Abstract
Purpose
Despite standardized treatment algorithms, patients with complex elbow fracture-dislocation frequently suffer from poor post-operative elbow function leading to reduced quality of life. Up to now, there is no valuable data regarding risk factors that lead to poor post-operative outcome after surgical reconstruction of complex elbow fracture-dislocations.
Methods
From 06/2010 to 12/2020 134 patients (51.3 ± 15.1 years, 44% women) undergoing surgical treatment of complex elbow fracture-dislocations could be included in this study. Follow-up period was 4.4 years (SD 2.5). All patients were clinically evaluated for elbow movement, elbow stability and common elbow scores (MEPS, OES, DASH-Score). Potential risk factors for poor post-operative outcome were identified using bi- and multivariate analyses.
Results
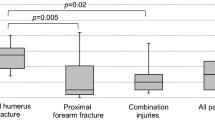
Overall good post-operative outcome has been achieved, mean MEPS was 88.8 ± 17.6. Post-operative complications occurred in 31.3% of the cases, while 25.4% required surgical revision. Patients with transolecranon dislocation fractures showed the significantly worst functional outcomes (p = 0.01). In addition, it has been shown that a patient’s age of more than 70 years (OR = 10, p = 0.003) and a BMI of more than 35 kg/m2 (OR = 7.6, p = 0.004) are independent risk factors for a poor post-operative outcome. In contrast, gender and time to surgery showed no significant influence on post-operative outcome.
Conclusion
In most cases, good post-operative functional results can be achieved using standardized treatment protocols. However, complication and revision rates remain high. Patients older than 70 years of age or with a BMI over 35 kg/m2 are at risk for an inferior outcome and require close follow-up monitoring.



Similar content being viewed by others
Data availability
Not applicable.
References
Josefsson PO, Nilsson BE. Incidence of elbow dislocation. Acta Orthop Scand. 1986. https://doi.org/10.3109/17453678609014788
Stoneback JW, Owens BD, Sykes J, Athwal GS, Pointer L, Wolf JM. Incidence of elbow dislocations in the United States population. J Bone Joint Surg Am. 2012. https://doi.org/10.2106/JBJS.J.01663
Siebenlist S, Braun KF. (2017) Elbow dislocation fractures. Unfallchirurg https://doi.org/10.1007/s00113-017-0373-7
Chan K, King GJW, Faber KJ. Treatment of complex elbow fracture-dislocations. Curr Rev Musculoskelet Med https://doi. 2016. https://doi.org/10.1007/s12178-016-9337-8
Rodriguez-Martin J, Pretell-Mazzini J, Andres-Esteban EM, Larrainzar-Garijo R. Outcomes after terrible triads of the elbow treated with the current surgical protocols. A review. Int Orthop. 2011. https://doi.org/10.1007/s00264-010-1024-6
Hotchkiss RN. Displaced fractures of the Radial Head: internal fixation or excision? J Am Acad Orthop Surg. 1997. https://doi.org/10.5435/00124635-199701000-00001
O’Driscoll SW, Jupiter JB, Cohen MS, Ring D, McKee MD. Difficult elbow fractures: pearls and pitfalls. Instr Course Lect. 2003;52:113–34.
Gustilo RB, Anderson JT. Prevention of infection in the treatment of one thousand and twenty-five open fractures of long bones: retrospective and prospective analyses. J Bone Joint Surg Am. 1976;58:4:453–8.
Doyle DJ, Hendrix JM, Garmon EH. American Society of Anesthesiologists Classification. StatPearls Publishing: In StatPearls; 2023.
Schreiber JJ, Paul S, Hotchkiss RN, Daluiski A. Conservative management of elbow dislocations with an overhead motion protocol. J Hand Surg Am. 2015. https://doi.org/10.1016/j.jhsa.2014.11.016
Lee AT, et al. The influence of gravity on the unstable elbow. J Shoulder Elb Surg. 2013. https://doi.org/10.1016/j.jse.2012.08.012
Schneeberger AG, Morrey BF. (2009) Semiconstrained Elbow Replacement: Results in Traumatic Conditions. In: Morrey’s The Elbow and Its Disorders (Fourth Edition) https://doi.org/10.1016/B978-1-4160-2902-1.50062-0
Dawson J, et al. The development and validation of a patient-reported questionnaire to assess outcomes of elbow surgery. J Bone Joint Surg Br. 2008. https://doi.org/10.1302/0301-620X.90B4.20290
Gummesson C, Atroshi I, Ekdahl C. The disabilities of the arm, shoulder and hand (DASH) outcome questionnaire: longitudinal construct validity and measuring self-rated health change after surgery. BMC Musculoskelet Disord. 2003. https://doi.org/10.1186/1471-2474-4-11
Lindenhovius A, Karanicolas PJ, Bhandari M, Ring D, Collaborative COAST. Radiographic arthrosis after elbow trauma: interobserver reliability. J Hand Surg Am. 2012. https://doi.org/10.1016/j.jhsa.2011.12.043
Hastings H, Graham TJ. The classification and treatment of heterotopic ossification about the elbow and forearm. Hand Clin. 1994;103:417–37.
Pierrat J, Bégué T, Mansat P, GEEC. Terrible triad of the elbow: treatment protocol and outcome in a series of eighteen cases. Injury. 2015. https://doi.org/10.1016/S0020-1383(15)70004-5
Pugh DMW, Wild LM, Schemitsch EH, King GJW, McKee MD. Standard surgical protocol to treat elbow dislocations with radial head and coronoid fractures. J Bone Joint Surg Am. 2004. https://doi.org/10.2106/00004623-200406000-00002
Heck S, Gick S, Dargel J, Pennig D, Unfallchirurg. https://doi.org/10.1007/s00113-010-1929-y
Macchi M, Spezia M, Elli S, Schiaffini G, Chisari E. Obesity increases the risk of Tendinopathy, Tendon tear and rupture, and postoperative complications: a systematic review of Clinical studies. Clin Orthop Relat Res. 2020. https://doi.org/10.1097/CORR.0000000000001261
Liu Q, Wu M, Orgill DP, Bai X, Panayi AC. The effect of obesity on inpatient outcomes in lower extremity trauma: a systematic review and meta-analysis. J Trauma Acute Care Surg. 2022. https://doi.org/10.1097/TA.0000000000003328
Rinonapoli G, et al. Obesity and bone: a complex relationship. Int J Mol Sci. 2021. https://doi.org/10.3390/ijms222413662
Morrey ME, Hevesi M. (2018) The influence of obesity on total elbow arthroplasty. Orthop Clin North Am https://doi.org/10.1016/j.ocl.2018.02.009
Cao JJ. Effects of obesity on bone metabolism. J Orthop Surg Res. 2011. https://doi.org/10.1186/1749-799X-6-30
Kim DH et al. (2023) Association of behavior pattern with overweight and obesity in South Korean adults-A multi correspondence analysis (KNHANES-2018-2020). PLOS Glob Public Health https://doi.org/10.1371/journal.pgph.0002384
Anderson K, Hamm RL. Factors that impair Wound Healing. J Am Coll Clin Wound Spec https://doi. 2012. https://doi.org/10.1016/j.jccw.2014.03.001
Foulke BA, Kendal AR, Murray DW, Pandit H, Maturitas. https://doi.org/10.1016/j.maturitas.2016.07.014
Onizuka N, Switzer J, Myeroff C. Management of geriatric elbow Injury. Orthop Clin North Am. 2021. https://doi.org/10.1016/j.ocl.2021.05.009
Lobstein T, Jackson-Leach R, Powis J, Brinsden H, Gray M. (2023) World Obesity Atlas 2023. World Obesity Federation, United Kingdom. https://policycommons.net/artifacts/3454894/untitled/4255209/. Accessed 4 December 2023.
Funding
The authors declare that no benefit in any form have been received or will be received from a commercial party related directly or indirectly to the preparation and the subject of this manuscript.
Author information
Authors and Affiliations
Contributions
Tim Jakobi: Conceptualized and designed the study, Examined the patients, Analysed and interpreted the data, Performed the statistical analysis, Wrote and revised the manuscript.
Yves Gramlich: Proofread the manuscript, Analysed the data.
Matthias Sauter: Proofread the manuscript, Analysed the data.
Matthias Schnetz: Proofread the manuscript, Analysed the data.
Reinhard Hoffmann: Proofread the manuscript, Conceived, and designed the study, Provided administrative, technical, and material support.
Alexander Klug: Proofread the manuscript, Reviewed the literature, Analysed the data, Provided administrative, technical, and material support.
Corresponding author
Ethics declarations
Ethics approval
The study has been approved by the Ethical Committee of the Regional Medical board of Hessen, Germany (FF3/2019). All investigations were conducted in conformity with the principles of good clinical practice and the ethical principles of research.
Informed consent
was obtained from all individual participants included in the study.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent to publish
There is no individual participant data in our manuscript.
Competing interests
The authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Jakobi, T., Gramlich, Y., Sauter, M. et al. Complex elbow fracture-dislocations– what factors are associated with a poor post-operative outcome?. Eur J Trauma Emerg Surg (2024). https://doi.org/10.1007/s00068-024-02531-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00068-024-02531-w