Abstract
Purpose
The rate of surgical site infection (SSI) after surgery for secondary peritonitis is very high. This study investigated the relationship between intraoperative procedures of emergency surgery for nonappendiceal perforation peritonitis and deep incisional or organ-space SSI.
Methods
This prospective, two-center observational study included patients aged ≥ 20 years who underwent emergency surgery for perforation peritonitis between April 2017 and March 2020. We compared patients with deep incisional or organ-space SSI (Group S) to patients without SSIs or with superficial incisional SSIs (Group C). Thereafter, we evaluated the association between intraoperative technical variables and deep incisional or organ-space SSI using a multivariate logistic regression model. All multivariate analyses were adjusted for potentially relevant risk factors (e.g., age, body mass index, diabetes, smoking habit, and National Nosocomial Infection Surveillance risk index).
Results
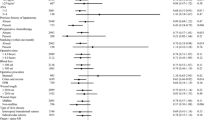
Of the 75 participants, 14 were in Group S and 61 were in Group C. The use of a wound protector device was significantly associated with decreased odds of deep incisional or organ-space SSI (adjusted odds ratios [AOR], 0.017; 95% confidence intervals [CI] 0.0014–0.19, p = 0.0011). A 1000 ml increase in intra-abdominal lavage with normal saline was significantly associated with increased odds of deep incisional or organ-space SSI (AOR: 1.28, 95% CI 1.02–1.61, p = 0.033).
Conclusion
Wound protector devices should be used in emergency surgery for nonappendiceal perforation peritonitis. Excessive intra-abdominal lavage with normal saline for peritonitis may have unsatisfactory benefits and increases the incidence of deep incisional or organ-space SSI.

Similar content being viewed by others
Data availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
World Health Organization (2018) Global guidelines for the prevention of surgical site infection, second edition. https://apps.who.int/iris/bitstream/handle/10665/277399/9789241550475-eng.pdf. Accessed 23 Jan 2022
Kusachi S, Kashimura N, Konishi T, Shimizu J, Kusunoki M, Oka M, et al. Length of stay and cost for surgical site infection after abdominal and cardiac surgery in Japanese hospitals: multi-center surveillance. Surg Infect (Larchmt). 2012;13:257–65. https://doi.org/10.1089/sur.2011.007.
Horan TC, Gaynes RP, Martone WJ, Jarvis WR, Emori TG. CDC definitions of nosocomial surgical site infections, 1992: a modification of CDC definitions of surgical wound infections. Am J Infect Control. 1992;20:271–4. https://doi.org/10.1016/s0196-6553(05)80201-9.
Gibbons C, Bruce J, Carpenter J, Wilson AP, Wilson J, Pearson A, et al. Identification of risk factors by systematic review and development of risk-adjusted models for surgical site infection. Health Technol Assess. 2011;15:1–156. https://doi.org/10.3310/hta15300.
Korol E, Johnston K, Waser N, Sifakis F, Jafri HS, Lo M, et al. A systematic review of risk factors associated with surgical site infections among surgical patients. PLoS ONE. 2013;8:e83743. https://doi.org/10.1371/journal.pone.0083743.
Zhang Y, Zheng QJ, Wang S, Zeng SX, Zhang YP, Bai XJ, et al. Diabetes mellitus is associated with increased risk of surgical site infections: a meta-analysis of prospective cohort studies. Am J Infect Control. 2015;43:810–5. https://doi.org/10.1016/j.ajic.2015.04.003.
Marchi M, Pan A, Gagliotti C, Morsillo F, Parenti M, Resi D, et al. The Italian national surgical site infection surveillance programme and its positive impact, 2009 to 2011. Euro Surveill. 2014;19:20815. https://doi.org/10.2807/1560-7917.es2014.19.21.20815.
Lee KY, Coleman K, Paech D, Norris S, Tan JT. The epidemiology and cost of surgical site infections in Korea: a systematic review. J Korean Surg Soc. 2011;81:295–307. https://doi.org/10.4174/jkss.2011.81.5.295.
Lawson EH, Hall BL, Ko CY. Risk factors for superficial vs deep/organ-space surgical site infections: implications for quality improvement initiatives. JAMA Surg. 2013;148:849–58. https://doi.org/10.1001/jamasurg.2013.2925.
Schein M, Gecelter G, Freinkel W, Gerding H, Becker PJ. Peritoneal lavage in abdominal sepsis. A controlled clinical study. Arch Surg. 1990;125:1132–5. https://doi.org/10.1001/archsurg.1990.01410210058008.
Doklestić SK, Bajec DD, Djukić RV, Bumbaširević V, Detanac AD, Detanac SD, et al. Secondary peritonitis – evaluation of 204 cases and literature review. J Med Life. 2014;7:132–8.
Berríos-Torres SI, Umscheid CA, Bratzler DW, Leas B, Stone EC, Kelz RR, et al. Centers for Disease Control and Prevention guideline for the prevention of surgical site infection, 2017. JAMA Surg. 2017;152:784–91. https://doi.org/10.1001/jamasurg.2017.0904.
National Institute for Health and Care Excellence. Surgical site infections. Prev Treat. 2019. https://www.nice.org.uk/guidance/ng125. Accessed 23 Jan 2022
Anderson DJ, Podgorny K, Berríos-Torres SI, Bratzler DW, Dellinger EP, Greene L, et al. Strategies to prevent surgical site infections in acute care hospitals: 2014 update. Infect Control Hosp Epidemiol. 2014;35:605–27. https://doi.org/10.1086/676022.
Linder MM, Wacha H, Feldmann U, Wesch G, Streifensand RA, Gundlach E. The Mannheim peritonitis index. An instrument for the intraoperative prognosis of peritonitis [Article in German]. Chirurg. 1987;58:84–92.
Billing A, Fröhlich D, Schildberg FW. Prediction of outcome using the Mannheim peritonitis index in 2003 patients. Peritonitis Study Group Br J Surg. 1994;81:209–13. https://doi.org/10.1002/bjs.1800810217.
Culver DH, Horan TC, Gaynes RP, Martone WJ, Jarvis WR, Emori TG, et al. Surgical wound infection rates by wound class, operative procedure, and patient risk index. National Nosocomial Infections Surveillance System. Am J Med. 1991;91:152–7. https://doi.org/10.1016/0002-9343(91)90361-z.
Mazuski JE, Solomkin JS. Intra-abdominal infections. Surg Clin North Am. 2009;89:421–37. https://doi.org/10.1016/j.suc.2008.12.001.
Lee P, Waxman K, Taylor B, Yim S. Use of wound-protection system and postoperative wound-infection rates in open appendectomy: a randomized prospective trial. Arch Surg. 2009;144:872–5. https://doi.org/10.1001/archsurg.2009.151.
Pinkney TD, Calvert M, Bartlett DC, Gheorghe A, Redman V, Dowswell G, et al. Impact of wound edge protection devices on surgical site infection after laparotomy: multicentre randomised controlled trial (ROSSINI Trial). BMJ. 2013;347:f4305. https://doi.org/10.1136/bmj.f4305.
Whiteside OJ, Tytherleigh MG, Thrush S, Farouk R, Galland RB. Intra-operative peritoneal lavage—who does it and why? Ann R Coll Surg Engl. 2005;87:255–8. https://doi.org/10.1308/1478708051847.
Burnett WE, Brown GR Jr, Rosemond GP, Caswell HT, Buchor RB, Tyson RR. The treatment of peritonitis using peritoneal lavage. Ann Surg. 1957;145:675–82. https://doi.org/10.1097/00000658-195705000-00009.
Thom H, Norman G, Welton NJ, Crosbie EJ, Blazeby J, Dumville JC. Intra-cavity lavage and wound irrigation for prevention of surgical site infection: systematic review and network meta-analysis. Surg Infect (Larchmt). 2021;22:144–67. https://doi.org/10.1089/sur.2019.318.
Edmiston CE Jr, Goheen MP, Kornhall S, Jones FE, Condon RE. Fecal peritonitis: microbial adherence to serosal mesothelium and resistance to peritoneal lavage. World J Surg. 1990;14:176–83. https://doi.org/10.1007/BF01664870.
Mashbari H, Hemdi M, Chow KL, Doherty JC, Merlotti GJ, Salzman SL, et al. A randomized controlled trial on intra-abdominal irrigation during emergency trauma laparotomy; time for yet another paradigm shift. Bull Emerg Trauma. 2018;6:100–7. https://doi.org/10.29252/beat-060203.
Tanaka K, Matsuo K, Kawaguchi D, Murakami T, Hiroshima Y, Hirano A, et al. Randomized clinical trial of peritoneal lavage for preventing surgical site infection in elective liver surgery. J Hepatobiliary Pancreat Sci. 2015;22:446–53. https://doi.org/10.1002/jhbp.222.
Bustamante Montalvo M, Cainzos M, Prieto Carreiras L, Castiñeira Piñeiro A, García Iglesias A, Fernandez Novo A, et al. Evaluation of the effect of triclosan coated sutures in the prevention of surgical site infections in a Spanish Hospital setting: a prospective, observational study. Infect Prev Pract. 2021;3:100154. https://doi.org/10.1016/j.infpip.2021.100154.
Ruiz-Tovar J, Alonso N, Morales V, Llavero C. Association between triclosan-coated sutures for abdominal wall closure and incisional surgical site infection after open surgery in patients presenting with fecal peritonitis: a randomized clinical trial. Surg Infect (Larchmt). 2015;16:588–94. https://doi.org/10.1089/sur.2014.072.
Mingmalairak C, Ungbhakorn P, Paocharoen V. Efficacy of antimicrobial coating suture coated polyglactin 910 with tricosan (Vicryl plus) compared with polyglactin 910 (Vicryl) in reduced surgical site infection of appendicitis, double blind randomized control trial, preliminary safety report. J Med Assoc Thai. 2009;92:770–5.
Ward WG Sr, Cooper JM, Lippert D, Kablawi RO, Neiberg RH, Sherertz RJ. Glove and gown effects on intraoperative bacterial contamination. Ann Surg. 2014;259:591–7. https://doi.org/10.1097/SLA.0b013e3182a6f2d9.
Zdanowski Z, Danielsson G, Jonung T, Norgren L, Ribbe E, Thörne J, et al. Intraoperative contamination of synthetic vascular grafts. Effect of glove change before graft implantation. A prospective randomised study. Eur J Vasc Endovasc Surg. 2000;19:283–7. https://doi.org/10.1053/ejvs.1999.1035.
Narice BF, Almeida JR, Farrell T, Madhuvrata P. Impact of changing gloves during cesarean section on postoperative infective complications: a systematic review and meta-analysis. Acta Obstet Gynecol Scand. 2021;100:1581–94. https://doi.org/10.1111/aogs.14161.
Acknowledgements
The authors are grateful to Kyohei Miyamoto for providing their statistical expertise and Editage (http://www.editage.com) for the English language editing.
Funding
No sources of funding are declared.
Author information
Authors and Affiliations
Contributions
YO contributed to the study design and drafted the article. All authors contributed to the acquisition and analysis of the data. YO, KU, TN, SKw, and KK contributed to the data interpretation. MM, MI, SU, and SKt contributed to reviewing, editing, and supervision. All the authors participated in revising the article and have read, approved the final version of manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethics approval and consent to participate
This study was conducted according to the principles of the Declaration of Helsinki. The study protocol was approved by the Research Ethics Committee of the Wakayama Medical University Hospital and the Research Ethics Committee of the Japanese Red Cross Wakayama Medical Center. The Research Ethics Committee of the Wakayama Medical University Hospital and the Research Ethics Committee of the Japanese Red Cross Wakayama Medical Center waived the need for documentation of informed consent due to the prospective but non-randomized and observational nature of the study; The Research Ethics Committee of the Wakayama Medical University Hospital and the Research Ethics Committee of the Japanese Red Cross Wakayama Medical Center approved verval informed consent procedure.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Okishio, Y., Ueda, K., Nasu, T. et al. Intraoperative techniques to prevent deep incisional or organ-space surgical site infection after emergency surgery for nonappendiceal perforation peritonitis: a prospective two-center observational study. Eur J Trauma Emerg Surg 49, 2215–2224 (2023). https://doi.org/10.1007/s00068-023-02301-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-023-02301-0