Abstract
Aims/hypothesis
The aim of this study was to examine whether cognitive function in early and later life, and decline in cognitive function from age 70 to 79 years, are associated with high blood glucose, as measured by HbA1c, at baseline (age 70), and changes in blood glucose from age 70 to 79.
Methods
Participants (n = 1091) in the Lothian Birth Cohort of 1936 were examined. Fourteen tests were used to assess cognitive functions, grouped into four domains: visuospatial ability, processing speed, memory and crystallised ability. Test results, and measurements of HbA1c and other health variables, were collected at each of four waves of assessment: at the mean age of 70, 73, 76 and 79 years. Data on cognitive function at age 11 was also available for this cohort. Latent growth curve modelling was performed and statistical controls for known risk factors were introduced.
Results
Higher age 11 cognitive function predicted lower HbA1c level at age 70 (p < 0.001). Higher cognitive function at age 70 was related to a comparatively smaller increase in HbA1c levels from age 70 to 79 (p < 0.001). HbA1c from age 70 to 79 did not have any consistent association with change in cognitive function from age 70 to 79. These associations survived adjustments for age, sex, education, APOE*ε4, smoking history, cardiovascular disease history, hypertension history, BMI and corrections for multiple testing.
Conclusions/interpretation
Our results show that, among older individuals, high blood glucose is consistently predicted by lower cognitive function. Clinical care that examines and tracks cognitive function, while also taking the positive effects of maintaining cognitive function and emulating healthy behaviours associated with higher cognitive function into account, may be one approach for protecting at-risk individuals from elevated blood glucose and subsequent type 2 diabetes mellitus.
Similar content being viewed by others
Avoid common mistakes on your manuscript.

Introduction
As the prevalence of type 2 diabetes mellitus has grown worldwide, so has the need to understand related health implications such as the link between diabetes and cognitive function. Type 2 diabetes is associated with an increased risk of cognitive decline and dysfunction, including dementia [1]. Diabetes-associated cognitive impairment is expected to become more prevalent as life expectancy for individuals with diabetes increases worldwide, highlighting a need to understand the reciprocal dynamic progression of type 2 diabetes and cognitive decline. The present study investigates the relationships between cognitive change and HbA1c measurements, one of the most important risk metrics in type 2 diabetes.
Impaired glucose control, confirmed by HbA1c measurement, is present in and predicts the development of type 2 diabetes, even though the syndrome may be asymptomatic and go undetected for years [2]. High HbA1c is also associated with cognitive decline in older populations, in both healthy individuals [3] and those diagnosed with type 2 diabetes [4, 5]. Additionally, HbA1c levels are associated with micro- and macrovascular complications [2, 6], reduction in brain volume [7, 8], and dementia [9]. The HbA1c–cognitive function relationship could be causative: the toxic generation of free radicals which accompanies increased HbA1c may cross over into the brain, affecting cognitive functions [10].
Previous work on cognitive functioning and diabetes has focused on controlling for known risk factors such as vascular disease and the APOE*ε4 allele, as well as identifying independent risk factors such as glucose peaks [11] and insulin resistance [12] that could be linked to cognitive decline. However, whereas type 2 diabetes and high blood glucose are associated with poorer cognitive function later in life, evidence for reverse causation also exists, suggesting that lower prior cognitive function might contribute to type 2 diabetes aetiology [13]. Many samples are unable to address these types of questions because they lack a longitudinal design that tracks relevant variables, cognitive and health-related, in the same individuals across discrete waves of assessment. HbA1c is a useful marker for studying the development of diabetes in this way, as it has good specificity and sensitivity to detect type 2 diabetes and also measures the severity of the disease [6, 14,15,16].
This study’s aim was to characterise, across the eighth decade of life, parallel changes in cognitive functions and high blood glucose (measured by HbA1c), and to investigate associations between baseline levels and change in these measures over time. Our study used four waves of data from the Lothian Birth Cohort of 1936 (LBC1936), a narrow age cohort of over 1000 community-dwelling people tested in four waves from age 70 to 79 years. LBC1936 also provides cognitive function data from age 11, as well as other control variables. This sample allowed us to assess two non-mutually exclusive hypotheses: higher HbA1c at age 70 is associated with relatively greater cognitive decline from age 70 to 79 [17,18,19]; and the reverse causative hypothesis, i.e. that lower initial cognitive function and relatively greater cognitive decline are associated with subsequently higher HbA1c levels [13, 20].
Methods
Study population
LBC1936 is a community-dwelling sample of 1091 initially healthy individuals. All were born in 1936 and were followed up in four waves of one-to-one cognitive and health testing between 2004 and 2017, at mean ages 70, 73, 76 and 79 years. Details on the background, recruitment and data collection procedures are available [21, 22]. Participants provided written informed consent. Ethics permissions were obtained from the Multicentre Research Ethics Committee for Scotland (wave 1, MREC/01/0/56), the Lothian Research Ethics Committee (wave 1, LREC/2003/2/29) and the Scotland A Research Ethics Committee (waves 2–4, 07/MRE00/58).
Cognitive function
When they were approximately 11 years old, 1028 members of the LBC1936 sat Moray House Test No. 12, a broad cognitive ability test that included word classification, proverbs, spatial items and arithmetic. The test correlated about 0.8 with the Terman–Merrill revision of the Stanford–Binet test, providing concurrent validity [23].
In older age, cognitive function is known to decline across multiple domains [24]. Age effects also act on overall cognitive function, a superordinate factor of the lower function domains [24]. We included tests to measure three important cognitive function domains that decline with age: visuospatial ability, processing speed and memory. We also tested crystallised ability, which remains relatively stable in later life [25]. All four domains also contribute to overall cognitive ability [26]. These relationships among cognitive tests and domains are described in the Statistical Analyses section below.
Cognitive functions in waves 1–4 were assessed using 14 individually administered cognitive tests at the same clinical research facility and using the same equipment and procedure for all four waves. The tests are fully described and referenced in an open-access protocol article [21]. The visuospatial domain consisted of matrix reasoning and block design from the Wechsler Adult Intelligence Scale (WAIS) [27], and spatial span forward and backward from the Wechsler Memory Scale (WMS) [28]. Processing speed was measured through symbol search and digit symbol substitution from the WAIS, plus four-choice reaction time [29] and inspection time [30, 31]. Memory was assessed using verbal paired associates and logical memory from the WMS [28], and the letter–number sequencing and digit span backward subtests of the WAIS [27]. Crystallised ability was measured through the National Adult Reading Test [32], Wechsler Test of Adult Reading [33] and a phonemic verbal fluency test [34].
Clinical diabetes measures
For each individual during each wave, HbA1c concentrations were measured using a Menarini HA-8160 analyser (Wokingham, UK). Diabetes diagnosis status was independently recorded. Twelve individuals with type 1 diabetes were excluded from further analyses.
Covariates
Three variable sets were evaluated as potential confounders. The first set defined our baseline control covariates: sex, age (z scored), age 11 cognitive function (z scored), and years of education (z scored). The second set included the available cardiovascular risk factors, obtained from interview and genetic testing: high BP history (no/yes), cardiovascular disease (CVD) history (no/yes), smoking history (current/former/never), and the presence of an APOE*ε4 allele. The third set contained only BMI (z scored), recorded at every testing wave and introduced to our analyses separately from the other cardiovascular variables because BMI is strongly associated with HbA1c and can have a confounding effect.
Statistical analyses
All four LBC1936 waves were analysed in latent growth curve models (LGCMs), a structural equation modelling technique that allows the user simultaneously to define and analyse multiple latent and measured variables [35]. For each variable modelled longitudinally, LGCMs model level (i.e. an intercept) and slope (i.e. a trajectory of change) variables. We modelled cognitive function using a hierarchical ‘factor of curves’ model, previously established with these data [26]. For each cognitive test we modelled a level (essentially the age 70 baseline) and a linear slope (the change between age 70 and 79, taking all four measurement occasions into account); for each cognitive domain (see Cognitive function, above) a latent level and linear slope variable were correspondingly composed of the individual tests’ latent level and latent slope variables. At the top of this cognitive hierarchy, latent levels and slopes for overall cognitive function were formed from the level and slope variables of each cognitive domain. For HbA1c variables, the same approach was taken, but only a pair of level and slope variables were defined for this outcome variable, as no hierarchical structure exists. A structural diagram to illustrate these measured and latent variables is presented in Fig. 1. We also investigated quadratic slope variables for both cognitive function and HbA1c, but models including quadratic components either would not converge successfully, or they fit very poorly and could not be trusted to produce reliable estimates.
Simplified path diagram of the hierarchical factor of curves growth model of cognitive function and HbA1c. Circles represent latent variables and squares represent measured variables. Growth curves, including a latent level and slope factor, were estimated for each cognitive test, and the intercepts and slopes were analysed in a hierarchical model which contained domain and overall factors of both level and slope. Basis coefficients (loadings on the individual test slopes) were fixed at 0, 2.96, 6.72 and 9.79 to precisely represent the amount of time passing between assessments. All loadings on latent level were fixed at 1. Dashed lines indicate the relationships between covariates that were fixed across waves and the overall and domain latent variables. Dotted lines indicate the relationships between covariates that differed between waves and individual measurements at different waves. To preserve interpretability, not all covariate relationships are shown. Solid double-arrowed lines indicate correlations between latent variables. Solid single arrowed lines indicate the variables that load on latent variables. Although only two domains and four tests are shown here, the full model used all 14 tests in the four domains, as described in Methods
Put simply, HbA1c level is analogous to blood glucose at the study’s beginning (age 70 years), and HbA1c slope is analogous to the magnitude at which blood glucose increases over the following decade. Cognitive function level is analogous to cognitive function at age 70 and is known to be highly correlated with cognitive function at age 11 [26], demonstrating the stability of cognitive function across a lifetime. The slope of cognitive function represents the rate at which cognitive functions change (mostly decrease, in fact) over subsequent waves, which is otherwise known as cognitive decline.
Control covariates that applied to all waves of data (sex, age 11 cognitive function, years of education, APOE*ε4 status and smoking history) were regressed on to the intercept and slope variables for latent levels and slopes, including those for the domains of cognitive function, but not on to the levels or slopes of individual cognitive tests. Control covariates that were related to physical condition and could differ between waves (age, history of high BP, history of CVD, and BMI) were regressed on to the individual HbA1c measurements.
Model coefficients were estimated using full information maximum likelihood, i.e. all data were used for all participants, even individuals who did not complete all waves. Standard errors were calculated using the robust Huber–White method, and p values were computed using the Yuan–Bentler scaled test statistic [36]. The false discovery rate correction for multiple testing was applied to the variables in each model that were not control covariates, which included the associations between the latent variables of cognitive function and its subdomains and HbA1c. All analyses were conducted in the R programming language, version 3.3.2 (R Foundation for Statistical Computing, Vienna, Austria), using the latent variable analysis (lavaan) package for modelling [37].
Results
Cohort characteristics
Demographic and clinical characteristics of the study population at all four waves are presented in Table 1. Electronic supplementary material (ESM) Table 1 presents wave 1–3 descriptions of study completers only, i.e. those individuals who remained present in wave 4.
Individuals with type 2 diabetes were more likely than healthy individuals to have a history of CVD or high BP (Table 1). The type 2 diabetes group included more men, as well as more current and former smokers. Individuals with type 2 diabetes had higher BMI and HbA1c levels; in all waves their mean HbA1c was above the diagnostic threshold of 48 mmol/mol (6.5%). Individuals with type 2 diabetes had lower age 11 cognitive function and scored more poorly than healthy individuals on all cognitive tests across all four waves.
To illustrate cognitive decline across domains, we plotted the discrete overall cognitive function and domain scores across all four waves, with individuals categorised as either healthy or showing a clinical or biochemical (HbA1c above diagnostic threshold) type 2 diabetes diagnosis at wave 1 (Fig. 2). Figure 2 represents study completers only, because including data from all study participants would bias the means of later waves in the positive direction, making plots unrepresentative of the sample. As expected, with the exception of crystallised ability, the curves show clear declines across all other cognitive domains in individuals with and without type 2 diabetes; however, cognitive function was worse in individuals with type 2 diabetes. Figure 2 is for illustration purposes only.
Trajectories of overall and domain-specific cognitive abilities in individuals with and without type 2 diabetes in the Lothian Birth Cohort 1936. Diabetes was defined by reported physician diagnosis or HbA1c level >48 mmol/mol (6.5%) at wave 1. (a) Overall cognitive ability, composed of the four specific cognitive domains: visuospatial ability (b), processing speed (c), memory (d) and crystallised ability (e). Red line and 95% confidence region, individuals without diabetes; blue line and 95% confidence region, individuals with diabetes. These plots only include data from individuals with data available from all four waves of the Lothian Birth Cohort 1936 study, since including data from all individuals in these plots would bias the means towards a positive direction at older ages, making them unrepresentative of the whole sample
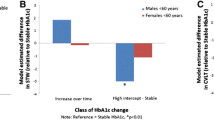
Age 70–79 cognitive performance and HbA1c
Figure 3 shows the relationships between the level and slope estimates of HbA1c and overall cognitive function. Three models are presented, with control variables added cumulatively, as described in Methods. The diagrams present the results for overall cognitive function; domain-specific results can be found in ESM Table 2. The effects of control variables on the level and slope estimates are also presented in Fig. 3, whereas disease-relevant effects of control variables, measured at each wave, are presented separately in ESM Table 2. Model fit statistics of all LGCMs indicated a good fit (root mean square error of approximation [RMSEA] <0.33; standardised root mean residual [SRMR] <0.62; comparative fit index [CFI] >0.939; Tucker–Lewis index [TLI] >0.936; see ESM Table 3 for complete fit statistics).
Path diagram of relationships between level and slope estimates of overall cognitive function (CF) and HbA1c in the Lothian Birth Cohort 1936 from age 70 to 79 years. In (a), the model includes the covariates shown, as well as age. In (b), the model includes the covariates shown, as well as age and history of CVD and high BP, history of smoking and the presence of an APOE*ε4 allele. In (c), the model includes all the covariates shown, age, and history of CVD, history of high BP, smoking and APOE*ε4, as well as BMI (the latter is demonstrated as a time-varying covariate in ESM Table 2). Numbers presented are standardised estimates with SEM in parentheses. Double-headed arrows between latent variables (circles) indicate correlations. Single-headed arrows from covariates (rectangles) indicate regression effects on latent variables. Dashed lines indicate non-significant correlations, whilst solid lines and † indicate significance; The false discovery rate correction for multiple testing was applied to all tested relationships. Additional estimates for domains and controls are presented in ESM Table 2
Age 11 cognitive function made significant contributions to both cognitive function level (β > 0.4, coefficient of partial determination ρ2 > 0.35) and HbA1c level (β > −0.066, ρ2 > 0.007) at age 70; that is, higher childhood cognitive function was associated with higher cognitive function and lower HbA1c concentration at age 70. More education was also associated with better cognitive function in older age, though to a lesser degree (β > 0.12, ρ2 > 0.026). These findings are consistent with those previously reported [13, 20, 38].
The relationship between cognitive function level at age 70 and cognitive function slope was robust and did not change when covariates were added (r = 0.002, ρ2 = 4 × 10−6), but the association was small enough that we can only infer that cognitive function level and slope have no strong relationship. This is likely due to low covariance between cognitive function level and slope; or, in other words, regardless of an individual’s starting cognitive function level, cognitive function will consistently decline over the course of the eighth decade.
Significant associations of the same sign were found between HbA1c slope and both level and slope of cognitive function in models. These results indicate that individuals with higher cognitive function at age 70 maintain lower blood glucose over the following decade, and these associations remain in the presence of all control covariates. The association between cognitive function level and HbA1c slope was as large as r = −0.166 (ρ2 = 0.03), which was found after controlling for the influence of age 11 cognitive function and education. The relationship between cognitive function slope and HbA1c slope, while consistently positive and significant, was small: at most it was r = 0.008 (ρ2 = 6.4 × 10−5) in the first model (Fig. 3a), which includes the fewest controls.
Associations between HbA1c level and cognitive function slope were significant but were not consistent across models and were relatively small. Moreover, the association between cognitive function level and HbA1c level was not always significant, nor was it in the same direction across models. We found no significant associations between HbA1c level and slope in any of these models.
Associations between HbA1c growth curve estimates and cognitive function at the domain level generally followed the associations found with overall cognitive function level and slope (Fig. 3; ESM Table 2), with the exception of crystallised ability, which, even in older individuals, tends not to decline over time. In the first model, with the fewest controls, all cognitive domain variables were significantly associated with HbA1c level and slope, and this held true across subsequent models, except for the slope variables of memory and crystallised ability. Decline in memory and crystallised ability was not associated with either HbA1c level or slope after controls were included.
We conducted sensitivity analyses on our three structural equation models; specifically, we fit the same models, excluding individuals from a wave if they had been given any type of diabetes diagnosis. The resultant models were very similar to the models presented in Fig. 3 (ESM Table 4); effect sizes were generally reduced, and no previously small and/or unstable associations became robust in these models. We also tested whether change in cognitive function that occurred between age 11 and age 70 was associated with HbA1c levels, but while age 11 cognitive function significantly predicted HbA1c, change in cognitive function did not (ESM Results, ESM Table 5).
Post hoc analyses of diagnosis status interacting with cognitive function and HbA1c
Individuals might change their behaviour once they are aware that they have type 2 diabetes. To test whether or not higher functioning individuals may be better at caring for themselves after diagnosis, we ran a repeated-measures ANCOVA on the first two study waves, treating type 2 diabetes diagnosis, wave and overall cognitive function as independent variables and HbA1c as the dependent variable. Type 2 diabetes diagnosis (ω2 = 0.338, p < 0.0001), cognitive function (ω2 = 0.004, p < 0.0001) and wave (ω2 = 0.023, p < 0.0001) all had individual main effects, as did the type 2 diagnosis and wave interaction (ω2 = 0.006, p < 0.0001). However, type 2 diagnosis and cognitive function did not significantly interact (ω2 < 0.001, p = 0.742), suggesting that knowledge of one’s diagnosis is not related to higher functioning individuals taking better care of themselves. No additional interactions in the model were significant either. These results were robust to the inclusion of control covariates (ESM Table 6).
In much the same way that cognitive function might behaviourally impact post-diagnosis HbA1c, individuals with type 2 diabetes who maintain low HbA1c measurements may show cognitive differences from individuals with type 2 diabetes who do not maintain healthier HbA1c. We also tested this is an ANCOVA framework, making cognitive function the outcome variable, and including HbA1c, wave (1 or 2) and type 2 diabetes diagnosis as independent variables. We found main effects of type 2 diabetes diagnosis (ω2 = 0.014, p < 0.0001) and HbA1c (ω2 = 0.006, p = 0.0001), but no effects of wave or any interactions. These effects were robust to the inclusion of covariates (ESM Table 7). Together, these findings suggest that type 2 diabetes diagnosis and HbA1c are both associated with cognitive function, but neither changes in diagnosis nor whether an individual with type 2 diabetes has relatively low or high HbA1c appear to be related to cognitive function.
Discussion
The results show that in an older narrow age cohort, tested on four occasions between 70 and 79 years, lower cognitive function at 70 is associated with increases in HbA1c over the following decade. Cognitive function level is negatively correlated with the slope of HbA1c, and this effect is robust to the inclusion of all covariates, including age 11 cognitive function. Age 11 cognitive function itself is consistently and negatively related to HbA1c level, which is consistent with previous reports of this sample [20, 39]. Together, these results suggest that cognitive function consistently predicts blood glucose later in life.
Other associations between slope and level estimates of cognitive functions and HbA1c were generally small and were inconsistent when different covariates were added. We found no consistent relationships between HbA1c level and cognitive function slope, which represents cognitive decline. If HbA1c had a causative, negative effect on cognitive function, we would expect to find this, but the largest association was 0.018 and in the opposite direction from what we would expect. The associations discussed thus far are visible in Fig. 2, where one can see that the initial level of cognitive function is lower in individuals with type 2 diabetes, though the rate of decline is not obviously different.
We found a significant association between age 11 cognitive function and HbA1c level starting at age 70 and cognitive function level at age 70, but we did not find any relationships between HbA1c level and age 70 cognitive function level or change in cognitive function from ages 11 and 70. This suggests that early life cognition, which is stable over the lifespan, drives the cross-sectional association between cognitive function and HbA1c at age 70. In 1947, there was no HbA1c measurement at age 11, so we cannot decide here whether early cognitive function is causal to worsening blood glucose across the life course to age 70, or whether cognitive functioning and blood glucose track each other through the life course.
It is notable that age 11 cognitive function was not associated with HbA1c slope, but cognitive function level at age 70 was. This was surprising, given that cognitive function level at age 70 was not reliably related to HbA1c level starting at the same age. However, these findings are consistent with a lead-lag effect: better cognitive functioning earlier in life predicts lower blood glucose, but only later in life.
Early cognitive function is a major life course variable that influences blood glucose and type 2 diabetes progression. In this sample, sex had few effects on level and slope outcomes. The strongest was with cognitive function level—men tended to have higher cognitive function level in this sample. Years of education display similar relationships: very small effects on all level and slope estimates other than cognitive function level, with which education showed positive relationships (β > 0.12).
When introduced in model B, disease variables including APOE*ε4 and hypertension and CVD history greatly reduced the effect of cognitive function on HbA1c slope. Smoking history, for example, had a notable effect on HbA1c level, indicating that smokers were more likely to have higher HbA1c at age 70. The impact of these variables suggests that the association between cognitive function and later measurements of HbA1c is related to health behaviours. One interpretation of the results is that individuals with higher cognitive function take better care of themselves: they smoke less, are more active and have a healthier diet [40]. These associations between cognitive function and health later in life have been extensively investigated [41,42,43], including through diabetes epidemiology [13, 20]. However, our post hoc analyses demonstrated that the relationship between cognitive function and HbA1c could not be explained by participants with higher cognitive function altering their behaviour more than those with lower cognitive function when these participants become aware of their type 2 diabetes diagnosis.
The extensive clinical and cognitive data that were available across all four waves, over a decade, are clear strengths of this study, as was the availability of a reliable cognitive function measure at an early age. Moreover, the broad range of validated cognitive tests allowed us to investigate both overall and domain level associations between cognitive function and blood glucose. As the LBC1936 is a narrow age cohort, neither cohort nor age effects could significantly bias our findings.
There were also limitations to this study that ought to be considered. First, our sample featured relatively few individuals diagnosed with type 2 diabetes, which limits the power of the statistical analyses. This issue was somewhat ameliorated by our use of HbA1c as an outcome, which captures fine-grained information about diabetic and prediabetic status; nevertheless, comparatively few individuals had clinically elevated blood glucose. Second, and similarly, dropout (most likely due to mortality and frailty) was significant; almost half of the original sample did not return by the fourth wave. Whereas our models take existing and missing data into account, ultimately these missing data limit our statistical power and would particularly impact our analyses of slopes. For instance, we might not have possessed the statistical power to detect small changes in cognitive function that could have been driven by high HbA1c. Third, we did not have any HbA1c measurements from earlier in life, so we could not control for the influence of type 2 diabetes precursors that might have existed earlier in life. However, the prevalence of type 2 diabetes in children and young adults is low [44] and would be lower still in a cohort born in 1936 [20].
HbA1c not only predicts type 2 diabetes but is also associated with vascular complications [2, 6] and declines in both cognitive function [3, 4, 9] and brain volume [7, 8]. However, some prior findings are counterintuitive. For example, total brain volume was increased in a group receiving targeted glycaemic control therapy, but in spite of this no differences were found in cognitive outcomes [7]. In general, it is difficult to determine the direction of causality in the association between type 2 diabetes and cognitive decline, but the current literature suggests that having type 2 diabetes causes greater cognitive decline [11, 12, 19, 45, 46].
Our results support an alternative hypothesis, i.e. that cognitive function predicts high blood glucose; however, we stress that the two hypotheses are not mutually exclusive. The best explanation for our results and the wider body of research is that early life cognitive function contributes to impairment of glucose tolerance and onset of type 2 diabetes. Once an individual has developed diabetes, complication of the disease could lead to later impairment in cognitive function. Our results also suggest that good cognitive function continues to protect an individual from developing high blood glucose, emphasising its possible importance in ameliorating type 2 diabetes progression throughout the lifespan. Further research into the mechanisms whereby cognitive function impacts and is impacted by elevated blood glucose is warranted in the pursuit of underused strategies for identifying at-risk older individuals and protecting them from cognitive decline and type 2 diabetes.
Data availability
The datasets analysed during the current study are not publicly available due to factors of individual privacy and health security, but are available from the study director of the Lothian Birth Cohorts of 1921 and 1936 on reasonable request.
Abbreviations
- CVD:
-
Cardiovascular disease
- LBC1936:
-
Lothian Birth Cohort of 1936
- LGCM:
-
Latent growth curve model
- WAIS:
-
Wechsler Adult Intelligence Scale
- WMS:
-
Wechsler Memory Scale
References
Biessels GJ, Strachan MW, Visseren FL, Kappelle LJ, Whitmer RA (2014) Dementia and cognitive decline in type 2 diabetes and prediabetic stages: towards targeted interventions. Lancet Diabetes Endocrinol 2:246–255
Bennett C, Guo M, Dharmage S (2007) HbA1c as a screening tool for detection of type 2 diabetes: a systematic review. Diabet Med 24:333–343
Ravona-Springer R, Moshier E, Schmeidler J et al (2012) Changes in glycemic control are associated with changes in cognition in non-diabetic elderly. J Alzheimers Dis 30:299–309
Yaffe K, Falvey C, Hamilton N et al (2012) Diabetes, glucose control, and 9-year cognitive decline among older adults without dementia. Arch Neurol 69:1170–1175
Awad N, Gagnon M, Messier C (2004) The relationship between impaired glucose tolerance, type 2 diabetes, and cognitive function. J Clin Exp Neuropsychol 26:1044–1080
Saleem T, Mohammad KH, Abdel-Fattah MM, Abbasi AH (2008) Association of glycosylated haemoglobin level and diabetes mellitus duration with the severity of coronary artery disease. Diab Vasc Dis Res 5:184–189
Launer LJ, Miller ME, Williamson JD et al (2011) Effects of intensive glucose lowering on brain structure and function in people with type 2 diabetes (ACCORD MIND): a randomised open-label substudy. Lancet Neurol 10:969–977
Kerti L, Witte AV, Winkler A, Grittner U, Rujescu D, Flöel A (2013) Higher glucose levels associated with lower memory and reduced hippocampal microstructure. Neurology 81:1746–1752
Ramirez A, Wolfsgruber S, Lange C et al (2015) Elevated HbA1c is associated with increased risk of incident dementia in primary care patients. J Alzheimers Dis 44:1203–1212
McCrimmon RJ, Ryan CM, Frier BM (2012) Diabetes and cognitive dysfunction. Lancet 379:2291–2299
Rawlings AM, Sharrett AR, Mosley TH, Ballew SH, Deal JA, Selvin E (2017) Glucose peaks and the risk of dementia and 20-year cognitive decline. Diabetes Care 40:879–886
Ekblad LL, Rinne JO, Puukka P et al (2017) Insulin resistance predicts cognitive decline: an 11-year follow-up of a nationally representative adult population sample. Diabetes Care 40:751–758
Mõttus R, Luciano M, Sarr JM, McCarthy MI, Deary IJ (2015) Childhood cognitive ability moderates later-life manifestation of type 2 diabetes genetic risk. Health Psychol 34:915–919
Khan H, Sobki S, Khan S (2007) Association between glycaemic control and serum lipids profile in type 2 diabetic patients: HbA1c predicts dyslipidaemia. Clin Exp Med 7:24–29
Tesfaye S, Stevens L, Stephenson J et al (1996) Prevalence of diabetic peripheral neuropathy and its relation to glycaemic control and potential risk factors: the EURODIAB IDDM Complications Study. Diabetologia 39:1377–1384
Shpirer I, Rapoport MJ, Stav D, Elizur A (2012) Normal and elevated HbA1c levels correlate with severity of hypoxemia in patients with obstructive sleep apnea and decrease following CPAP treatment. Sleep Breath 16:461–466
Strachan MW, Reynolds RM, Marioni RE, Price JF (2011) Cognitive function, dementia and type 2 diabetes mellitus in the elderly. Nat Rev Endocrinol 7:108–114
Hassing LB, Hofer SM, Nilsson SE et al (2004) Comorbid type 2 diabetes mellitus and hypertension exacerbates cognitive decline: evidence from a longitudinal study. Age Ageing 33:355–361
Cukierman T, Gerstein H, Williamson J (2005) Cognitive decline and dementia in diabetes—systematic overview of prospective observational studies. Diabetologia 48:2460–2469
Mõttus R, Luciano M, Starr JM, Deary IJ (2013) Diabetes and life-long cognitive ability. J Psychosom Res 75:275–278
Deary IJ, Gow AJ, Taylor MD et al (2007) The Lothian Birth Cohort 1936: a study to examine influences on cognitive ageing from age 11 to age 70 and beyond. BMC Geriatr 7:28
Deary IJ, Gow AJ, Pattie A, Starr JM (2011) Cohort profile: the Lothian Birth Cohorts of 1921 and 1936. Int J Epidemiol 41:1576–1584
Deary IJ, Whalley LJ, Starr JM (2009) A lifetime of intelligence: follow-up studies of the Scottish mental surveys of 1932 and 1947. American Psychological Association, Washington, DC
Verhaeghen P, Salthouse TA (1997) Meta-analyses of age–cognition relations in adulthood: estimates of linear and nonlinear age effects and structural models. Psychol Bull 122:231–249
Horn JL, Cattell RB (1967) Age differences in fluid and crystallized intelligence. Acta Psychol 26:107–129
Ritchie SJ, Tucker-Drob EM, Cox SR et al (2016) Predictors of ageing-related decline across multiple cognitive functions. Intelligence 59:115–126
Wechsler D (1997) Adult Intelligence Scale. Psychological Corporation, San Antonio
Wechsler D (1997) Wechsler Memory Scale. Psychological Corporation, San Antonio
Deary IJ, Der G, Ford G (2001) Reaction times and intelligence differences: a population-based cohort study. Intelligence 29:389–399
Deary IJ, Johnson W, Starr JM (2010) Are processing speed tasks biomarkers of cognitive aging? Psychol Aging 25:219–228
Deary IJ, Simonotto E, Meyer M et al (2004) The functional anatomy of inspection time: an event-related fMRI study. NeuroImage 22:1466–1479
Nelson HE, Wilson J (1991) National Adult Reading Test (NART). Nfer-Nelson, Windsor
Wechsler D (2001) Wechsler Test of Adult Reading: WTAR. Psychological Corporation, San Antonio
Lezak MD, Howieson DB, Loring DW, Fischer JS (2004) Neuropsychological assessment. Oxford University Press, New York
Preacher KJ (2008) Latent growth curve modeling. Sage Publications, Los Angeles
Yuan K-H, Bentler PM (1997) Mean and covariance structure analysis: theoretical and practical improvements. J Am Stat Assoc 92:767–774
Rosseel Y (2012) Lavaan: an R package for structural equation modeling. J Stat Softw 48:1–36
Čukić I, Mõttus R, Luciano M, Starr JM, Weiss A, Deary IJ (2015) Do personality traits moderate the manifestation of type 2 diabetes genetic risk? J Psychosom Res 79:303–308
Spauwen P, Martens R, Stehouwer C et al (2016) Lower verbal intelligence is associated with diabetic complications and slower walking speed in people with type 2 diabetes: the Maastricht Study. Diabet Med 33:1632–1639
Deary IJ, Weiss A, Batty GD (2010) Intelligence and personality as predictors of illness and death: how researchers in differential psychology and chronic disease epidemiology are collaborating to understand and address health inequalities. Psychol Sci Public Interest 11:53–79
Calvin CM, Batty GD, Deary IJ (2011) Cognitive epidemiology: concepts, evidence, and future directions. In: Chamorro-Premuzic T, von Stumm S, Furnham A (eds) The Wiley-Blackwell handbook of individual differences. Blackwell Publishing, Chichester, pp 427–460
Batty GD, Deary IJ (2004) Early life intelligence and adult health: associations, plausible mechanisms, and public health importance are emerging. BMJ 329:585–586
Deary IJ, Batty GD (2007) Cognitive epidemiology. J Epidemiol Community Health 61:378–384
American Diabetes Association (2000) Type 2 diabetes in children and adolescents. Pediatrics 105:671–680
Geijselaers SL, Sep SJ, Claessens D et al (2017) The role of hyperglycemia, insulin resistance, and blood pressure in diabetes-associated differences in cognitive performance—the Maastricht Study. Diabetes Care 40:1537–1547
Feinkohl I, Keller M, Robertson CM et al (2015) Cardiovascular risk factors and cognitive decline in older people with type 2 diabetes. Diabetologia 58:1637–1645
Acknowledgements
The LBC1936 study is funded by Age UK (The Disconnected Mind project). We thank the Scottish Council for Research in Education for allowing access to SMS1947. We thank the LBC1936 study participants and research team members.
Funding
The LBC1936 data were collected using a Research into Ageing programme grant; this research continues as part of the Age UK-funded Disconnected Mind project. DMA, JMS and IJD are members of The University of Edinburgh Centre for Cognitive Ageing and Cognitive Epidemiology, which is funded by the Biotechnology and Biological Sciences Research Council and Medical Research Council (MR/K026992/1).
Author information
Authors and Affiliations
Contributions
DMA performed the analyses and drafted the manuscript. JMS assisted in the study design, and critically reviewed the analyses and manuscript. IJD conceptualised the study, assisted in the study design, data analysis, drafting and critical review of the manuscript. All authors approved the final manuscript. DMA is responsible for the integrity of the work as a whole.
Corresponding author
Ethics declarations
The authors declare that there is no duality of interest associated with this manuscript.
Electronic supplementary material
ESM
(PDF 896 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Altschul, D.M., Starr, J.M. & Deary, I.J. Cognitive function in early and later life is associated with blood glucose in older individuals: analysis of the Lothian Birth Cohort of 1936. Diabetologia 61, 1946–1955 (2018). https://doi.org/10.1007/s00125-018-4645-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-018-4645-8