Abstract
Purpose
Unplanned extubation (UE) is an important paediatric intensive care unit (PICU) quality indicator. Studies on UE have been modest in size, with accurate UE rate calculation potentially hampered by ventilation episodes recorded in calendar days. We wished to document UE rates, outcomes, associated factors and quantify error when calendar days rather than exact timings are used.
Methods
We recorded prospectively all UE episodes and potential associated factors in our 20-bed PICU for 12,533 admissions (2000–2013). Ventilation episodes were recorded to the minute, with non-invasive and tracheostomy ventilation excluded. Analysis utilised multilevel mixed-effects Poisson regression, adjusting for multiple ventilation episodes in the same patient.
Results
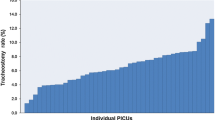
Overall, 243 UEs occurred within 14,141 ventilation episodes (31,564 intubated days), giving a UE rate of 0.77 (95 % CI 0.67–0.87) episodes per 100 intubated days. If calendar ventilation days were used, the yearly UE rate was underestimated by 27–35 %. UE rates decreased with time, by approximately 0.05/100 intubated days each year. Associations with UE incidence rate included patient age, source of admission, disease severity and diagnostic category, with nasal tubes decreasing the risk. Although UE versus planned extubation was associated with a higher re-intubation rate (43 versus 8 %) and longer median PICU stay (4.6 versus 2.6 days, p < 0.001), mortality between the two groups did not differ (3.0 versus 5.1 %, p = 0.18).
Conclusions
This study provides contemporaneous UE rates for benchmarking. Recording ventilation in calendar days underestimates UE rate. Several factors associated with UE may serve as a focus of quality improvement.



Similar content being viewed by others
References
Slater A (2004) Monitoring outcome in paediatric intensive care. Paediatr Anaesth 14:113–116
NHS England (2013) Service specifications for paediatric intensive care. http://www.england.nhs.uk/commissioning/wp-content/uploads/sites/12/2013/07/eo7sa-paed-inten-care.pdf. Accessed 16 Dec 2014
De Vos M, Graafmans W, Keesman E et al (2007) Quality measurement at intensive care units: which indicators should we use? J Crit Care 22:267–274
Kapadia F, Bajan K, Raje K (2000) Airway accidents in intubated intensive care unit patients: an epidemiological study. Crit Care Med 28:659–664
De Lassence A, Alberti C, Azoulay E et al (2002) Impact of unplanned extubation and reintubation after weaning on nosocomial pneumonia risk in the intensive care unit: a prospective multicenter study. Anesthesiology 97:148–156
Sadowski R, Dechert RE, Bandy KP et al (2004) Continuous quality improvement: reducing unplanned extubations in a pediatric intensive care unit. Pediatrics 114:628–632
Roddy DJ, Spaeder MC, Pastor W et al (2015) Unplanned extubations in children: impact on hospital cost and length of stay. Pediatr Crit Care Med. doi:10.1097/PCC.0000000000000406
Lucas da Silva PS, de Carvalho WB (2010) Unplanned extubation in pediatric critically ill patients: a systematic review and best practice recommendations. Pediatr Crit Care Med 11:287–294
Marcin JP, Rutan E, Rapetti PM et al (2005) Nurse staffing and unplanned extubation in the pediatric intensive care unit. Pediatr Crit Care Med 6:254–257
Da Silva PS, de Aguiar VE, Neto HM et al (2008) Unplanned extubation in a paediatric intensive care unit: impact of a quality improvement programme. Anaesthesia 63:1209–1216
Universities of Leeds and Leicester (2014) Paediatric intensive care audit network: annual report. http://www.picanet.org.uk/Audit/Annual-Reporting/PICANet_2014_Annual_Report_Tables_and_Figures.pdf. Accessed 16 Dec 2014
Paediatric Intensive Care Society (2010) Standards for the care of critically ill children, 4th edn, version 2. http://www.ukpics.org.uk/documents/PICS_standards.pdf. Accessed 16 Dec 2014
Advanced Life Support Group (2008) Paediatric and neonatal safe transfer and retrieval. The practical approach (PaNSTaR). Wiley, Blackwell
Arenas-López S, Riphagen S, Tibby SM et al (2004) Use of oral clonidine for sedation in ventilated paediatric intensive care patients. Intensive Care Med 30:1625–1629
Popernack ML, Thomas NJ, Lucking SE (2004) Decreasing unplanned extubations: utilization of the Penn State Children’s Hospital sedation algorithm. Pediatr Crit Care Med 5:58–62
Slater A, Shann F, Pearson G (2003) PIM2: a revised version of the Paediatric Index of Mortality. Intensive Care Med 29:278–285
Tibby SM, Correa-West J, Durward A et al (2004) Adverse events in a paediatric intensive care unit: relationship to workload, skill mix and staff supervision. Intensive Care Med 30:1160–1166
Young JQ, Ranji SR, Wachter RM et al (2011) “July effect”: impact of the academic year–end changeover on patient outcomes: a systematic review. Ann Intern Med 155:309–315
Rabe-Hesketh S, Skrondal A (2012) Multilevel and longitudinal modeling using Stata, vol II, 3rd edn. Stata, College Station
Sauerbrei W, Meier-Hirmer C, Benner A et al (2006) Multivariable regression model building by using fractional polynomials: description of SAS, STATA and R programs. Comput Stat Data Anal 50:3464–3485
Chiang AA, Lee KC, Lee JC et al (1996) Effectiveness of a continuous quality improvement program aiming to reduce unplanned extubation: a prospective study. Intensive Care Med 22:1269–1271
Chevron V, Ménard JF, Richard JC et al (1998) Unplanned extubation: risk factors of development and predictive criteria for reintubation. Crit Care Med 26:1049–1053
Bouza C, Garcia E, Diaz M et al (2007) Unplanned extubation in orally intubated medical patients in the intensive care unit: a prospective cohort study. Heart Lung 36:270–276
Little L, Koenig JJ, Newth C (1990) Factors affecting accidental extubations in neonatal and pediatric intensive care patients. Crit Care Med 18:163–165
Chang L-C, Liu P-F, Huang Y-L et al (2011) Risk factors associated with unplanned endotracheal self-extubation of hospitalized intubated patients: a 3-year retrospective case-control study. Appl Nurs Res 24:188–192
Epstein SK, Nevins ML, Chung J (2000) Effect of unplanned extubation on outcome of mechanical ventilation. Am J Respir Crit Care Med 161:1912–1916
De Groot RI, Dekkers OM, Herold IH et al (2011) Risk factors and outcomes after unplanned extubations on the ICU: a case-control study. Crit Care 15:R19
Conflicts of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Take-home message: We used a prospectively collected database over 14 years (14,141 ventilation episodes) to verify the suggested benchmark for unplanned extubation of less than 1 episode/100 intubated patient days. However, significant underestimation of the unplanned extubation rate (up to approximately one-third) occurs if ventilated days are calculated using traditional methods (calendar days), rather than recording ventilation to the hour.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Kanthimathinathan, H.K., Durward, A., Nyman, A. et al. Unplanned extubation in a paediatric intensive care unit: prospective cohort study. Intensive Care Med 41, 1299–1306 (2015). https://doi.org/10.1007/s00134-015-3872-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-015-3872-4