Abstract
Background
This retrospective study compares tibial component rotations and radiological and functional outcomes in patients who underwent Oxford medial unicompartmental knee arthroplasty (UKA), using the antero-posterior (AP) tibia axis or anterior superior iliac spine (ASIS) as the landmarks for the direction of the vertical cut.
Methods
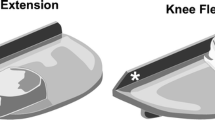
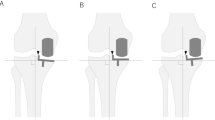
A total of 86 patients, who underwent Oxford medial UKA were divided into 2 groups, each consisting of 43 patients, according to the use of AP axis (group I) or ASIS (group II) as landmarks for the rotation of vertical tibial cut and compared for the radiological and functional outcomes. Tibial component rotations (α-angle), involvement of the posterior cruciate ligament (PCL) fossa, and instant bearing position (IBP) were measured on computed tomography (CT) images. Functional outcomes were evaluated using Oxford knee score (OKS) and Knee Society score (KSS).
Result
The median α‑angle was significantly smaller in group I than group II (2.5°, range −4–5.5° vs. −6°, range −13–0.5°, p < 0.001). The rates of PCL fossa involvements were 14 (32.6%) and 17 (39.5%, p = 0.7). The median flexion angle of the femoral component (7° vs. 10.5°) and posterior tibial slope (6° vs. 8°) were significantly lower in group I than group II (p = 0.001). All other radiological parameters, preoperative and final OKS and KSS were statistically similar in both groups.
Conclusion
Taking the AP tibial axis as a landmark for vertical tibial cut rotation provides more neutral tibial component rotation in Oxford medial UKA compared to ASIS; however, this difference may not influence the clinical outcomes.
Zusammenfassung
Hintergrund
Diese retrospektive Studie vergleicht die Rotation der Tibiakomponente sowie die radiologischen und funktionellen Ergebnisse bei Patienten, die eine mediale unikondyläre Knieendoprothese (Oxford-Schlittenprothese) am Kniegelenk erhalten hatten, wobei die anteroposteriore Tibiaachse oder die Spina iliaca anterior superior (SIAS) als Orientierungspunkt für die Richtung des vertikalen Schnitts verwendet wurde.
Methoden
Insgesamt 86 Patienten, die eine mediale unikondyläre Schlittenprothese erhalten hatten, wurden in 2 Gruppen mit jeweils 43 Patienten unterteilt, je nachdem, ob die a.-p.-Achse (Gruppe I) oder die SIAS (Gruppe II) als Orientierungspunkt für die Rotation des vertikalen Tibiaschnitts verwendet wurde, und hinsichtlich der radiologischen und funktionellen Ergebnisse verglichen. Die Rotation der Tibiakomponente (α-Winkel), die Beteiligung der Fossa des hinteren Kreuzbands (HKB) und die sofortige Lagerposition („instant bearing position“ [IBP]) wurden auf CT-Bildern gemessen. Die funktionellen Ergebnisse wurden mit dem Oxford Knie Score (OKS) und dem Knee Society Score (KSS) bewertet.
Ergebnis
Der mediane α‑Winkel war in Gruppe I signifikant kleiner als in Gruppe II (2,5°, Range: −4 bis 5,5° vs. −6°, Range: −13 bis 0,5°; p < 0,001). Die Raten der HKB-Fossa-Beteiligung betrugen 14 (32,6 %) und 17 (39,5 %; p = 0,7). Der mediane Flexionswinkel der femoralen Komponente (7 vs. 10,5) und die posteriore tibiale Neigung (6 vs. 8) waren in Gruppe I signifikant geringer als in Gruppe II (p = 0,001). Alle anderen radiologischen Parameter sowie der präoperative und endgültige OKS und KSS waren in beiden Gruppen statistisch ähnlich.
Schlussfolgerung
Bei der medialen unikondylären Oxford-Schlittenprothese führt die Verwendung der a.-p.-Tibiaachse als Orientierungspunkt für die vertikale Rotation des Tibiaschnitts zu einer neutraleren Rotation der Tibiakomponente im Vergleich zur SIAS; dieser Unterschied hat jedoch möglicherweise keinen Einfluss auf das klinische Outcome.






Similar content being viewed by others
References
Akagi M, Oh M, Nonaka T, Tsujimoto H, Asano T, Hamanishi C (2004) An anteroposterior axis of the tibia for total knee arthroplasty. Clin Orthop Relat Res 420:213–219
Barbadoro P, Ensini A, Leardini A et al (2014) Tibial component alignment and risk of loosening in unicompartmental knee arthroplasty: a radiographic and radiostereometric study. Knee Surg Sports Traumatol Arthrosc 22(12):3157–3162
Berger RA, Della Valle CJ (2010) Unicompartmental knee arthroplasty: indications, techniques, and results. Instr Course Lect 59:47–56
Clarius M, Haas D, Aldinger PR, Jaeger S, Jakubowitz E, Seeger JB (2010) Periprosthetic tibial fractures in unicompartmental knee arthroplasty as a function of extended sagittal saw cuts: an experimental study. Knee 17(1):57–60
Emerson RH Jr., Hansborough T, Reitman RD, Rosenfeldt W, Higgins LL (2002) Comparison of a mobile with a fixed-bearing unicompartmental knee implant. Clin Orthop Relat Res 404:62–70
Iriberri I, Aragon JF (2014) Alignment of the tibial component of the unicompartmental knee arthroplasty, assessed in the axial view by CT scan: does it influence the outcome? Knee 21(6):1269–1274
Kamenaga T, Hiranaka T, Hida Y, Fujishiro T, Okamoto K (2019) Rotational position of the tibial component can decrease bony coverage of the tibial component in Oxford mobile-bearing unicompartmental knee arthroplasty. Knee 26(2):459–465
Kamenaga T, Hiranaka T, Kikuchi K, Hida Y, Fujishiro T, Okamoto K (2018) Influence of tibial component rotation on short-term clinical outcomes in Oxford mobile-bearing unicompartmental knee arthroplasty. Knee 25(6):1222–1230
Kamenaga T, Hiranaka T, Takayama K, Tsubosaka M, Kuroda R, Matsumoto T (2019) Adequate positioning of the tibial component is key to avoiding bearing impingement in oxford unicompartmental knee arthroplasty. J Arthroplasty 34(11):2606–2613
Kawahara S, Matsuda S, Okazaki K, Tashiro Y, Iwamoto Y (2012) Is the medial wall of the intercondylar notch useful for tibial rotational reference in unicompartmental knee arthroplasty? Clin Orthop Relat Res 470(4):1177–1184
Kendrick BJ, Simpson DJ, Kaptein BL et al (2011) Polyethylene wear of mobile-bearing unicompartmental knee replacement at 20 years. J Bone Joint Surg Br 93(4):470–475
Khanna G, Levy BA (2007) Oxford unicompartmental knee replacement: literature review. Orthopedics 30(5):11–14
Kristensen PW, Holm HA, Varnum C (2013) Up to 10-year follow-up of the Oxford medial partial knee arthroplasty—695 cases from a single institution. J Arthroplasty 28(9):195–198
Lee SY, Bae JH, Kim JG et al (2014) The influence of surgical factors on dislocation of the meniscal bearing after Oxford medial unicompartmental knee replacement: a case-control study. Bone Joint J 96(7):914–922
Lee SY, Chay S, Lim HC, Bae JH (2017) Tibial component rotation during the unicompartmental knee arthroplasty: is the anterior superior iliac spine an appropriate landmark? Knee Surg Sports Traumatol Arthrosc 25(12):3723–3732
Lee YS, Yun JY, Lee BK (2014) Tibial component coverage based on bone mineral density of the cut tibial surface during unicompartmental knee arthroplasty: clinical relevance of the prevention of tibial component subsidence. Arch Orthop Trauma Surg 134(1):85–89
Liow MH, Tsai TY, Dimitriou D, Li G, Kwon YM (2016) Does 3‑dimensional in vivo component rotation affect clinical outcomes in unicompartmental knee arthroplasty? J Arthroplasty 31(10):2167–2172
Murray DW, Goodfellow JW, O’Connor JJ (1998) The Oxford medial unicompartmental arthroplasty: a ten-year survival study. J Bone Joint Surg Br 80(6):983–989
Nicoll D, Rowley DI (2010) Internal rotational error of the tibial component is a major cause of pain after total knee replacement. J Bone Joint Surg Br 92(9):1238–1244
Pandit H, Jenkins C, Gill HS, Barker K, Dodd CA, Murray DW (2011) Minimally invasive Oxford phase 3 unicompartmental knee replacement: results of 1000 cases. J Bone Joint Surg Br 93(2):198–204
Peersman G, Stuyts B, Vandenlangenbergh T, Cartier P, Fennema P (2015) Fixed- versus mobile-bearing UKA: a systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc 23(11):3296–3305
Price AJ, Webb J, Topf H, Dodd CA, Goodfellow JW, Murray DW (2001) Rapid recovery after oxford unicompartmental arthroplasty through a short incision. J Arthroplasty 16(8):970–976
Robertsson O, Knutson K, Lewold S, Lidgren L (2001) The routine of surgical management reduces failure after unicompartmental knee arthroplasty. J Bone Joint Surg Br 83(1):45–49
Scott RD (2010) Mobile- versus fixed-bearing unicompartmental knee arthroplasty. Instr Course Lect 59:57–60
Servien E, Fary C, Lustig S et al (2011) Tibial component rotation assessment using CT scan in medial and lateral unicompartmental knee arthroplasty. Orthop Traumatol Surg Res 97(3):272–275
Sloper PJ, Hing CB, Donell ST, Glasgow MM (2003) Intra-operative tibial plateau fracture during unicompartmental knee replacement: a case report. Knee 10(4):367–369
Smith TO, Hing CB, Davies L, Donell ST (2009) Fixed versus mobile bearing unicompartmental knee replacement: a meta-analysis. Orthop Traumatol Surg Res 95(8):599–605
Svärd UC, Price AJ (2001) Oxford medial unicompartmental knee arthroplasty. A survival analysis of an independent series. J Bone Joint Surg Br 83(2):191–194
Tsukamoto I, Akagi M, Mori S, Inoue S, Asada S, Matsumura F (2017) Anteroposterior rotational references of the tibia for medial unicompartmental knee arthroplasty in Japanese patients. J Arthroplasty 32(10):3169–3175
White SH, Ludkowski PF, Goodfellow JW (1991) Anteromedial osteoarthritis of the knee. J Bone Joint Surg Br 73(4):582–586
Yoshida K, Tada M, Yoshida H, Takei S, Fukuoka S, Nakamura H (2013) Oxford phase 3 unicompartmental knee arthroplasty in Japan—clinical results in greater than one thousand cases over ten years. J Arthroplasty 28(9):168–171
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
O. Aliyev, M. Ağır, A. Aghazada, D.H. Çeşme, D. Kara, A. Toprak, İ. Tuncay, and F. Yıldız declare that they have no competing interests.
Ethical standards.
All studies mentioned were in accordance with the ethical standards indicated in each case.
Additional information
Level of evidence
Level III therapeutic

Scan QR code & read article online
Rights and permissions
About this article
Cite this article
Aliyev, O., Ağır, M., Aghazada, A. et al. Antero-posterior axis of the tibia is a better landmark for tibial component rotation in Oxford medial unicompartmental knee arthroplasty. Orthopädie 51, 996–1002 (2022). https://doi.org/10.1007/s00132-022-04308-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00132-022-04308-8