Abstract
Purpose
The non-operative management of extradural hemorrhage in the pediatric age group has been increasingly considered in the last decade with good clinical outcomes and comparable results to surgical intervention in carefully selected patients. The purpose of this study is to evaluate the outcome of observation in the management of pediatric patients with extra dural hematoma.
Patients and methods
All consecutive pediatric patients with traumatic EDH after TBI who were presented to a single neurosurgical institution between January, 2008 and November, 2018 were retrospectively reviewed. Mechanism of injury, Glasgow coma scale (GCS) on admission, presenting neurological examination, treatment modality, the first and last imaging findings, and outcome were analyzed. The outcome was measured using the Glasgow outcome scale (GOS) on discharge from the hospital.
Results
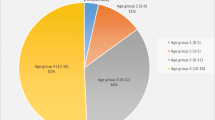
A total of 83 patients were identified. The median age was 7.1 years (0.8–14 years) and 67% of the patients were male (n = 56). The median thickness of acute EDH was 1.1 cm (0.2–2.6 cm).
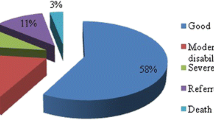
44 patients were managed conservatively with a close observation at a specialized neurotrauma unit for any clinical deterioration, and the remaining 39 patients were managed surgically. There was no significant difference in the patients age, hematoma thickness, presence of skull fractures, systemic injuries, and other types of cerebral injuries between the two groups. The presenting GCS was significantly lower in the surgical group which reflects the severity of the injury. Hospital stay was significantly longer among the surgical group, and the GOS was significantly better in the non-surgical group.
The majority of the surgical group showed complete resolution of the hematoma on discharge, while only 50% of the non-surgical patients (n = 22) had a complete resolution of the hematoma one month after the TBI.
Conclusion
The conservative management is applicable in carefully selected pediatric patients with acute traumatic extradural hematoma provided that the observation is accomplished in a well-established and equipped neurosurgical unit. These results are congruent with similar earlier studies.


Similar content being viewed by others
Abbreviations
- CT:
-
Computed tomography
- EDH:
-
Extradural hematoma
- GCS:
-
Glasgow coma scale
- CSF:
-
Cerebrospinal fluid
- GOS:
-
Glasgow outcome score
- TBI:
-
Traumatic brain injury
References
Duhaime AC, Alario AJ, Lewander WJ, Schut L, Sutton LN, Seidl TS, Nudelman S, Budenz D, Hertle R, Tsiaras W, Loporchio S. Head injury in very young children: mechanisms, injury types, and ophthalmologic findings in 100 hospitalized patients younger than 2 years of age. Pediatrics. 1992;90:179–85.
McLaurin R. Towbin R Posttraumatic hematomas. In: McLaurin R, Schult L, Veres J, Epstein F, editors. Pediatric neurosurgery. 2nd ed. Philadelphia: Saunders; 1989. p. 277–289.
Binder H, Majdan M, Tiefenboeck TM, Fochtmann A, Michel M, Hajdu S, Mauritz W, Leitgeb J. Management and outcome of traumatic epidural hematoma in 41 infants and children from a single center. Orthop Traumatol Surg Res. 2016;102:769–74.
Beni-Adani L, Flores I, Spektor S, Umansky F, Constantini S. Epidural hematoma in infants: a different entity? J Trauma Acute Care Surg. 1999;1999(46):306–11.
Pang D, Horton JA, Herron JM, Wilberger JE Jr, Vries JK. Nonsurgical management of extradural hematomas in children. J Neurosurg. 1983;59:958–71.
Knuckey NW, Gelbard S, Epstein MH. The management of “asymptomatic” epidural hematomas: a prospective study. J Neurosurg. 1989;1989(70):392–6.
Chen TY, Wong CW, Chang CN, Lui TN, Cheng WC, Tsai MD, Lin TK. The expectant treatment of “asymptomatic” supratentorial epidural hematomas. Neurosurgery. 1993;1993(32):176–9.
Pillay R, Peter JC. Extradural haematomas in children. S Afr Med J. 1995;1995(85):672–4.
Bullock MR, Chesnut R, Ghajar J, Gordon D, Hartl R, Newell DW, Servadei F, Walters BC, Wilberger JE. Surgical management of acute subdural hematomas. Neurosurgery. 2006;58:S2–16.
Jamous MA, Aziz HA, Al Kaisy F, Eloqayli H, Azab M, Al-Jarrah M. Conservative management of acute epidural hematoma in a pediatric age group. Pediatr Neurosurg. 2009;45:181–4.
Basamh M, Robert A, Lamoureux J, Saluja RS, Marcoux J. Epidural hematoma treated conservatively: when to expect the worst. Can J Neurol Sci. 2016;2016(43):74–81.
Balmer B, Boltshauser E, Altermatt S, Gobet R. Conservative management of significant epidural haematomas in children. Childs Nerv Syst. 2006;2006(22):363–7.
Paiva WS, Andrade AFD, Mathias Júnior L, Guirado VMDP, Amorim RL, Magrini NN, Teixeira MJ. Management of supratentorial epidural hematoma in children: report on 49 patients. Arq Neuropsiquiatr. 2010;68:888–92.
Teichert JH, Rosales PR Jr, Lopes PB, Enéas LV, Da Rocha TS. Extradural hematoma in children: case series of 33 patients. Pediatr Neurosurg. 2012;48:216–20.
Skadorwa T, Zygańska E, Eibl M, Ciszek B. Distinct strategies in the treatment of epidural hematoma in children: clinical considerations. Pediatr Neurosurg. 2013;2013(49):166–71.
Flaherty BF, Moore HE, Riva-Cambrin J, Bratton SL. Pediatric patients with traumatic epidural hematoma at low risk for deterioration and need for surgical treatment. J Pediatr Surg. 2017;52:334–9.
Champagne PO, He KX, Mercier C, Weil AG, Crevier L. Conservative management of large traumatic supratentorial epidural hematoma in the pediatric population. Pediatr Neurosurg. 2017;52:168–72.
Bezircioglu H, Ersahin Y, Demircivi F, Yurt I, Donertas K, Tektas S. Nonoperative treatment of acute extradural hematomas: analysis of 80 cases. J Trauma Acute Care Surg. 1996;41:696–8.
Salama MM, Eissa EM. Conservative management of extradural hematoma: experience with 70 cases. Egypt J Neurol Surg. 2010;25:185–94.
Mayr R, Troyer S, Kastenberger T, Krappinger D, Rosenberger R, Obwegeser A, El Attal R. The impact of coagulopathy on the outcome of traumatic epidural hematoma. Arch Orthop Trauma Surg. 2012;132:1445–500.
Ding J, Yuan F, Guo Y, Chen SW, Gao WW, Wang G, Cao HL, Ju SM, Chen H, Zhang PQ, Tian HL. A prospective clinical study of routine repeat computed tomography (CT) after traumatic brain injury (TBI). Brain Inj. 2012;26:1211–6.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author discloses no conflict of interest.
Ethical approval
This article is compliant with the ethical standards. It was not funded from any source.
Informed consent
Informed consent and ethical approval are not applicable for this article because of its retrospective nature.
Rights and permissions
About this article
Cite this article
Jamous, M.A. The outcome of observation of acute traumatic extradural hemorrhage in pediatric age group. Eur J Trauma Emerg Surg 47, 847–853 (2021). https://doi.org/10.1007/s00068-019-01262-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-019-01262-7