematic review and meta-analysis. BJS Open. https://doi.org/10.1093/bjsopen/zraa018
Gu WJ, Hou BL, Kwong JSW, Tian X, Qian Y, Cui Y, Hao J, Li JC, Ma ZL, Gu XP (2018) Association between intraoperative hypotension and 30-day mortality, major adverse cardiac events, and acute kidney injury after non-cardiac surgery: a meta-analysis of cohort studies. Int J Cardiol 258:68–73. https://doi.org/10.1016/j.ijcard.2018.01.137
Hu AM, Hai C, Wang HB, Zhang ZH, Sun LB, Zhang ZJ, Li HP (2021) Associations between elevated systolic blood pressure and outcomes in critically ill patients: a retrospective cohort study and propensity analysis. Shock (Augusta, Ga). https://doi.org/10.1097/SHK.0000000000001774
Humaloja J, Skrifvars MB, Raj R, Wilkman E, Pekkarinen PT, Bendel S, Reinikainen M, Litonius E (2021) The association between arterial oxygen level and outcome in neurocritically ill patients is not affected by blood pressure. Neurocrit Care 34:413–422. https://doi.org/10.1007/s12028-020-01178-w
Jentzer JC, Burstein B, Van Diepen S, Murphy J, Holmes DR Jr, Bell MR, Barsness GW, Henry TD, Menon V, Rihal CS, Naidu SS, Baran DA (2021) Defining shock and preshock for mortality risk stratification in cardiac intensive care unit patients. Circ Heart Fail 14:e007678. https://doi.org/10.1161/circheartfailure.120.007678
Ko CH, Lan YW, Chen YC, Cheng TT, Yu SF, Cidem A, Liu YH, Kuo CW, Yen CC, Chen W, Chen CM (2021) Effects of mean artery pressure and blood ph on survival rate of patients with acute kidney injury combined with acute hypoxic respiratory failure: a retrospective study. Medicina (Kaunas). https://doi.org/10.3390/medicina57111243
Lamontagne F, Meade MO, Hébert PC, Asfar P, Lauzier F, Seely AJE, Day AG, Mehta S, Muscedere J, Bagshaw SM, Ferguson ND, Cook DJ, Kanji S, Turgeon AF, Herridge MS, Subramanian S, Lacroix J, Adhikari NKJ, Scales DC, Fox-Robichaud A, Skrobik Y, Whitlock RP, Green RS, Koo KKY, Tanguay T, Magder S, Heyland DK (2016) Higher versus lower blood pressure targets for vasopressor therapy in shock: a multicentre pilot randomized controlled trial. Intensive Care Med 42:542–550. https://doi.org/10.1007/s00134-016-4237-3
Ng L, Ghobrial M, Peoples J, Shah SO, Vibbert M, Urtecho J, Athar MK, Bar B, Jallo J, Pineda CC, Tzeng D, Bell R, Rincon F (2015) Incidence of circulatory shock after spontaneous intracerebral hemorrhage and impact on case-fatality: a multi-center cohort study. Crit Care Shock 18:72–81
Patidar KR, Peng JL, Pike F, Orman ES, Glick M, Kettler CD, Nephew LD, Desai AP, Nair K, Khan BA, Buckley CA, Machado RF, Chalasani NP, Ghabril MS (2020) Associations between mean arterial pressure and poor ICU outcomes in critically ill patients with cirrhosis: is 65 the sweet spot? Crit Care Med 48:e753–e760. https://doi.org/10.1097/ccm.0000000000004442
Winchell RJ, Simons RK, Hoyt DB (1996) Transient systolic hypotension. a serious problem in the management of head injury. Arch Surg 131:533–539. https://doi.org/10.1001/archsurg.1996.01430170079015
Burstein B, Tabi M, Barsness GW, Bell MR, Kashani K, Jentzer JC (2020) Association between mean arterial pressure during the first 24 hours and hospital mortality in patients with cardiogenic shock. Crit Care 24:513. https://doi.org/10.1186/s13054-020-03217-6
Cengic S, Zuberi M, Bansal V, Ratzlaff R, Rodrigues E, Festic E (2020) Hypotension after intensive care unit drop-off in adult cardiac surgery patients. World J Crit Care Med 9:20–30. https://doi.org/10.5492/wjccm.v9.i2.20
Dünser MW, Takala J, Ulmer H, Mayr VD, Luckner G, Jochberger S, Daudel F, Lepper P, Hasibeder WR, Jakob SM (2009) Arterial blood pressure during early sepsis and outcome. Intensive Care Med 35:1225–1233. https://doi.org/10.1007/s00134-009-1427-2
Green RS, Turgeon AF, McIntyre LA, Fox-Robichaud AE, Fergusson DA, Doucette S, Butler MB, Erdogan M (2015) Postintubation hypotension in intensive care unit patients: a multicenter cohort study. J Crit Care 30:1055–1060. https://doi.org/10.1016/j.jcrc.2015.06.007
Dupont V, Bonnet-Lebrun AS, Boileve A, Charpentier J, Mira JP, Geri G, Cariou A, Jozwiak M (2022) Impact of early mean arterial pressure level on severe acute kidney injury occurrence after out-of-hospital cardiac arrest. Ann Intensive Care 12:69. https://doi.org/10.1186/s13613-022-01045-1
Izawa J, Kitamura T, Iwami T, Uchino S, Takinami M, Kellum JA, Kawamura T (2016) Early-phase cumulative hypotension duration and severe-stage progression in oliguric acute kidney injury with and without sepsis: an observational study. Crit Care 20:405. https://doi.org/10.1186/s13054-016-1564-2
Janssen van Doorn K, Verbrugghe W, Wouters K, Jansens H, Jorens PG (2014) The duration of hypotension determines the evolution of bacteremia-induced acute kidney injury in the intensive care unit. PLoS ONE 9:e114312. https://doi.org/10.1371/journal.pone.0114312
Khanna AK, Maheshwari K, Mao G, Liu L, Perez-Protto SE, Chodavarapu P, Schacham YN, Sessler DI (2019) Association between mean arterial pressure and acute kidney injury and a composite of myocardial injury and mortality in postoperative critically ill patients: a retrospective cohort analysis. Crit Care Med 47:910–917. https://doi.org/10.1097/ccm.0000000000003763
Kotani Y, Yoshida T, Kumasawa J, Kamei J, Taguchi A, Kido K, Yamaguchi N, Kariya T, Nakasone M, Mikami N, Koga T, Nakayama I, Shibata M, Yoshida T, Nashiki H, Karatsu S, Nogi K, Tokuhira N, Izawa J (2021) The impact of relative hypotension on acute kidney injury progression after cardiac surgery: a multicenter retrospective cohort study. Ann Intensive Care 11:178. https://doi.org/10.1186/s13613-021-00969-4
Panwar R, Tarvade S, Lanyon N, Saxena M, Bush D, Hardie M, Attia J, Bellomo R, Van Haren F (2020) Relative hypotension and adverse kidney-related outcomes among critically ill patients with shock. a multicenter, prospective cohort study. Am J Respir Crit Care Med 202:1407–1418. https://doi.org/10.1164/rccm.201912-2316OC
Poukkanen M, Wilkman E, Vaara ST, Pettilä V, Kaukonen KM, Korhonen AM, Uusaro A, Hovilehto S, Inkinen O, Laru-Sompa R, Hautamäki R, Kuitunen A, Karlsson S (2013) Hemodynamic variables and progression of acute kidney injury in critically ill patients with severe sepsis: data from the prospective observational FINNAKI study. Crit Care 17:R295. https://doi.org/10.1186/cc13161
Maheshwari K, Ahuja S, Khanna AK, Mao G, Perez-Protto S, Farag E, Turan A, Kurz A, Sessler DI (2020) Association between perioperative hypotension and delirium in postoperative critically ill patients: a retrospective cohort analysis. Anesth Analg 130:636–643. https://doi.org/10.1213/ane.0000000000004517
Nguyen DN, Huyghens L, Parra J, Schiettecatte J, Smitz J, Vincent JL (2018) Hypotension and a positive fluid balance are associated with delirium in patients with shock. PLoS ONE 13:e0200495. https://doi.org/10.1371/journal.pone.0200495
Wang J, Mao G, Malackany N, Marciniak D, Donaldson C, Wakefield B, Hassan M, Ruetzler K, Sessler DI, Turan A (2022) Association between perioperative hypotension and postoperative delirium and atrial fibrillation after cardiac surgery: a post-hoc analysis of the DECADE trial. J Clin Anesth 76:110584. https://doi.org/10.1016/j.jclinane.2021.110584
Laurikkala J, Wilkman E, Pettila V, Kurola J, Reinikainen M, Hoppu S, Ala-Kokko T, Tallgren M, Tiainen M, Vaahersalo J, Varpula T, Skrifvars MB (2016) Mean arterial pressure and vasopressor load after out-of-hospital cardiac arrest: associations with one-year neurologic outcome. Resuscitation 105:116–122. https://doi.org/10.1016/j.resuscitation.2016.05.026
Mebazaa A, Parissis J, Porcher R, Gayat E, Nikolaou M, Boas FV, Delgado JF, Follath F (2011) Short-term survival by treatment among patients hospitalized with acute heart failure: the global ALARM-HF registry using propensity scoring methods. Intensive Care Med 37:290–301. https://doi.org/10.1007/s00134-010-2073-4
Mebazaa A, Motiejunaite J, Gayat E, Crespo-Leiro MG, Lund LH, Maggioni AP, Chioncel O, Akiyama E, Harjola VP, Seferovic P, Laroche C, Julve MS, Roig E, Ruschitzka F, Filippatos G (2018) Long-term safety of intravenous cardiovascular agents in acute heart failure: results from the European Society of Cardiology Heart Failure Long-Term Registry. Eur J Heart Fail 20:332–341. https://doi.org/10.1002/ejhf.991
VanderWeele TJ, Hernan MA (2013) Causal inference under multiple versions of treatment. J Causal Inference 1:1–20. https://doi.org/10.1515/jci-2012-0002
Fan C, Ding X, Song Y (2021) A new prediction model for acute kidney injury in patients with sepsis. Ann Palliat Med 10:1772–1778. https://doi.org/10.21037/apm-20-1117
Lehman LW, Saeed M, Talmor D, Mark R, Malhotra A (2013) Methods of blood pressure measurement in the ICU. Crit Care Med 41:34–40. https://doi.org/10.1097/CCM.0b013e318265ea46
Mouncey PR, Richards-Belle A, Thomas K, Harrison DA, Zia Sadique M, Grieve RD, Camsooksai J, Darnell R, Gordon AC, Henry D et al (2021) Reduced exposure to vasopressors through permissive hypotension to reduce mortality in critically ill people aged 65 and over: the 65 RCT. Health Technol Assess 25:VII–77. https://doi.org/10.3310/HTA25140
Acknowledgements
We would like to thank Faridi van Etten—Jamaludin for her help conducting the search and Myrthe Biesma for her help screening articles on title and abstract.
Funding
This project was conducted without receiving any specific funding.
Author information
Authors and Affiliations
Contributions
JaS, NM, WV, JiS, DPV, and APJV contributed to the conception and design of the study. The data acquisition was conducted by JaS, BTBR, SRR, JTMT, and VCK. The analysis and interpretation of the data were performed by JaS, JiS, DPV, and APJV. The first draft of the article was written by JaS, and all authors provided critical revisions. All authors approved the submitted version of the article.
Corresponding author
Ethics declarations
Conflicts of interest
JS, DPV and APJV report receipt of consulting fees from Edwards Lifesciences paid to the institution. DPV additionally reports receipt of research grants from Philips and Edwards Lifesciences and APJV reports receipt of unrestricted research grants from Edwards Lifesciences.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Schuurmans, J., van Rossem, B.T.B., Rellum, S.R. et al. Hypotension during intensive care stay and mortality and morbidity: a systematic review and meta-analysis. Intensive Care Med 50, 516–525 (2024). https://doi.org/10.1007/s00134-023-07304-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-023-07304-4