Abstract
Objective
Although several advantages are attributed to tracheotomy in ICU patients requiring mechanical ventilation (MV), true benefits and the optimal timing of tracheotomy remain controversial. In this study, we compared early tracheotomy (ET) with prolonged intubation (PI) in severely ill patients requiring prolonged MV.
Design
Prospective, randomized study.
Setting
Twenty-five medical and surgical ICUs in France.
Patients
Patients expected to require MV > 7 days.
Measurements and results
Patients were randomised to either (open or percutaneous) ET within 4 days or PI. The primary end-point was 28-day mortality. Secondary end-points were: the incidence of ICU-acquired pneumonia, number of d1-d28 ventilator-free days, time spent in the ICU, 60-day mortality, number of septic episodes, amount of sedation, comfort and laryngeal and tracheal complications. A sample size of 470 patients was considered necessary to obtain a reduction from 45 to 32% in 28-day mortality. After 30 months, 123 patients had been included (ET = 61, PI = 62) in 25 centres and the study was prematurely closed. All group characteristics were similar upon admission to ICU. No difference was found between the two groups for any of the primary or secondary end-points. Greater comfort was the sole benefit afforded by tracheotomy after subjective self-assessment by patients.
Conclusions
The trial did not demonstrate any major benefit of tracheotomy in a general population of ICU patients, as suggested in a previous meta-analysis, but was underpowered to draw any firm conclusions. The potential advantage of ET may be restricted to selected groups of patients.
Similar content being viewed by others
Introduction
A tracheotomy is usually proposed to facilitate airway management of intensive care unit (ICU) patients requiring prolonged mechanical ventilation (MV). However, despite decades of experience, there is still controversy over its specific indications, techniques, and timing [1]. Physician attitudes regarding tracheotomy are heterogeneous across units and the reasons for performing or withholding a tracheotomy are often exclusively based on personal convictions [2].
Tracheotomy is purported to offer several advantages: an early tracheotomy (ET) could avoid complications of trans-laryngeal intubation such as laryngeal injury, facilitate nursing care and weaning off MV and improve patient comfort [3–6]. A study in critically ill medical patients showed that early percutaneous tracheotomy was associated with reduced mortality and morbidity, and shorter MV and ICU durations [5]. However, a subsequent meta-analysis challenged the mortality benefit of ET [7].
We previously showed that practices regarding tracheotomy were highly heterogeneous. This was a strong incentive to conduct a prospective comparison of prolonged trans-laryngeal intubation (PI) and ET in unselected mechanically ventilated patients [2]. We hypothesised that ET, as compared to PI, could reduce the 28-day mortality rate, the duration of MV and the incidence of pneumonia in critically ill patients.
Patients and methods
Study design
This prospective randomized unblinded non-sponsored study was performed between April 2002 and September 2004 in 25 medical, surgical or medical-surgical ICUs in France [8]. The protocol was approved by the Ethics Committee, Kremlin Bicêtre, France. Written informed consent was obtained from all patients or their relatives.
The main goal was to demonstrate that ET performed before the end of the fourth calendar day of MV allowed a reduction in the 28-day mortality. Secondary end-points (see below) included the incidence of infectious complications, the duration of MV and length of ICU stay, day 60 and hospital mortality rates, laryngeal and tracheal complications, and patient comfort.
Patients
ICU patients who were intubated and who had been mechanically ventilated for less than 4 days were eligible if they met the following criteria: (1) older than 18 years; (2) written consent available; (3) expected duration of MV > 7 days (clinical predictors of prolonged MV were provided to the investigators [9–12] for information, but the appreciation of these criteria was left to their clinical judgment).
To optimise the external validity of the trial, exclusion criteria were minimal (previous tracheotomy or enrolment in the trial, major risk of bleeding, infection or anatomical deformity of the neck, severe respiratory insufficiency or neurological failure, and high severity of illness scores [13, 14], see details in the Electronic Supplementary Material).
Randomisation
Patients were randomly assigned to ET or PI, using a centralised computerised system before the fourth day of MV. Randomisation was stratified (minimisation) by the participating centre, type of admission (medical, scheduled surgery and unscheduled surgery), MV for neurological failure or not, and MV for exacerbated chronic obstructive pulmonary disease (COPD) or not.
Tracheotomy procedure
In the ET group, the choice of the type (percutaneous or surgical) and location (bedside—in surgical aseptic conditions—versus operating room) of procedure was left to the physician. No instructions were given for routine timing of cannula changes. After weaning off MV, the cannula had to be removed as soon as possible and within 48 h. If required due to the clinical course, a delayed tracheotomy was permitted for patients in the PI group, but after at least 14 days of MV.
Ventilation, weaning and sedation protocol
In both groups, weaning off MV was conducted according to current French recommendations [15] [daily T-piece trials or pressure support ventilation (PSV), see supplementary material]. Patients meeting weaning criteria were extubated or placed on a tracheotomy collar. Weaning failure was defined as the need, within 48 h, for reintubation or reconnection to the ventilator.
Sedation was monitored by nurses 4–6 times per day using the sedation-agitation scale (SAS) [16], to maintain the patient calm and cooperative or slightly sedated (i.e. scores 3–4), depending on severity. If sedation was deemed too deep, the dose of sedatives was decreased by 50%. Two sedatives (propofol or midazolam) and two narcotics (fentanyl or sufentanil) were recommended.
Data collection
Demographic, physiological and radiographic features, characteristics of MV and co-existing conditions were recorded on admission to the ICU and at the time of randomisation. Severity of illness and radiological scores were calculated [13–18].
End-points and follow-up
The primary end-point was death at 28 days. Secondary end-points included: d28 incidence of ICU-acquired pneumonia and duration of MV, d60 and hospital mortality rates, the total duration of MV, infectious complications (other than pneumonia) during the first 28 days, early laryngeal and tracheal complications, sedation requirements during the first 28 days and patient comfort.
ICU-acquired pneumonia
Respiratory samples were obtained when a new episode of ICU-acquired pneumonia was clinically suspected [19]. The diagnosis of pneumonia was established by positive quantitative cultures of pulmonary secretion samples [20–23] (ESM). All charts were finally reviewed by four of the investigators, blinded to the treatment arm, in order to classify the episodes as definite, probable or pneumonia excluded.
Infectious complications (other than pneumonia)
Episodes of bloodstream infections were recorded during the first 28 days. Stomal complications were recorded for patients who underwent tracheotomy (ESM). Maxillary sinusitis was not systematically investigated; nevertheless, clinical suspicion of sinusitis and any complementary investigations were recorded.
Laryngeal and tracheal complications
Early (1–5 days after extubation or cannula removal) laryngeal and tracheal examinations were performed by an ENT specialist. The number of patients presenting at least one symptom (swallowing disorders, dysphonia, dyspnoea) was recorded. These patients underwent a laryngeal and/or tracheal fiberoptic assessment. Late (2 months) complications were also sought whenever possible, with systematic fiberoptic assessment.
Sedation requirements during the first 28 days
The number and type of drugs used, cumulative daily doses, and the lowest and highest SAS scores were recorded on a daily basis. The cumulative doses of each drug used, and the median lowest and highest SAS scores during MV were compared between the two groups.
Comfort
Comfort was self-evaluated using a questionnaire distributed to each conscious patient between the end of MV and ICU discharge. Results were expressed according to a numerical scale from 1 (acceptable) to 10 (unbearable). In addition, objective comfort criteria evaluated on d28 and d60 included the time of the first transfer from bed to chair, first oral feeding and speech recovery.
Statistical analyses
Based on data obtained in French ICUs [24], we assumed that the day-28 mortality rate of patients who were mechanically ventilated 7 days or more would approximate 45%. In order to demonstrate an absolute decrease in day 28 mortality from 45 to 32% with ET, 234 patients were required in each group to reach a power of 80% with a type one error of 5% (two-sided test, Casagrande and Pike method [25]). The study was expected to be completed within 3 years.
Results are expressed as percentages or medians (range) and the two groups were compared using non parametric tests. For survival or time-dependent end-points, the randomisation date was the beginning of the follow-up and the corresponding rates were calculated using the Kaplan–Meier method [26] and Rothman’s 95% confidence intervals [95%CI] [27]. When a specific event-free rate was estimated, patients who died before the occurrence of the event of interest were censored at the date of their death. Survival and event-free curves were compared using the logrank test [28] and results are expressed with the hazard ratio (HR) of events for ET versus PI with their 95%CI. We performed an intention-to-treat analysis. All tests were two-sided. P values were only reported for significant differences at the 5% level. SAS 8.02 software (SAS Institute Inc., Cary, NC, USA) was used for statistical analyses.
After about 2 years, only 123 patients had been included in 25 centres and the study was prematurely interrupted and analysed.
Results
Patient and tracheotomy characteristics
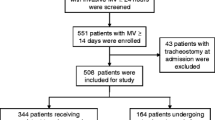
Between May 2002 and September 2004, 61 and 62 patients were enrolled in the ET and PI groups, respectively (Fig. 1) [29]. A questionnaire sent to all the investigators at the end of the study revealed that only 10–20% of the patients assessed for eligibility were actually included. The four main reasons for non inclusion were: difficulties in anticipating MV lasting > 7 days, team reluctance to follow the protocol, difficulties in organising an early tracheotomy, refusal of consent. None of the patients were lost to follow-up.
The characteristics of the 123 patients were similar at ICU admission (Table 1) and at the time of randomisation (ESM). Two-thirds of patients were medical ICU patients, and half of them had two organ failures upon ICU admission.
One of the 61 patients randomised to the ET group died before the tracheotomy. Sixteen of the 62 patients randomised to the PI group had a delayed tracheotomy. Tracheotomies were most often performed at the bedside in the ICU, by intensivists using a surgical technique (ESM).
Outcome measures
Mortality
On d28, 12 patients (20%; 95%CI: 11–31) and 15 patients (24%; 95%CI: 15–36) had died in the ET and PI groups, respectively (Table 2). On d60, 16 patients (27%; 95%CI: 17–39) and 15 patients (24%; 95%CI: 15–36) had died in the ET and PI groups, respectively. Actuarial survival did not differ between the two groups (P = 0.62, Fig. 2), and the hazard ratio (95%CI) of death for ET versus PI was 1.17 (0.63–2.17).
Mechanical ventilation, endotracheal prosthesis
The median (range) duration of MV during the first 28 days was not significantly different at 14 (2–28) and 16 (3–28) days in the ET and PI groups, respectively (ESM Fig. 3). The total duration of MV (Table 2) and the number of accidental extubations were also similar (respectively 5 and 10%).
Infectious complications
Thirty and 31 patients experienced at least one episode of definite or probable pneumonia (day 28 incidence [95% CI]: 67% [49%–81%] and 59% [43%–73%]; median time to occurrence: 17 and 18 days, in the ET and PI groups, respectively). The ICU-acquired pneumonia curves did not differ between the groups [P = 0.94; HR = 0.98 (95%CI: 0.60–1.62)] (ESM, Fig. 4).
The day 28 incidence rates of bloodstream infections [HR = 1.43 (95%CI: 0.68–3.03)] and sinusitis [HR = 0.63 (95%CI: 0.21–1.92)] did not differ between the two groups (Table 2).
Sedation
The level of sedation and amount of sedatives used during the first 28 days was similar in the two groups (Table 2).
Laryngeal and tracheal complications
Early assessment was performed in 85% of the successfully weaned patients (Table 3). Laryngeal symptoms (such as swallowing disorders or dysphonia) and abnormalities at laryngeal examination were not significantly reduced by ET. The only benefit was observed at the time of late assessment (30% of survivors at 2 months), when ET was associated with a significant reduction of laryngeal symptoms (one vs. seven patients, P = 0.01) (ESM).
Comfort
More than half of the surviving and conscious patients (ET group, 23; PI group, 22) completed the self-evaluation questionnaire. Most of the criteria evaluated were in favour of tracheotomy, and all patients who had undergone both trans-laryngeal intubation and early or late tracheotomy considered that the tracheotomy was the most comfortable technique (Table 4). There was no difference regarding time to transfer from bed to chair, oral feeding and speech recovery (Table 4).
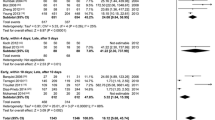
When our results were added to those of the meta-analysis published by Griffiths et al. [7], no benefit could be demonstrated for hospital mortality, incidence of pneumonia and duration of MV (see ESM).
Discussion
This is the first large multicentre randomised trial comparing early tracheotomy and prolonged trans-laryngeal intubation in mechanically ventilated patients. The results (no apparent benefits for mortality, duration of MV and infectious complications) are in accordance with the meta-analysis by Griffiths et al. [7].
This trial however, has a number of limitations. First, despite our best efforts, the study is underpowered, thus precluding definitive conclusions in one direction or another. Recruitment difficulties can be explained by cultural considerations (many investigators were strongly for or against tracheotomy) and the complexity of the study. Only a small proportion of patients fulfilling inclusion criteria were actually included. This led to unavoidable recruitment biases, possibly in favour of patients with a better prognosis, which probably explains the low mortality rate observed; a day 28 mortality rate of 20% instead of the 45% assumed when we computed the sample size. This shows the major difficulties encountered when conducting multicentre ICU RCTs, with a conflict between the need for a large number of patients and the need for detailed data collection.
In addition, although several studies have attempted to define predictive factors [9–12], it proved very difficult to identify patients likely to require MV for >7 days.
Another limitation is that a minority of our patients underwent percutaneous tracheotomy which was not as popular at the time of the study as it is currently.
Finally, the heterogeneity of the study population (medical, surgical, COPD, trauma patients) may have masked subgroup-specific benefits.
Despite these limitations, some points should not be underestimated. First, despite the lack of power, it is noteworthy that our results are consistent with the meta-analysis by Griffiths et al. [7], as suggested by the forest-plots presented in the online supplement. This may be an indication that the very positive results observed by others [5] could have been driven by some specific features of the corresponding study group, hence the need for caution before their generalisation. For example, our results are seemingly different from the results reported by Rumbak et al. [5]. However, as shown in the electronic supplement, there is a marked confidence intervals overlap between the two studies making it impossible to rule out that they represent random variation on the same result.
Second, the premature interruption of our study may not be the main reason for its lack of power. Indeed, based on the accrued mortality rates in our 123 patients, it appears that 2,268 patients would have been required. The low mortality rates we reported considerably reduced the probability of demonstrating any effect of ET on prognosis. As mentioned, this could be explained by stringent selection of patients with a greater likelihood of survival estimated by physicians after 4 days in the ICU. A post hoc analysis of patients who were actually ventilated over 7 days or more, as specified by our inclusion criteria (excluding patients who died rapidly or extubated patients), showed that mortality rates at d28 and d60 remained very similar (P = 0.98).
Third, as in the negative study recently published by the OutcomeRea Study Group [30], our study population was unselected, whereas previous trials showing tracheotomy-associated benefits were mostly conducted in more selected ICU populations: medical [5], burn [31], trauma patients [32, 33], or patients with chronic respiratory insufficiency [34].
Fourth, despite the lack of power, we found a significant benefit of ET regarding late laryngeal symptoms in the subset of patients investigated (Table 3). We also found a significant difference in self-reported comfort in favour of ET, in line with the findings of Nieszkowska et al. [6]. Considering the impact of an ICU stay on quality of life after discharge, and the corresponding psychological consequences [35], such outcomes cannot be considered negligible. Even though the benefits we show regarding laryngeal complications and comfort can hardly be qualified as more than tenuous, they tend to tilt the risk–benefit balance slightly in favour of ET, if anything.
In conclusion, because it is underpowered, this trial does not contribute to the debate about the mortality benefits or lack thereof of early tracheotomy in unselected ICU patients. It hints at putative comfort benefits. Hopefully many of the currently open questions (mortality, but also MV, ICU or hospital duration, or the incidence of nosocomial infections) will find answers in the results of the large “Tracman” trial [36].
References
Maziak DE, Meade MO, Todd TRJ (1998) The timing of tracheotomy. A systematic review. Chest 114:605–609
Blot F, Melot C, Commission d’Epidémiologie et de Recherche Clinique (2005) Indications, timing, and techniques of tracheostomy in 152 French ICUs. Chest 127:1347–1352
Stauffer JL, Olson DE, Petty TL (1981) Complications and consequences of endotracheal intubation and tracheotomy: a prospective study of 150 critically ill adult patients. Am J Med 70:65–76
Diehl JL, El Atrous S, Touchard D, Lemaire F, Brochard L (1999) Changes in the work of breathing induced by tracheotomy in ventilator-dependent patients. Am J Respir Crit Care Med 159:383–388
Rumbak MJ, Newton M, Truncale T, Schwartz SW, Adams JW, Hazard PB (2004) A prospective, randomized, study comparing early percutaneous dilational tracheotomy to prolonged translaryngeal intubation (delayed tracheotomy) in critically ill medical patients. Crit Care Med 32:1689–1694
Nieszkowska A, Combes A, Luyt CE, Ksibi H, Trouillet JL, Gibert C, Chastre J (2005) Impact of tracheotomy on sedative administration, sedation level, and comfort of mechanically ventilated intensive care unit patients. Crit Care Med 33:2527–2533
Griffiths J, Barber VS, Morgan L, Young JD (2005) Systematic review and meta-analysis of studies of the timing of tracheostomy in adult patients undergoing artificial ventilation. BMJ 330:1243–1247
Blot F (2003) A study of early tracheostomy in patients undergoing prolonged mechanical ventilation. Rev Mal Respir 20:411–420
Heffner JE, Zamora CA (1990) Clinical predictors of prolonged translaryngeal intubation in patients with the adult respiratory distress syndrome. Chest 97:447–452
Kollef MH, Ahrens TS, Shannon W (1999) Clinical predictors and outcomes for patients requiring tracheostomy in the intensive care unit. Crit Care Med 27:1714–1720
Troche G, Moine P (1997) Is the duration of mechanical ventilation predictable? Chest 112:745–751
Seneff MG, Zimmerman JE, Knaus WA, Wagner DP, Draper EA (1996) Predicting the duration of mechanical ventilation. The importance of disease and patient characteristics. Chest 110:469–479
Le Gall JR, Lemeshow S, Saulnier F (1993) A new simplified acute physiology score (SAPS II) based on a European/North American multicenter study. JAMA 270:2957–2963
Knaus WA, Draper EA, Wagner DP, Zimmerman JE (1985) Prognosis in acute organ-system failure. Ann Surg 11:685–693
Boles JM, Bion J, Connors A, Herridge M, Marsh B, Melot C, Pearl R, Silverman H, Stanchina M, Vieillard-Baron A, Welte T (2007) Weaning from mechanical ventilation. Eur Respir J 29:1033–1056
Riker RR, Picard JT, Fraser GL (1999) Prospective evaluation of the Sedation-Agitation Scale for adult critically ill patients. Crit Care Med 27:1325–1329
Mac Cabe WR, Jackson GG (1962) Gram negative bacteremia: etiology and ecology. Arch Intern Med 110:847–852
Weinberg PF, Matthay MA, Webster RO, Roskos KV, Goldstein IM, Murray FF (1984) Biologically active products of complement and acute lung injury in patients with the sepsis syndrome. Am Rev Respir Dis 130:791–796
American Thoracic Society (1996) Hospital-acquired pneumonia in adults: diagnosis, assessment of severity, initial antimicrobial therapy, and preventive strategies. A consensus statement, American Thoracic Society, November 1995. Am J Respir Crit Care Med 153:1711–1725
Chastre J, Fagon JY, Soler P, Domart Y, Pierre J, Dombret MC, Gibert C (1989) Quantification of BAL cells containing intracellular bacteria rapidly identifies ventilated patients with nosocomial pneumonia. Chest 95:190S–192S
Chastre J, Viau F, Brun P (1984) Prospective evaluation of the protected specimen brush for the diagnosis of pulmonary infections in ventilated patients. Am Rev Respir Dis 130:924–929
Pham LH, Brun-Buisson C, Legrand P, Rauss A, Verra F, Brochard L, Lemaire F (1991) Diagnosis of nosocomial pneumonia in mechanically ventilated patients. Comparison of a plugged telescoping catheter with the protected specimen brush. Am Rev Respir Dis 143:1055–1061
Marquette CH, Georges H, Wallet F, Ramon P, Saulnier F, Neviere R, Mathieu D, Rime A, Tonnel AB (1993) Diagnostic efficiency of endotracheal aspirates with quantitative bacterial cultures in intubated patients with suspected pneumonia. Comparison with the protected specimen brush. Am Rev Respir Dis 148:138–144
Aegerter P, Auvert B, Buonamico G, Sznajder M, Beauchet A, Guidet B, LeGall JR, Cub-Rea (1998) Organization and quality control of a clinical database on intensive care medicine in central and suburban Paris. Rev Epidemiol Sante Publique 46:226–237
Casagrande JT, Pike MC, Smith PG (1978) An improved approximate formula for calculating sample sizes for comparing two binomial distributions. Biometrics 34:483–486
Kaplan EL, Meier P (1958) Non parametric estimation from incomplete observations. J Am Statist Assoc 53:457–481
Rothman KJ (1978) Estimation of confidence limits for the cumulative probability of survival in life table analysis. J Chronic Dis 31:557–560
Peto R, Pike MC, Armitage P, Breslow NE, Cox DR, Howard SV, Mantel N, McPherson K, Peto J, Smith PG (1977) Design and analysis of randomized clinical trials requiring prolonged observation of each patient. II: analysis and examples. Br J Cancer 35:1–39
Nitenberg G, Laplanche A, Chastre J, Similowski T, Blot F (2005) Early tracheotomy versus prolonged endotracheal intubation in ICU patients. Intensive Care Med 31(Suppl 1):S116
Clec’h C, Alberti C, Vincent F, Garrouste-Orgeas M, de Lassence A, Toledano D, Azoulay E, Adrie C, Jamali S, Zaccaria I, Cohen Y, Timsit JF (2007) Tracheostomy does not improve the outcome of patients requiring prolonged mechanical ventilation: a propensity analysis. Crit Care Med 35:132–138
Saffle JR, Morris SE, Edelman L (2002) Early tracheostomy does not improve outcome in burn patients. J Burn Care Rehabil 23:431–438
Rodriguez JL, Steinberg SM, Luchetti FA, Gibbons KJ, Taheri PA, Flint LM (1990) Early tracheostomy for primary airway management in the surgical critical care setting. Surgery 108:655–659
Bouderka MA, Fakhir B, Bouaggad A, Hmamouchi B, Hamoudi D, Harti A (2004) Early tracheostomy versus prolonged endotracheal intubation in severe head injury. J Trauma 57:251–254
Cracco C, Demoule A, Harb A, Taright N, Lefort Y, Derenne JP, Similowski T (2005) Tracheostomy in intensive care: impact on prognosis and the influence of underlying chronic respiratory insufficiency. Rev Mal Respir 22:751–757
Donchin Y, Seagull J (2002) The hostile environment of the intensive care unit. Curr Opin Crit Care 8:316–320
Tracman. Tracheostomy management in critical care. http://www.tracman.org.uk/
Acknowledgments
TRACHEO trial group. Grant from the Délégation à la Recherche Clinique (PHRC 2002) and ANTADIR (Association fédérative Nationale pour le Traitement A Domicile de l’Insuffisance Respiratoire Chronique). The study was endorsed by the French learned societies for Intensive Care Medicine (Société de Réanimation de Langue Française), Anesthesiology (Société Française d’Anesthésie-Réanimation), and Respiratory Medicine (Société de Pneumologie de Langue Française).
Authors thank Lorna Saint Ange for editing; Anne-Marie Flaux and Dominique Meunier for their outstanding efforts in monitoring and planning the study; Antonella Pinna and Anne-Sophie Veillard for invaluable help in data monitoring; Armelle Morin for secretarial assistance; all the staff members of all the participating hospitals and ICUs who were associated with the study; and the members of the Délégation Régionale à la Recherche Clinique, for their help in conducting the study.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is discussed in the editorial available at: doi:10.1007/s00134-008-1194-5
Electronic supplementary material
Below is the link to the electronic supplementary material.
Appendix
Appendix
List of investigators
Members of the TRACHEO group: Auboyer C, Blot F, Chastre J, Durand-Zaleski I, Holzapfel L, Laplanche A, Nitenberg G, Similowski T, Tenaillon A.
Drs Chardon P, Roustan JP, Capdevila X (Hôpital Lapeyronie, Montpellier); Korach JM (Centre Hospitalier, Chalons-en-Champagne); Costa MA, Vincent F (Hôpital Tenon, AP-HP), Chastre J, Trouillet JL (Groupe Hospitalier Pitié-Salpétrière, AP-HP); Duguet A, Prodanovic H, Demoule A, Similowski T (Groupe Hospitalier Pitié-Salpétrière, AP-HP); Blot F, Raynard B (Institut Gustave Roussy, Villejuif); Frappier J, Journois D (Hôpital Européen Georges Pompidou, AP-HP); Azoulay E, Thiéry G (Hôpital Saint Louis, AP-HP); Fartoukh M, Harb A, Vincent F, Parrot A (Hôpital Tenon, AP-HP); Pipien I, Hammami A, Poirier H (Centre Hospitalier des Quatre Villes, Saint-Cloud); Bruder N (Hôpital Timone, Marseille); Clair B, Orlikowski D, Shashar T, Annane D (Hôpital Raymond Poincaré, AP-HP); Pinsard M, Rigaud JP (Centre Hospitalier, Dieppe); Van de Louw A, Tenaillon A (Centre Hospitalier Sud-Francilien, Evry); Longchal J (Hôpital Intercommunal, Meulan Les Mureaux); Léon A (Centre Hospitalier Universitaire, Reims); Lecomte B, Falcucci D (Centre Hospitalier Notre-Dame de la Miséricorde, Ajaccio); Lamer C, Tric L (Institut Mutualiste Montsouris, Paris); Chassard D (Hôpital Hôtel Dieu, Lyon); Boulle C, Thévenin D (Centre Hospitalier Docteur Schaffner, Lens); Santoli F, Gallaud C, Pallot JL (Centre Hospitalier Intercommunal André Grégoire, Montreuil); Guittard P, Cathala B (Centre Hospitalier Purpan, Toulouse); Dumas R (Hôpital, Freyming-Merlebach); Jaber S (Hôpital Saint-Eloi, Montpellier); Clin O (Centre Hospitalier, Troyes).
Rights and permissions
About this article
Cite this article
Blot, F., Similowski, T., Trouillet, JL. et al. Early tracheotomy versus prolonged endotracheal intubation in unselected severely ill ICU patients. Intensive Care Med 34, 1779–1787 (2008). https://doi.org/10.1007/s00134-008-1195-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-008-1195-4