Abstract
Aims/hypothesis
This study aimed to assess the use of ambulatory BP monitoring (ABPM) to identify the presence of masked, nocturnal and white-coat hypertension in individuals with type 1 diabetes, patterns that could not be detected by regular office-based BP monitoring alone. We also analysed associations between BP patterns and arterial stiffness in order to identify individuals at cardiovascular risk.
Methods
This substudy included 140 individuals with type 1 diabetes from the Helsinki metropolitan area, who attended the Finnish Diabetic Nephropathy Study (FinnDiane) Centre in Helsinki between January 2013 and August 2017. Twenty-four hour ABPM and pulse wave analysis were performed simultaneously using a validated non-invasive brachial oscillometric device (Mobil-O-Graph). Definitions of hypertension were based on the European Society of Hypertension guidelines. Masked hypertension was defined as normal office BP (BP obtained using a standardised automated BP device) but elevated 24 h ABPM, and white-coat hypertension as elevated office BP but normal 24 h ABPM.
Results
A total of 38% of individuals were normotensive and 33% had sustained hypertension, while 23% had masked and 6% had white-coat hypertension. About half of the cohort had increased absolute levels of night-time BP, half of whom were untreated. In the ambulatory setting, central BP and pulse wave velocity (PWV) were higher in participants with masked hypertension than in those with normotension (p ≤ 0.001). In a multivariable linear regression model adjusted for age, sex, BMI, antihypertensive treatment and eGFR, masked hypertension was independently associated with higher 24 h PWV (β 0.50 [95% CI 0.34, 0.66]), but not with PWV obtained during resting conditions (adjusted β 0.28 [95% CI −0.53, 1.10]), using normotension as the reference group.
Conclusions/interpretation
ABPM analysis revealed that one-quarter of the participants with type 1 diabetes had masked hypertension; these individuals would not have been detected by office BP alone. Moreover, arterial stiffness was increased in individuals with masked hypertension. These findings support the use of ABPM to identify individuals at risk of cardiovascular disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.

Introduction
Hypertension is a major risk factor for microvascular complications and cardiovascular disease in individuals with type 1 diabetes [1, 2]. We recently reported that elevated BP and suboptimal antihypertensive drug regimens are common in type 1 diabetes [3]. Our results were, however, based on office-based BP values (herein referred to as ‘office BP’; obtained using a standardised automated BP device), which are often used in the management of hypertension in clinical practice. However, office BP alone does not reflect the real diurnal BP variation, and cannot exclude disturbed BP patterns such as masked, nocturnal or white-coat hypertension [4]. Therefore, ambulatory BP monitoring (ABPM) might be more accurate than clinical BP measurement; it allows the detection of nocturnal BP and dipping patterns, and can reduce false-positive results by detecting white-coat hypertension, and false-negative results by detecting masked hypertension [5]. Indeed, several studies have shown the superiority of ABPM over office- or home-based BP monitoring to detect hypertension and predict cardiovascular outcomes [6, 7].
There is strong evidence that individuals with masked hypertension have an increased prevalence of target organ damage, more frequently unfavourable metabolic profiles and a higher risk of cardiovascular events than those who are normotensive [8, 9]. Notably, the prevalence of masked hypertension is higher in individuals with diabetes than in those without, and also higher in individuals treated with antihypertensives than in untreated individuals [10]. This suggests that current treatment regimens may be too focused on normalising office BP rather than targeting daily BP patterns [10].
Increased arterial stiffness reflects structural and functional changes that precede manifest hypertension and cardiovascular events [11]. This phenomenon, known as early vascular ageing, is evident in individuals with type 1 diabetes and is associated with elevated BP and vascular complications [12,13,14,15]. Notably, very few studies have analysed the association between masked hypertension and markers of arterial stiffness in individuals with diabetes [16]. However, a new cuff-based validated oscillometric Mobil-O-Graph device (I.E.M., Stolberg, Germany) now allows simultaneous monitoring of peripheral BP and markers of arterial stiffness during ambulatory conditions, such as daily activities and sleep [17].
Therefore, the aim of the study was to estimate the prevalence of masked, nocturnal, white-coat and sustained hypertension in individuals with type 1 diabetes, and to examine the association between disturbed BP patterns and determinants of arterial stiffness during ambulatory conditions.
Methods
The study is part of the nationwide, multicentre, ongoing Finnish Diabetic Nephropathy Study (FinnDiane), the main aim of which is to identify genetic, clinical and environmental risk factors for diabetic complications among individuals with type 1 diabetes. Baseline and prospective FinnDiane visits were carried out according to the same protocol and took place in conjunction with a regular visit to their attending physician. A more detailed description of the study has been reported elsewhere [3, 18]. In this substudy, individuals with type 1 diabetes from the Helsinki metropolitan area who attended the FinnDiane study centre in Helsinki were asked to undergo 24 h ABPM measurement either at the baseline or at a prospective FinnDiane visit (from January 2013 until August 2017). This substudy comprises a total of 140 participants with type 1 diabetes who successfully completed 24 h ABPM and simultaneous ambulatory pulse wave analysis (PWA) with the Mobil-O-Graph device. Type 1 diabetes was defined by age at onset of diabetes <40 years, C-peptide ≤0.3 nmol/l and insulin treatment initiated within 1 year of the diagnosis of diabetes. Written informed consent was obtained from each participant. The study protocol was approved by the Ethics Committee of the Helsinki and Uusimaa Health District, and the study was carried out in accordance with the Declaration of Helsinki.
As part of the FinnDiane protocol, all individuals underwent a clinical examination that included blood and urine sampling. Details of the participants’ clinical characteristics were obtained from the medical records by the attending physician using a standardised questionnaire. Each participant also completed a detailed questionnaire on lifestyle, smoking habits and family history. The measurements of height, weight and waist and hip circumferences were performed with the participant in light clothing. Office BP was measured twice at 2 min intervals in the sitting position after a 10 min rest using a standardised automated BP device (Omron M6; Omron Healthcare, Kyoto, Japan). The mean of these two measurements was calculated. Blood samples were drawn and analysed for HbA1c, serum creatinine and lipids. GFR was estimated using the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) formula [19]. Nephropathy status was defined on the basis of the urinary AER in at least two out of three overnight or 24 h urine collections. Normal AER was defined as an AER of <20 μg/min or <30 mg/24 h; microalbuminuria as an AER of 20–200 μg/min or 30–300 mg/24 h; and macroalbuminuria as an AER of >200 μg/min or >300 mg/24 h. The fourth group consisted of participants with end-stage renal disease (ESRD).
Both ABPM and PWA were performed simultaneously over 24 h using the oscillometric Mobil-O-Graph device, which has been validated against invasive and non-invasive reference methods [20,21,22]. BP readings were recorded using an upper arm BP cuff (with appropriate cuff size) every 15 min during the day (07:00–22:00 hours) and every 30 min at night (22:00–07:00 hours). During monitoring, participants were asked to avoid vigorous physical exercise and to keep their arm relaxed. Daytime and night-time periods were defined on the basis of individual sleeping time. At least 70% of the measurements had to be valid, and monitoring had to cover at least 20 h, with an interval of no longer than 3 h between two successive readings [23]. Based on these criteria, about 13% of participants (21 out of 161) underwent unsuccessful monitoring and were thus excluded from the analyses. As measurement of BP variability, SD over 24 h was weighted for the duration of the daytime and night-time intervals [24]. Along with peripheral BP monitoring, pulse waves from the brachial artery were obtained simultaneously with the same conventional upper arm BP cuff. The data from the Mobil-O-Graph device were exported and analysed using the Hypertension Management Software Client-Server version 4.6 (I.E.M.). Central BP and arterial pulse waves were calculated using a generalised transfer function process (ARCSolver; Austrian Institute of Technology, Vienna, Austria), which combined several variables into a mathematical model, coupled with information on age and systolic BP [17]. The augmentation index (AIx) was standardised to a heart rate of 75 bpm.
In addition, PWA and pulse wave velocity (PWV) were recorded by non-invasive applanation tonometry (SphygmoCor; AtCor Medical, Sidney, Australia) under standardised laboratory conditions by the same investigator after participants had rested for 15 min in the supine position in a quiet examination room with a stable temperature. About two-thirds of participants had their tonometry and ambulatory monitoring on the same day, while one-third had a median lag of 14.6 days between these two measurements. The waveforms were recorded from the radial artery of the right arm. The AIx was calculated as the augmentation pressure divided by the pulse pressure, expressed as a percentage and corrected for a heart rate of 75 bpm. Aortic PWV was measured by sequential recording of ECG-gated carotid and femoral artery waveforms with a high-fidelity micromanometer (SPC-301; Millar Instruments, Houston, TX, USA) for 30 s. The SphygmoCor software Cardiovascular Management System, Version 9 (AtCor Medical, Sydney, NSW, Australia) calculates the aortic pulse wave by means of a validated and population-based generalised transfer function [25].
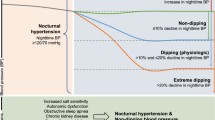
Definitions of hypertension were based on the European Society of Hypertension guidelines [23]. For the office BP, the threshold was ≥140/≥90 mmHg, for 24 h ABPM ≥130/≥80 mmHg, for daytime BP ≥135/≥85 mmHg and for night-time BP ≥120/≥70 mmHg. Masked hypertension was defined as normal office BP but elevated 24 h ABPM, and white-coat hypertension as elevated office BP but normal 24 h ABPM [23]. Nocturnal hypertension was defined as increased absolute values of night-time BP (≥120/≥70 mmHg). Participants with a nocturnal decrease in systolic BP and/or in diastolic BP of less than 10% of the corresponding daytime values were defined as non-dippers [23]. Isolated nocturnal hypertension was defined as normal office BP (<140/90 mmHg), 24 h BP (<130/80 mmHg) and daytime BP (<135/85 mmHg), but elevated night-time BP (≥120/70 mmHg) [23].
Statistical analysis
The data are expressed as mean ± SD for normally distributed variables, as medians with interquartile range for non-normally distributed values and as percentages for categorical variables. Differences between groups were tested using ANOVA for normally distributed variables, and the Kruskal–Wallis test for non-parametric data. Frequencies were tested with a Pearson’s χ2 test or two-tailed Fisher’s exact test. Linear regression analysis was performed to test the association between BP patterns and ambulatory arterial stiffness (i.e. 24 h, daytime and night-time PWV). The multivariable models were adjusted for sex, age, BMI, antihypertensive treatment and eGFR. The number of independent variables was intended to be kept moderate to avoid overfitting. The PWV (dependent variable) corresponding to the independent variables fulfilled the assumptions for a linear regression model: normality, homoscedasticity, independence and linearity. In addition, collinearity of independent variables was tested. Statistical analyses were performed using SAS version 9.4 (SAS Institute, Cary, NC, USA). A p value of <0.05 was considered statistically significant.
Results
BP patterns
In total, 140 individuals with type 1 diabetes were studied, of whom 50% were men. Mean age was 43.7 ± 10.4 years, and mean duration of diabetes was 26.3 ± 9.7 years. The prevalence of normotension was 38% and of sustained hypertension 33% (see electronic supplementary material [ESM] Table 1). Moreover, 23% of participants met the criteria for masked hypertension, and only 6% had white-coat hypertension. In those with masked hypertension, about 9% had only elevated systolic BP and 44% had only elevated diastolic BP, while 47% had elevations in both systolic and diastolic BP. For those with sustained hypertension, more than half of the participants had elevated systolic and diastolic 24 h BP combined with elevations in office systolic BP alone. Nearly 14% of the whole cohort had untreated masked hypertension, while about 9% had uncontrolled masked hypertension, even though they were taking antihypertensive drugs.
Masked hypertension
Table 1 shows the demographic and clinical characteristics of the individuals with normotension, masked hypertension and sustained hypertension. Participants with masked hypertension were more often men (p = 0.002), were older (p = 0.03), had a higher WHR (p = 0.001) and triacylglycerol levels (p = 0.01), and had a higher occurrence of nocturnal hypertension (p < 0.001) than those with normotension. Individuals with sustained hypertension were older (p = 0.02), had a lower BMI (p = 0.008) and eGFR (p = 0.02), were more likely to have retinopathy (p = 0.05) and showed more nocturnal hypertension (p = 0.005) than those with masked hypertension. Notably, no differences were observed regarding glycaemic control, smoking history, antihypertensive medication, dipping pattern, nephropathy status and prevalence of cardiovascular events between participants with sustained hypertension and masked hypertension.
Individuals with masked hypertension had higher office (p = 0.02), 24 h (p < 0.001), daytime (p < 0.001) and night-time (p < 0.001) systolic BP than those who were normotensive. They also had higher office (p = 0.02) and ambulatory (p < 0.001) diastolic BP (Tables 1 and 2). Individuals with sustained hypertension had higher office (p < 0.05) and ambulatory systolic BP (p < 0.05) than those with masked hypertension. Notably, after adjustment for age, in those with masked hypertension, systolic office BP did not differ from those with normotension (p = 0.09), while 24 h (p = 0.1) daytime (p = 0.1) and night-time (p = 0.09) systolic BP did not differ from those with sustained hypertension (ESM Tables 2 and 3). However, both office (p = 0.006) and ambulatory (p < 0.001) diastolic BP were higher in individuals with masked hypertension than in those with normotension. Similarly, diastolic office (p < 0.001) and diastolic ambulatory (p ≤ 0.04) BP were higher in those with sustained hypertension compared with masked hypertension (ESM Tables 2 and 3).
Figure 1 presents box plots of the office BP and 24 h ABPM distributions with and without antihypertensive treatment according to the BP patterns. With masked hypertension, no differences were observed in ambulatory or office BP between antihypertensive treated and untreated participants (Fig. 1), but 24 h systolic BP variability was higher (p = 0.03) among those who had been treated (ESM Table 4). Moreover, the treated individuals had a longer duration of diabetes (p = 0.01) and worse glycaemic control (p = 0.03), were more often taking lipid-lowering drugs (p < 0.001), had a higher WHR (p = 0.006) and recorded more laser-treated retinopathy (p < 0.001) and diabetic nephropathy (p = 0.002) than untreated individuals. In comparison with untreated normotensive participants, along with elevated ambulatory BP profile, masked untreated participants had only higher WHR (p = 0.007) and triacylglycerol concentrations (p = 0.05).
Office BP and 24 h ambulatory systolic (a–c) and diastolic (d–f) BP in individuals with normotension (a, d), masked hypertension (b, e) and sustained hypertension (c, f) with and without antihypertensive treatment. OBP+, office BP, treated with antihypertensives; OBP−, office BP, not treated with antihypertensives; ABP+, 24 h ambulatory BP, treated with antihypertensives; ABP−, 24 h ambulatory BP, not treated with antihypertensives. Data are presented as box plots with mean value (+), median value (central horizontal line), interquartile range (box limits) and minimum and maximum values (the extent of the whiskers). Normotension treated, n = 19; normotension not treated, n = 34; masked hypertension treated, n = 13; masked hypertension not treated, n = 19; sustained hypertension treated, n = 27; sustained hypertension not treated, n = 19. **p < 0.01, ***p < 0.001
Nocturnal hypertension
A total of 72 (51%) individuals had an increased absolute level of night-time BP, half of whom were not on antihypertensive treatment (ESM Table 5). About one-third of those with nocturnal hypertension had either normal office BP (26% were not being treated with antihypertensive agents) or normal daytime BP (21% of them not being treated with antihypertensives). Notably, the proportion of nocturnal hypertension was 59% in those with masked hypertension and as much as 87% in those with sustained hypertension (Table 1). Of the whole cohort, 6% (9 out of 140) of participants met the criteria for isolated nocturnal hypertension, and five individuals were not taking antihypertensive medication. However, their night-time BP values were close to the diagnostic thresholds. Participants with nocturnal hypertension were more often men (p = 0.02), were older (p = 0.002) and had higher a WHR (p = 0.001) than those with normal night-time BP (ESM Table 5). In addition, they had higher PWV (p < 0.001), central BP (p < 0.001) and AIx (p < 0.02) measurements, both at rest (SphygmoCor) and during ambulatory conditions (Mobil-O-Graph).
White-coat hypertension
Only nine participants met the criteria for white-coat hypertension, three of whom were taking antihypertensive medication. About 56% of them were men; their median age was 46.5 (44.3–56.7) years and median duration of diabetes 24.4 (21.5–38.8) years. Median systolic office BP was 148 (142–149) mmHg and diastolic BP 80 (77–85) mmHg, whereas 24 h systolic BP was 122 (120–123) mmHg and diastolic BP 78 (75–78) mmHg.
Markers indicating arterial stiffness
In the ambulatory setting, PWV as well as central systolic and diastolic BP were higher in the participants with masked hypertension (p ≤ 0.001), compared with normotension, but there was no difference with respect to AIx (Table 2, ESM Fig. 1). Furthermore, during resting conditions (SphygmoCor), there were no differences in these markers between the two groups. Individuals with sustained hypertension had a higher PWV (p ≤ 0.007), but not AIx, during ambulatory conditions, and similarly only PWV (p = 0.05) was higher during resting conditions, compared with those with masked hypertension (Table 2, ESM Fig. 1). Although the treated masked hypertension group had higher 24 h PWV (p = 0.003) and AIx (p = 0.006) values than untreated participants, no significant differences were observed in office or 24 h BP (ESM Table 4). However, in comparison with untreated normotensive participants, 24 h systolic (p < 0.001), 24 h diastolic (p < 0.001) BP and 24 h PWV (p = 0.006) were significantly higher in those with untreated masked hypertension.
Table 3 shows the associations between BP patterns and PWV in both the ambulatory (Mobil-O-Graph) and resting (SphygmoCor) conditions. In fully adjusted linear regression models, masked hypertension was associated with higher 24 h PWV (β 0.50 [95% CI 0.34, 0.66]), but not with PWV in resting conditions (β 0.28 [95% CI −0.53, 1.10]), when normotension was the reference. Similar figures were seen in those with sustained hypertension. Interestingly, although only nine participants had white-coat hypertension, median 24 h PWV was also higher than in those who were normotensive (6.7 [6.3–7.7] vs 5.8 [5.5–6.1], p < 0.001), but did not differ from those with masked hypertension (6.4 [6.0–7.4], p = 0.4).
Discussion
The main finding of this study was the high prevalence of masked hypertension in individuals with type 1 diabetes, highlighting the need for ABPM in this group. Notably, of those with masked hypertension, approximately 60% were not on antihypertensive treatment, while 40% were taking treatment, but they may have been treated with insufficient antihypertensive therapy. We also found ambulatory large artery stiffness to be greater in individuals with masked hypertension, compared with truly normotensive individuals. Given the fact that masked hypertension increases the risk of cardiovascular events [8, 9], our results suggest a potential benefit of the parallel use of office BP and ABPM to identify individuals who are at risk, and thereby those who would not have been detected by office BP alone.
The prevalence of masked hypertension varies considerably depending on the study population, definition and BP measurement technique, and whether or not antihypertensive medication is being used [26]. The population-based International Database on Ambulatory blood pressure monitoring in relation to Cardiovascular Outcomes (IDACO) study showed that masked hypertension is more common in individuals with diabetes and those taking antihypertensive medication [10]. About 6% of the middle-aged or the elderly participants had diabetes, but there was no distinction made between diabetes types, suggesting that the majority might have had type 2 diabetes. Among those who had normal office BP, the prevalence of masked hypertension was 29% in those not treated and 42% in those treated who had diabetes, while it was 19% in untreated and 30% in treated non-diabetic individuals. The definition of masked hypertension was based on daytime ABPM (threshold ≥135/85 mmHg). However, nocturnal hypertension is a common phenomenon in diabetes and is superior to daytime BP in predicting cardiovascular risk [23]. In our cohort, about half of the participants had nocturnal hypertension, although one-third of them had either normal office BP or normal daytime BP. Therefore, as recommended by the European Society of Hypertension guidelines, our definition of masked hypertension was based on 24 h ABPM rather than daytime ABPM. By using daytime ABPM alone, we would have missed nearly one-fifth of those affected. Consequently, in our cohort, the prevalence of masked hypertension was 23% in those who were untreated and 34% in those treated among individuals with normal office BP based on daytime ABPM. Compared with the IDACO study population, our lower rates could be explained by the type of diabetes and small number of participants, who were younger and had fewer cardiovascular or other diabetic complications.
Only a few small studies have assessed the prevalence of masked and nocturnal hypertension in individuals with type 1 diabetes [27, 28]. Rodrigues et al [27] reported that the occurrence of masked hypertension in 188 adults with type 1 diabetes who were not taking antihypertensive medication was approximately 7% in the entire cohort and about 14% among those with normal office BP. Moreover, nearly 23% of those with normal office BP had nocturnal hypertension. In a Spanish study of normotensive individuals with type 1 diabetes (n = 85), the prevalence of masked hypertension was 24% [28]. However, our results are not comparable with these two studies, due to differences in cut-off values defining the patterns of hypertension. For both other studies, the threshold for normal office BP was <130/80 mmHg, while for daytime BP it was <135/85 mmHg in the study by Rodrigues et al [27] and <130/80 mmHg in the study by Mateo-Gavira et al [28]. If the office BP threshold is set to 130/80 mmHg, ABPM thresholds should be lowered by 5–10 mmHg [29, 30].
The cut-off values for BP have been debated for years and revised several times. Consequently, there is no consensus regarding the definition of normal ABPM values in individuals with type 1 diabetes. Some have proposed lower cut-offs for ABPM in high-risk individuals with diabetes [9]. The American College of Cardiology and the American Heart Association recently published new guidelines for hypertension [31]. They assume that the majority of individuals with diabetes would fit into the high-risk category (10 year cardiovascular risk >10%), and therefore the new guidelines recommend a more stringent office BP goal (<130/80 mmHg). They also published the corresponding cut-off values for the ABPM measurements: <125/75 mmHg for 24 h ABPM; <130/80 mmHg for daytime ABPM; and <110/65 mmHg for night-time ABPM. These new recommendations may have an impact on diabetes guidelines in the near future. By implementing these new thresholds, the prevalence of different BP patterns would change in our cohort in such a way that the prevalence of normotension would decrease from 38% to 16%, and masked hypertension from 23% to 17%, while the prevalence of sustained hypertension would increase from 33% to 61%.
Someone might argue that only untreated individuals should be considered as having masked hypertension, because treated individuals are already diagnosed, cannot therefore be characterised as masked and should be evaluated separately [23]. In fact, there is evidence that masked hypertension is more common in treated individuals, indicating suboptimal treatment and similarly increased cardiovascular risk as for individuals with sustained hypertension [10]. It has consequently been suggested that the majority of individuals with uncontrolled masked hypertension may have sustained hypertension. The treatment may have focused on normalising office BP, but these individuals continue to have elevated ambulatory BP values, and therefore mimicked masked hypertension [10]. In fact, there is evidence that more intensive treatment of office BP (systolic BP target <120 mmHg) may be more effective in lowering ambulatory BP as well, compared with standard treatment of office BP (systolic BP target <140 mmHg) [32]. In our cohort, no differences were observed in office or ambulatory BP between untreated and treated participants with masked hypertension. Notably, those who were treated had worse glycaemic control, more microvascular complications and higher values of the markers indicating arterial stiffness. Whether masked hypertension predicts diabetic vascular complications in individuals with type 1 diabetes has to be elucidated in longitudinal studies.
Arterial stiffness in individuals type 1 diabetes has been widely studied using non-invasive tonometry under resting conditions [12, 33]. To our knowledge, this study is one of the first to assess determinants of arterial stiffness under ambulatory conditions over 24 h in individuals with type 1 diabetes. We used the oscillometric Mobil-O-Graph device, which has been validated against the non-invasive SphygmoCor device in resting conditions [21, 34]. The validation studies reported comparable estimates regarding central systolic BP and AIx, but lower estimates of PWV. Although the correlation between the PWV values obtained by these two devices was high in our study (r = 0.68), we also found lower estimates of PWV when using the Mobil-O-Graph compared with the SphygmoCor. One reason may be that these devices use different techniques and algorithms to estimate arterial stiffness, and measurements thus appear to be device-dependent and not entirely comparable [35]. Nevertheless, the cuff-based, easy-to-use Mobil-O-Graph device is a promising tool for early screening and evaluation of arterial stiffness during normal daily life [17]. However, more long-term follow-up studies are needed to evaluate the prognostic and clinical value of the measures obtained by the device, as well as thresholds for the measurements.
All participants were part of the carefully characterised FinnDiane study population. The main limitation relates to the cross-sectional design and small sample size. However, additional prospective data from 48 participants from the FinnDiane cohort who performed ABPM three times at 5-yearly intervals demonstrated that the prevalence of masked and sustained hypertension increased by time and duration of diabetes; while only three out of 48 participants met the criteria for masked hypertension at the first visit, as many as 16 had masked hypertension at the third visit (p < 0.001). Similarly, five had sustained hypertension at the first and ten at the third session of AMBP, but the increase did not reach statistical significance (p = 0.2). These preliminary longitudinal data support the data from the cross-sectional analysis. Another limitation being the device-specific technique and the algorithm to calculate the markers of arterial stiffness, our measurements may not, therefore, necessarily be comparable with the results obtained using other devices. However, it has to be acknowledged that the methodology has been previously validated [20,21,22]. Finally, we did not have information to assess participants’ adherence to antihypertensive treatment.
In conclusion, this study showed a large number of disturbed BP patterns in individuals with type 1 diabetes, patterns that would not have been detected by office BP alone. The main finding was, however, that one-quarter of participants had masked hypertension, and the same group had also signs of arterial stiffness, a condition known to precede manifest hypertension and cardiovascular disease. Therefore, detailed evaluation of BP patterns by ABPM could be clinically meaningful in order to improve the diagnosis and management of hypertension in this group. However, further longitudinal and interventional studies are needed to evaluate the prognostic value of masked hypertension and the effect of antihypertensive treatment in individuals with type 1 diabetes.
Data availability
No data are available. The ethical statement and informed consent do not allow for free data availability.
Abbreviations
- ABPM:
-
Ambulatory BP monitoring
- AIx:
-
Augmentation index
- CKD-EPI:
-
Chronic Kidney Disease Epidemiology Collaboration
- FinnDiane:
-
Finnish Diabetic Nephropathy Study
- IDACO:
-
International Database on Ambulatory blood pressure monitoring in relation to Cardiovascular Outcomes
- PWA:
-
Pulse wave analysis
- PWV:
-
Pulse wave velocity
References
Jensen T, Borch-Johnsen K, Kofoed-Enevoldsen A, Deckert T (1987) Coronary heart disease in young type 1 (insulin-dependent) diabetic patients with and without diabetic nephropathy: incidence and risk factors. Diabetologia 30:144–148
Forrest KY, Becker DJ, Kuller LH, Wolfson SK, Orchard TJ (2000) Are predictors of coronary heart disease and lower-extremity arterial disease in type 1 diabetes the same? A prospective study. Atherosclerosis 148:159–169
Lithovius R, Harjutsalo V, Forsblom C, Saraheimo M, Groop PH, on behalf of the FinnDiane Study Group (2014) Antihypertensive treatment and resistant hypertension in patients with type 1 diabetes by stages of diabetic nephropathy. Diabetes Care 37:709–717
Mancia G, Verdecchia P (2015) Clinical value of ambulatory blood pressure: evidence and limits. Circ Res 116:1034–1045
Solak Y, Kario K, Covic A et al (2016) Clinical value of ambulatory blood pressure: is it time to recommend for all patients with hypertension? Clin Exp Nephrol 20:14–22
Hodgkinson J, Mant J, Martin U et al (2011) Relative effectiveness of clinic and home blood pressure monitoring compared with ambulatory blood pressure monitoring in diagnosis of hypertension: systematic review. BMJ 342:d3621
Lazaridis AA, Sarafidis PA, Ruilope LM (2015) Ambulatory blood pressure monitoring in the diagnosis, prognosis, and management of resistant hypertension: still a matter of our resistance? Curr Hypertens Rep 17:78
Pickering TG, Davidson K, Gerin W, Schwartz JE (2002) Masked hypertension. Hypertension 40:795–796
O’Brien E, Parati G, Stergiou G et al (2013) European Society of Hypertension position paper on ambulatory blood pressure monitoring. J Hypertens 31:1731–1768
Franklin SS, Thijs L, Li Y et al (2013) Masked hypertension in diabetes mellitus: treatment implications for clinical practice. Hypertension 61:964–971
George B, Bantwal G, Ayyar V, Mathew V (2015) Occurrence of increased arterial stiffness in a cohort of adult patients with type 1 diabetes mellitus when compared to normoglycemic controls. J Diabetes Sci Technol 9:138–144
Theilade S, Lajer M, Persson F, Joergensen C, Rossing P (2013) Arterial stiffness is associated with cardiovascular, renal, retinal, and autonomic disease in type 1 diabetes. Diabetes Care 36:715–721
Nilsson PM, Lurbe E, Laurent S (2008) The early life origins of vascular ageing and cardiovascular risk: the EVA syndrome. J Hypertens 26:1049–1057
Rönnback M, Fagerudd J, Forsblom C, Pettersson-Fernholm K, Reunanen A, Groop PH, Finnish Diabetic Nephropathy (FinnDiane) Study Group (2004) Altered age-related blood pressure pattern in type 1 diabetes. Circulation 110:1076–1082
Gordin D, Waden J, Forsblom C et al (2011) Pulse pressure predicts incident cardiovascular disease but not diabetic nephropathy in patients with type 1 diabetes (the FinnDiane study). Diabetes Care 34:886–891
Takeno K, Mita T, Nakayama S et al (2012) Masked hypertension, endothelial dysfunction, and arterial stiffness in type 2 diabetes mellitus: a pilot study. Am J Hypertens 25:165–170
Omboni S, Posokhov IN, Kotovskaya YV, Protogerou AD, Blacher J (2016) Twenty-four-hour ambulatory pulse wave analysis in hypertension management: current evidence and perspectives. Curr Hypertens Rep 18:72
Thorn LM, Forsblom C, Fagerudd J et al (2005) Metabolic syndrome in type 1 diabetes: association with diabetic nephropathy and glycemic control (the FinnDiane study). Diabetes Care 28:2019–2024
Levey AS, Stevens LA, Schmid CH et al (2009) CKD-EPI (Chronic Kidney Disease Epidemiology Collaboration). A new equation to estimate glomerular filtration rate. Ann Intern Med 150:604–612
Hametner B, Wassertheurer S, Kropf J, Mayer C, Eber B, Weber T (2013) Oscillometric estimation of aortic pulse wave velocity: comparison with intra-aortic catheter measurements. Blood Press Monit 18:173–176
Weiss W, Gohlisch C, Harsch-Gladisch C, Tolle M, Zidek W, van der Giet M (2012) Oscillometric estimation of central blood pressure: validation of the Mobil-O-Graph in comparison with the SphygmoCor device. Blood Press Monit 17:128–131
Feistritzer HJ, Reinstadler SJ, Klug G et al (2015) Comparison of an oscillometric method with cardiac magnetic resonance for the analysis of aortic pulse wave velocity. PLoS One 10:e0116862
Parati G, Stergiou G, O’Brien E et al (2014) European Society of Hypertension practice guidelines for ambulatory blood pressure monitoring. J Hypertens 32:1359–1366
Hansen TW, Thijs L, Li Y et al (2010) Prognostic value of reading-to-reading blood pressure variability over 24 hours in 8938 subjects from 11 populations. Hypertension 55:1049–1057
Wilkinson IB, Fuchs SA, Jansen IM et al (1998) Reproducibility of pulse wave velocity and augmentation index measured by pulse wave analysis. J Hypertens 16:2079–2084
Franklin SS, O’Brien E, Thijs L, Asayama K, Staessen JA (2015) Masked hypertension: a phenomenon of measurement. Hypertension 65:16–20
Rodrigues TC, Canani LH, Viatroski RS, Hoffmann LH, Esteves JF, Gross JL (2010) Masked hypertension, nocturnal blood pressure and retinopathy in normotensive patients with type 1 diabetes. Diabetes Res Clin Pract 87:240–245
Mateo-Gavira I, Vilchez-Lopez FJ, Garcia-Palacios MV, Carral-San Laureano F, Jimenez-Carmona S, Aguilar-Diosdado M (2016) Nocturnal blood pressure is associated with the progression of microvascular complications and hypertension in patients with type 1 diabetes mellitus. J Diabetes Complicat 30:1326–1332
Head GA, Mihailidou AS, Duggan KA et al (2010) Definition of ambulatory blood pressure targets for diagnosis and treatment of hypertension in relation to clinic blood pressure: prospective cohort study. BMJ 340:c1104
Parati G, Bilo G (2009) Should 24-h ambulatory blood pressure monitoring be done in every patient with diabetes? Diabetes Care 32:S298–S304
Whelton PK, Carey RM, Aronow WS et al (2018) 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/ APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension 71:e13–e115
Drawz PE, Pajewski NM, Bates JT et al (2017) Effect of intensive versus standard clinic-based hypertension management on ambulatory blood pressure: results from the SPRINT (Systolic Blood Pressure Intervention Trial) Ambulatory Blood Pressure Study. Hypertension 69:42–50
Gordin D, Waden J, Forsblom C et al (2012) Arterial stiffness and vascular complications in patients with type 1 diabetes: the Finnish Diabetic Nephropathy (FinnDiane) study. Ann Med 44:196–204
Luzardo L, Lujambio I, Sottolano M et al (2012) 24-H ambulatory recording of aortic pulse wave velocity and central systolic augmentation: a feasibility study. Hypertens Res 35:980–987
Omboni S, Posokhov IN, Parati G et al (2016) Vascular health assessment of the hypertensive patients (VASOTENS) registry: study protocol of an international, web-based telemonitoring registry for ambulatory blood pressure and arterial stiffness. JMIR Res Protoc 5:e137
Acknowledgements
The skilled technical assistance of A. Sandelin, M. Rahkonen, J. Tuomikangas and M. Parkkonen (Folkhälsan Research Center/University of Helsinki, Helsinki, Finland) is gratefully acknowledged. Parts of this study were presented in abstract form at the 53rd Annual Meeting of the European Association for the Study of Diabetes, Lisbon, Portugal, 11–15 September 2017.
Funding
The study was supported by grants from the Folkhälsan Research Foundation, the Wilhelm and Else Stockmann Foundation, the Academy of Finland, the Liv och Hälsa Society, the Waldemar von Frenckell Foundation, the Finnish Medical Society and the Novo Nordisk Foundation.
Author information
Authors and Affiliations
Consortia
Contributions
RL designed and carried out the data analyses, interpreted the results and drafted the manuscript. DG designed and interpreted the results and revised the manuscript critically for important intellectual content. MS interpreted the results and revised the manuscript critically for important intellectual content. VH designed the data analysis, contributed to the acquisition of data and revised the manuscript. CF and P-HG contributed to the acquisition of data and revised the manuscript critically for important intellectual content. P-HG is the guarantor of this work and, as such, had full access to all the data in the study and take full responsibility for the integrity of the data and the accuracy of the data analysis. All authors gave their final approval of this version of the manuscript.
Corresponding author
Ethics declarations
P-HG has received lecture honoraria from Astra Zeneca, Boehringer Ingelheim, Eli Lilly, EloWater, Genzyme, Medscape, MSD, Novartis, Novo Nordisk and Sanofi. P-HG is an advisory board member for AbbVie, Astra Zeneca, Boehringer Ingelheim, Eli Lilly, Medscape, MSD, Novartis, Novo Nordisk and Sanofi. P-HG has received investigator-initiated grants from Eli Lilly and Roche. MS has received lecture fees from Astra Zeneca, BD, Eli Lilly, Infucare, Medtronic, Novo Nordisk, Roche and Sanofi-Aventis, and is an advisory board member of Medtronic in Scandinavia, Abbott Diabetes Care EMEA and the Insulin Advisory Board of Novo Nordisk Finland. The funding sources were not involved in the design or conduct of the study. All other authors declare that there is no duality of interest associated with this manuscript.
Electronic supplementary material
ESM
(PDF 331 kb)
Rights and permissions
About this article
Cite this article
Lithovius, R., Gordin, D., Forsblom, C. et al. Ambulatory blood pressure and arterial stiffness in individuals with type 1 diabetes. Diabetologia 61, 1935–1945 (2018). https://doi.org/10.1007/s00125-018-4648-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-018-4648-5