Abstract
Purpose
The MAKASI intervention aimed to empower Sub-Saharan African immigrants living in precarious situations in the Paris metropolitan area. Because there are factors specifically related to immigration that may increase the risk for common mental disorders, the present study aimed to examine participants’ levels of depression and loneliness and analyze the effect of the intervention on depression and loneliness.
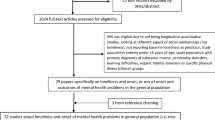
Methods
The MAKASI study was designed as a stepped wedge cluster randomized trial. Study participants were recruited through an outreach program led by a nongovernmental organization and randomly assigned to two clusters, with an intervention delay of 3 months between them. Participants were assessed for 6 months after inclusion and the effect of the intervention on depression and loneliness was assessed using generalized linear mixed models. The study was conducted from 2018 to 2021 and took in consideration whether being interviewed during one of the Covid-19 confinement had an effect on the results.
Results
Between 2018 and 2021 a total of 821 subjects participated in the Makasi study. High levels of depression and loneliness were found in the study population. We found no effect of the intervention on depression [95% CI 0.77 to 2.40]. Similarly, no effect of the intervention was found on loneliness [95% CI 0.87 to 2.54].
Conclusions
The intervention tested did not appear to improve the level of depression and loneliness among participants. However, the high prevalence of mental and emotional problems in the study population suggests a public health crisis among immigrants in the greater Paris area.
Clinical Trial Registration Number: Trial registration Clinicaltrials.gov, NCT04468724 (July 13, 2020).




Similar content being viewed by others
Data availability
Data requests will be reviewed internally and will be available subject to a written proposal and a signed data sharing agreement.
Notes
Intervention sites in Paris greater area: Rosa Parks, Marcadet, Château Rouge, Flandres, Montreuil, Aubervilliers, Sevran Beaudottes, Saint Denis, Sarcelles, Pierrefitte-Stains and Gare de Grigny.
References
-McAuliffe M, Khadria B (2020) World Migration Report 2020. https://publications.iom.int/system/files/pdf/wmr_2020.pdf. Accessed 2 Jan 2023.
- Institut national de la statistique et des études économiques (2022) L’essentiel sur... les immigrés et les étrangers [The essentials about... immigrants and foreigners]. https://www.insee.fr/fr/statistiques/3633212. Accessed 2 Jan 2023.
- Beauchemin, C (2020) Profil démographique des personnes d’origine subsaharienne en France : Etude pour la Chaire ”Diasporas Africaines” [Demographic profile of people of sub-Saharan origin in France: Study for the “African Diasporas”]. https://hal.science/hal-03097531
World Health Organization (2018) Report on the Health of refugees and migrants in the WHO European Region. No public health without refugee and migrant health. World Health Organization. Regional Office for Europe 1–114 p. https://apps.who.int/iris/bitstream/handle/10665/311347/9789289053846-eng.pdf?sequence=1&isAllowed=y
Löbel L, Kröger H, Tibubos A (2021) Social isolation and loneliness in the context of migration: a cross-sectional study of refugees, migrants, and the native population in Germany. SOEPpapers on SOEPpapers Multidiscip Panel Data Res 1124:1–82
Kroenke K, Spitzer RL, Williams JBW (2001) The PHQ-9: validity of a brief depression measure. J Gen Intern Med 16:606–613. https://doi.org/10.1046/j.1525-1497.2001.016009606.x
World Health Organization (2021) Depression. https://www.who.int/news-room/fact-sheets/detail/depression. Accessed 2 Jan 2023.
Fond G, Lancon C, Auquier P, Boyer L (2019) Prévalence de la dépression majeure en France en population générale et en populations spécifiques de: une revue systématique de la littérature.[ Prevalence of major depression in France in the general population and in specific populations from 2000 to 2018: a systematic review of the literature]. La Presse Médicale 48(4):365–375. https://doi.org/10.1016/j.lpm.2018.12.004
Close C, Kouvonen A, Bosqui T, Patel K, O’Reilly D, Donnelly M (2016) The mental health and wellbeing of first generation migrants: a systematic-narrative review of reviews. Glob Health 12(1):47. https://doi.org/10.1186/s12992-016-0187-3
Grupp F, Piskernik B, Mewes R (2020) Is depression comparable between asylum seekers and native Germans? an investigation of measurement invariance of the PHQ-9. J Affect Disord 1(262):451–458. https://doi.org/10.1016/j.jad.2019.11.055
Pannetier J, Lert F, Jauffret Roustide M, du Loû AD (2017) Mental health of sub-saharan african migrants: the gendered role of migration paths and transnational ties. SSM - Popul Health 1(3):549–557. https://doi.org/10.1016/j.ssmph.2017.06.003
Salami B, Yaskina M, Hegadoren K, Diaz E, Meherali S, Rammohan A et al (2017) Migration and social determinants of mental health: results from the Canadian health measures survey. Can J Public Health 108(4):362–7. https://doi.org/10.17269/cjph.108.6105
World Health Organization. (2008). The global burden of disease : 2004 update. World Health Organization. https://apps.who.int/iris/handle/10665/43942. Accessed 2 Jan 2023.
Carroll H, Luzes M, Freier LF, Bird MD (2020) The migration journey and mental health: evidence from Venezuelan forced migration. SSM - Popul Health 1:10. https://doi.org/10.1016/j.ssmph.2020.100551
Sangalang CC, Becerra D, Mitchell FM, Lechuga-Peña S, Lopez K, Kim I (2019) Trauma, post-migration stress, and mental health: a comparative analysis of refugees and immigrants in the United States. J immigr minor health 21(5):909–919. https://doi.org/10.1007/s10903-018-0826-2
Scarlett H, Davisse-Paturet C, Longchamps C, El Aarbaoui T, Allaire C, Colleville A, Convence-Arulthas M, Crouzet L, Ducarroz S, Melchior M (2021) Depression during the COVID-19 pandemic amongst residents of homeless shelters in France. J affect disord reports 6:100243. https://doi.org/10.1101/2021.04.23.21255993
Fierloos IN, Tan SS, Williams G, Alhambra-Borrás T, Koppelaar E, Bilajac L et al (2021) Socio-demographic characteristics associated with emotional and social loneliness among older adults. BMC Geriatr 21(1):114. https://doi.org/10.1186/s12877-021-02058-4
Baarck J, Balahur-Dobrescu A, Cassio L, D`hombres B, Pasztor Z, Tintori G (2021) Loneliness in the EU. Insights from surveys and online media data. Publications Office of the European Union. https://publications.jrc.ec.europa.eu/repository/handle/JRC125873. Accessed 2 Jan 2023.
Holt-Lunstad J (2017) The potential public health relevance of social isolation and loneliness: prevalence, epidemiology, and risk factors. Public Policy Aging Rep 27(4):127–130. https://doi.org/10.1093/ppar/prx030
Masi C, Chen H, Hawkley L, Cacioppo J (2010) A meta-analysis of interventions to reduce loneliness. Personal Soc Psychol Rev 15(3):219–266. https://doi.org/10.1177/1088868310377394
Hertz N (2020) The lonely century: coming together in a world that’s pulling apart. Sceptre, p 352
Kraav S, Lehto S, Junttila N, Ruusunen A, Kauhanen J, Hantunen S et al (2021) Depression and loneliness may have a direct connection without mediating factors. Nordi J Psychiatr 75(7):553–557. https://doi.org/10.1080/08039488.2021.1894231
Gosselin A, Carillon S, Coulibaly K, Ridde V, Taéron C, Kohou V et al (2019) Participatory development and pilot testing of the makasi intervention: a community based outreach intervention to improve sub-saharan and caribbean immigrants’ empowerment in sexual health. BMC Public Health 19(1):1–10. https://doi.org/10.1186/s12889-019-7943-2
Mufson L, Morrison C, Shea E, Kluisza L, Robbins R, Chen Y et al (2022) Screening for depression with the PHQ-9 in young adults affected by HIV. J affect disord 297:276–282. https://doi.org/10.1016/j.jad.2021.10.037
Ninacs WA. Empowerment: cadre conceptuel et outil d’évaluation de l’intervention sociale et communau- taire. [Empowerment: conceptual framework and evaluation tool for social and community intervention] Clé Coop Consult En Dév. 2003;26.
Brown CA, Lilford RJ (2006) The stepped wedge trial design: a systematic review. BMC Med Res Methodol 6:54. https://doi.org/10.1186/1471-2288-6-54
Li YH, Mullette E, Brant JM (2018) The stepped-wedge trial design: paving the way for cancer care delivery research. J Adv Pract Oncol 9(7):722–727. https://doi.org/10.6004/jadpro.2018.9.7.3. (Epub 2018 Nov 1)
Hussey MA, Hughes JP (2007) Design and analysis of stepped wedge cluster randomized trials. Contemp Clin Trials 28(2):182–191. https://doi.org/10.1016/j.cct.2006.05.007
Costantini L, Pasquarella C, Odone A, Colucci ME, Costanza A, Serafini G, Aguglia A, Belvederi MM, Brakoulias V, Amore M, Ghaemi SN, Amerio A (2021) Screening for depression in primary care with patient health questionnaire-9 (PHQ-9): a systematic review. J affect disord 279:473–483. https://doi.org/10.1016/j.jad.2020.09.131
American Psychiatric Association (2013). Diagnostic and statistical manual of mental disorders (5th ed.). https://doi.org/10.1176/appi.books.9780890425596
Levis B, Benedetti A, Thombs BD (2019) Accuracy of patient health questionnaire-9 (PHQ-9) for screening to detect major depression: individual participant data meta-analysis. BMJ 365:l1476. https://doi.org/10.1136/bmj.l1476
Carballeira Y, Dumont P, Borgacci S, Rentsch D, de Tonnac N, Archinard M, Andreoli A (2007) Criterion validity of the french version of patient health questionnaire (PHQ) in a hospital department of internal medicine. Psychol psychother 80(Pt 1):69–77. https://doi.org/10.1348/147608306X103641
Gelaye B, Williams MA, Lemma S, Deyessa N, Bahretibeb Y, Shibre T, Wondimagegn D, Lemenhe A, Fann JR, Vander Stoep A, Andrew Zhou XH (2013) Validity of the patient health questionnaire-9 for depression screening and diagnosis in East Africa. Psychiatr Res 210(2):653–661. https://doi.org/10.1016/j.psychres.2013.07.015
Cholera R, Gaynes BN, Pence BW, Bassett J, Qangule N, Macphail C, Bernhardt S, Pettifor A, Miller WC (2014) Validity of the patient health questionnaire-9 to screen for depression in a high-HIV burden primary healthcare clinic in Johannesburg, South Africa. J Affect Disord 167:160–166. https://doi.org/10.1016/j.jad.2014.06.003
Monahan PO, Shacham E, Reece M, Kroenke K, Ong’or WO, Omollo O, Yebei VN, Ojwang C (2009) Validity/reliability of PHQ-9 and PHQ-2 depression scales among adults living with HIV/AIDS in western Kenya. J Gen Intern Med 24(2):189–197. https://doi.org/10.1007/s11606-008-0846-z
Huang FY, Chung H, Kroenke K, Delucchi KL, Spitzer RL (2006) Using the patient health questionnaire-9 to measure depression among racially and ethnically diverse primary care patients. J Gen Intern Med 21(6):547–552. https://doi.org/10.1111/j.1525-1497.2006.00409.x
Kleiman, E (2017). Understanding and analyzing multilevel data from real-time monitoring studies: An easily- accessible tutorial using R. https://doi.org/10.31234/osf.io/xf2pw
Nickless A, Voysey M, Geddes J, Yu LM, Fanshawe TR (2018) Mixed effects approach to the analysis of the stepped wedge cluster randomised trial-Investigating the confounding effect of time through simulation. PLoS ONE 13(12):e0208876. https://doi.org/10.1371/journal.pone.0208876
Coll-Planas L, del Valle Gómez G, Bonilla P, Masat T, Puig T, Monteserin R (2017) Promoting social capital to alleviate loneliness and improve health among older people in Spain. Health Soc Care Community 25(1):145–157
Johanson S, Bejerholm U (2017) The role of empowerment and quality of life in depression severity among unemployed people with affective disorders receiving mental healthcare. Disabil Rehabil 39(18):1807–1813. https://doi.org/10.1080/09638288.2016.1211758
Winters M, Rechel B, de Jong L, Pavlova M (2018) A systematic review on the use of healthcare services by undocumented migrants in Europe. BMC Health Serv Res 18(1):30. https://doi.org/10.1186/s12913-018-2838-y. (ISSN 1472-6963)
Lebano A, Hamed S, Bradby H, Gil-Salmerón A, Durá-Ferrandis E, Garcés-Ferrer J et al (2020) Migrants’ and refugees’ health status and healthcare in Europe: a scoping literature review. BMC Public Health 20:1039. https://doi.org/10.1186/s12889-020-08749-8
Turrini G, Purgato M, Acarturk C, Anttila M, Au T, Ballette F et al (2019) Efficacy and acceptability of psychosocial interventions in asylum seekers and refugees: systematic review and meta-analysis. Epidemiol Psychiatr Sci 28(4):376–388. https://doi.org/10.1017/S2045796019000027
Orang TM, Missmahl TAM, Valensise L, Brenner A, Gardisi M, Peter H, Kluge U (2022) New directions in the mental health care of migrants, including refugees-a randomized controlled trial investigating the efficacy of value-based counselling. Clin Psychol Psychother 29(4):1433–1446. https://doi.org/10.1002/cpp.2728
Bousmah MQ, Gosselin A, Coulibaly K, Ravalihasy A, Desgrées du Loû A (2022) Health empowerment and access to health coverage among immigrants in France: the Makasi intervention. Eur J Public Health. https://doi.org/10.1093/eurpub/ckac129.457
Bousmah MQ, Gosselin A, Coulibaly K, Ravalihasy A, Taéron C, Senne JN, Gubert F, Desgrées du Loû A, MAKASI Study Group (2023) Immigrants’ health empowerment and access to health coverage in France: a stepped wedge randomised controlled trial. Soc Sci Med 339:116400. https://doi.org/10.1016/j.socscimed.2023.116400
Lanfredi M, Zoppei S, Ferrari C, Bonetto C, Van Bortel T, Thornicroft G, Knifton L, Quinn N, Rossi G, Lasalvia A, ASPEN Study group (2015) Self-stigma as a mediator between social capital and empowerment among people with major depressive disorder in Europe: the ASPEN study. Eur Psychiatry J Assoc Eur Psychiatri 30(1):58–64. https://doi.org/10.1016/j.eurpsy.2014.06.002
Schwartz CE, Rohde G, Biletch E, Stuart RBB, Huang I-C, Lipscomb J et al (2022) If it’s information, it’s not “bias”: a scoping review and proposed nomenclature for future response-shift research. Qual Life Res Int J Qual Life Asp Treat Care And Rehabil 31(8):2247–2257. https://doi.org/10.1007/s11136-021-03023-9
Vanier A, Frans OJ, Mcclimans L, Ow N, Gulek BG et al (2021) Response shift in patient-reported outcomes: definition, theory, and a revised model. Qual Life Res Int J Qual Life Asp Treat Care Rehabil 30(12):3309–3322. https://doi.org/10.1007/s11136-021-02846-w
Christodoulou P (2014) This is how it feels to be lonely. The Forum. http://migrantsorganise.org/wp-content/uploads/2014/09/Loneliness-report_The-Forum_UPDATED.pdf. Accessed 2 Jan 2023.
Ehsan A, Bolano D, Guillaume-Boeckle S, Spini D (2020) Reducing loneliness in older adults: looking at locals and migrants in a Swiss case study. Eur J Ageing 18(3):333–344. https://doi.org/10.1007/s10433-020-00577-4
Lai DWL, Li J, Ou X, Li CYP (2020) Effectiveness of a peer-based intervention on loneliness and social isolation of older Chinese immigrants in Canada: a randomized controlled trial. BMC Geriatr 20:356. https://doi.org/10.1186/s12877-020-01756-9
Saito T, Kai I, Takizawa A (2012) Effects of a program to prevent social isolation on loneliness, depression, and subjective well-being of older adults: a randomized trial among older migrants in Japan. Arch Gerontol Geriatr 55(3):539–547. https://doi.org/10.1016/j.archger.2012.04.002
Ettman CK, Abdalla SM, Cohen GH, Sampson L, Vivier PM, Galea S (2020) Prevalence of depression symptoms in US adults before and during the COVID-19 pandemic. JAMA Netw Open 3(9):e2019686. https://doi.org/10.1001/jamanetworkopen.2020.19686
Gosselin A, Melchior M, Carillon S, Gubert F, Ridde V, Kohou V et al (2021) Deterioration of mental health and insufficient Covid-19 information among disadvantaged immigrants in the greater Paris area. J Psychosom Res 146:110504. https://doi.org/10.1016/j.jpsychores.2021.110504
Varga TV, Bu F, Dissing AS, Elsenburg LK, Bustamante JJH, Matta J, van Zon SKR, Brouwer S, Bültmann U, Fancourt D et al (2021) Loneliness, worries, anxiety, and precautionary behaviours in response to the COVID-19 pandemic: a longitudinal analysis of 200,000 Western and Northern Europeans. Lancet Reg Health Eur 2:100020. https://doi.org/10.1016/j.lanepe.2020.100020
Luchetti M, Lee JH, Aschwanden D, Sesker A, Strickhouser JE, Terracciano A, Sutin AR (2020) The trajectory of loneliness in response to COVID-19. Am Psychol 75(7):897–908. https://doi.org/10.1037/amp0000690
Rothman K, Greenland S (1998) Modern Epidemiology, 2nd edn. Lippincott Williams & Wilkins
Acknowledgements
This study was supported by the French National Agency for research on AIDS and Viral hepatitis (ANRS) and Health regional agency (ANRS 14057). The sponsor of the study had no role in study design, data collection, data analysis, data interpretation or writing of the paper. We would also like to thank the contributions given by Véronique Sébille and Myriam Blanchin from Nantes University. The MAKASI Study Group included Annabel Desgrées du Loû, Nicolas Derche, Flore Gubert, Romain Mbiribindi, Maria Melchior (scientific coordinators), Ny Sata Andrianirina, Marwân-al-Qays Bousmah, Séverine Carillon, Virginie Comblon, Karna Coulibaly, Angèle Delbe, Jacques Ebongue, Ruth Foundje Notemi, Charles Gaywahali, Anne Gosselin, Veroska Kohou, France Lert, Jean Lusilu-Voza, Belinda Lutonadio, Yves Nyemeck, Patricia Mbiribindi, Thierry Miatti, Jean-Paul Ngueya, Andrainolo Ravalihasy, Valéry Ridde, Jean-Noël Senne, Oumar Sissoko, Corinne Taéron, Faya Tess, and Iris Zoumenouand the Makasi group of peers.
Funding
The MAKASI study received funding from the French National Agency of Research on HIV/Aids and Viral Hepatitis (ANRS). The mentioned sponsor did not participate in the elaboration, data collection or analysis of the study.
Author information
Authors and Affiliations
Consortia
Contributions
ADDL was responsible for securing the funding for the study. ADDL and MM designed the study. ADDL, AG, KC, MQB and AR collected and prepared the data. BGT, MQB and KC conducted statistical analysis. BGT conducted the literature review and wrote the first draft of the paper. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no competing interests concerning the present study.
Ethical approval
The MAKASI study was performed in line with the principles of the Declaration of Helsinki. This study was approved by the French Data Protection Authority (Commission Nationale de l’Informatique et des Libertés, CNIL, declaration n°2215270) and the Committee for Persons’ Protection (Comité de protection des personnes, ID RCB 2018-A02129-46). Written informed consent was obtained from all participants.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Additional information
The Members of the Makasi Study Group are listed in Acknowledgements.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gonçalves Tasca, B., Bousmah, MaQ., Coulibaly, K. et al. Depression and loneliness among Sub-Saharan immigrants living in the greater Paris area: results from the MAKASI empowerment stepped wedge cluster randomised controlled trial. Soc Psychiatry Psychiatr Epidemiol (2024). https://doi.org/10.1007/s00127-024-02665-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00127-024-02665-7