Abstract
Objective
To examine the outcomes of trauma patients who tested positive for alcohol at the time of hospital arrival versus those who tested negative.
Methods
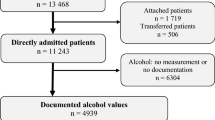
Data were pulled from the National Trauma Data Bank (2007–2010). All injured patients who were ≥14 years of age, sustained a “blunt” or “penetrating” injury, had complete systolic blood pressure (SBP) and heart rate (HR) records, were taken to a level 1 or 2 trauma center, and who received a confirmed blood alcohol test were included in the study. Any blood alcohol concentration (BAC) above the legal limit (≥0.08 g/dL) was considered “positive” for alcohol, and if no alcohol was identified it was considered “negative”. Patients’ demography and clinical information were compared across groups using Chi-square and Wilcoxon rank sum tests. Logistic regression, propensity score matching, and a follow-up paired analysis were also performed.
Results
Of 279,460 total patients, around one-third of the patients (92,960) tested positive for BAC. There were clear demographic differences found between the two groups regarding age, gender, race, and injury type. There was also a significantly higher mortality rate (4.3 vs. 3.1%, P < 0.001) and a longer hospital length of stay (4 vs. 3 days, P < 0.001) found in the alcohol-negative group. Propensity score matching was also performed resulting in 92,959 patients per group. Using the paired data, the overall mortality observed was 3.1 vs. 3.3% (P = 0.035) between the alcohol-positive and alcohol-negative groups, respectively. There was no significant difference noted in the total hospital length of stay (median: 3 vs. 4 days, P = 0.84).
Conclusion
Patients who tested positive for alcohol following a traumatic injury showed no clinically significant reduction in mortality and no significant difference in total hospital length of stay.


Similar content being viewed by others
References
National Trauma Institute: Trauma Statistics. Posted in February 2014. Available at: http://www.nationaltraumainstitute.org/home/trauma_statistics.html. Accessed on January 05, 2016.
World Health Organization. Global status report on alcohol and health, p. XIII. 2014 ed. Available at: http://www.who.int/substance_abuse/publications/global_alcohol_report/msb_gsr_2014_1.pdf?ua=1. Accessed on January 05, 2016.
National Highway Traffic Safety Administration. 2013 motor vehicle crashes: Overview. Available at: http://www-nrd.nhtsa.dot.gov/Pubs/812101.pdf. Accessed on January 05, 2016.
Fulde GW, Smith M, Forster SL. Presentations with alcohol-related serious injury to a major Sydney trauma hospital after 2014 changes to liquor laws. MJA. 2015;203(9):366.
Gottesfeld Z, Moore AN, Dash PK. Acute ethanol intake attenuates inflammatory cytokines after brain injury in rats: a possible role for corticosterone. J of Neurotrauma. 2002;19(3):317–26.
Kelly DF, Lee SM, Pinanong PA, Hovda DA. Paradoxical effects of acute ethanolism in experimental brain injury. J of Neurosurgery. 1997;86(5):876–82.
Taylor AN, Sutton RL (2015) Evidence for beneficial and adverse effects of alcohol in animal models and clinical studies of traumatic brain injury. In: FH Kobeissy (Ed.) Brain neurotrauma: molecular, neuropsychological, and rehabilitation aspects. Boca Raton (FL): by Taylor and Francis Group, LLC.
Schutte C, Hanks R. Impact of the presence of alcohol at the time of injury on acute and one-year cognitive and functional recovery after traumatic brain injury. Int J Neurosci. 2010;120(8):551–6.
Raj R, Skrifvars MB, Kivisaari R, Hernesniemi J, Lappalainen J, Siironen J. Acute alcohol intoxication and long-term outcome in patients with traumatic brain injury. J Neurotrauma. 2015;32(2):95–100. doi:10.1089/neu.2014.3488 (Epub 2014 Nov 13).
Brennan JH, Bernard S, Cameron PA, Rosenfeld JV, Mitra B. Ethanol and isolated traumatic brain injury. J Clin Neurosci. 2015;22(9):1375–81. doi:10.1016/j.jocn.2015.02.030 (Epub 2015 Jun 9).
Hadjizacharia P, O’Keeffe T, Pleurad DS, Green DJ, Brown CV, Chan LS, et al. Alcohol exposure and outcomes in trauma patients. Eur J Trauma Emerg Surg. 2011;37:169–75.
Zeckery C, Dannecker S, Hildebrand F, Mommsen P, Scherer R et al. Alcohol and multiple trauma-is there an influence on the outcome? Alcohol 2011;45(3):245–51. doi:10.1016/j.alcohol.2010.08.004.
Allison, Paul D. Measures of Fit for Logistic Regression. SAS Global Forum, March 25, 2014, Washington, DC. Unpublished conference paper. Statistical Horizons LLC, Philadelphia, PA, 2015. http://statisticalhorizons.com/wp-content/uploads/GOFForLogisticRegression-Paper.pdf. Accessed 3 Aug 2015.
Sing T, Sander O, Beerenwinkel N, Lengauer T (2005) ROCR: visualizing classifier performance in R. _Bioinformatics_, *21*(20), pp. 7881. http://rocr.bioinf.mpi-sb.mpg.de. Accessed 18 Sept 2015.
Rosenbaum PR, Rubin DB. The central role of the propensity score in observational studies for causal effects. Biometrika. 1983;70(1):41–55. doi:10.1093/biomet/70.1.41.
Ho DE, Imai K, King G, Stuart EA (2011) MatchIt: Nonparametric Preprocessing for Parametric Causal Inference. Journal of Statistical Software, vol. 42, No. 8, pp. 1–28. http://www.jstatsoft.org/v42/i08/. Accessed 30 Sept 2015.
Hothorn T, Hornik K, van de Wiel MA, Zeileis A (2008). Implementing a class of permutation tests: the coin package. Journal of Statistical Software 28(8), 1–23. http://www.jstatsoft.org/v28/i08/. Accessed 18 Sept 2015.
Therneau T(2015). _A Package for Survival Analysis in R_. R package version 2.38–3. http://CRAN.R-project.org/package=survival.
Therneau Terry M, Grambsch Patricia M. Modeling survival data: extending the cox model. New York: Springer; 2000. ISBN 0-387-98784-3.
R Core Team (2014). R: a language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. http://www.R-project.org/.
StataCorp. Stata Statistical Software: Release 13. College Station, TX: StataCorp LP. 2013.
Kelly DF, Kozlowski DA, Haddad E, Echiverri A, Hovda DA, Lee SM. Ethanol reduces metabolic uncoupling following experimental head injury. J Neurotrauma. 2000;17:261–72.
Lustenberger T, Inaba K, Bamparas G, Talving P, Pleurad D, Lam L, Konstantinidis A, Demetriades D. Ehtanol intoxication is associated with lower incidence of admission coagulopathy in severe traumatic brain injury patients. J Neurotrauma. 2011;28(9):1699–706.
Talving P, Pleurad D, Bamparas G, Dubose J, Inaba K, Lam L, Chan L. Demetriades Isolated severe traumatic brain injuries: association of blood alcohol levels with the severity of injuries and outcomes. J Trauma. 2010;68(2):357–62.
De Guise E, Leblanc J, Dagherb J, Lamoureuxc J, Jishid AA, Malekid M, Marcouxd J, Feyza M. Outcome in patients with traumatic brain injury, pre-injury alcohol abuse and intoxication at time of injury. Brain Inj. 2009;23(11):853–65. doi:10.1080/02699050903283221.
Wagner N, Akbarpour A, Mörs K, Voth M, Störmann P, et al. Alcohol intoxication reduces systemic interleukin-6 levels and leukocyte counts after severe TBI compared with not intoxicated TBI patients. Shock. 2016;3:261–9.
Relja B, Menke J, Wagner N, Auner B, Voth M, et al. Effect of positive blood alcohol concentration on outcome and systemic interleukin-6 in major trauma patients. Injury. 2016;47:640–5.
Rootman DB, Mustard R, Kalia V, Ahmed N. Increased incidence of complications in trauma patients co-intoxicated with alcohol and other drugs. J Trauma. 2007;62:755–8.
Plurad D, Demetriades D, Gruzinski G, Preston C, Chan L, Gaspard D, et al. Motor vehicle crashes: the association of alcohol consumption with the type and severity of injuries and outcomes. J Emerg Med. 2010;38:12–7.
Stϋbig T, Petri M, Zeckery C, Brand S, et al. Alcohol intoxication in road traffic accidents lead to higher impact speed difference, higher ISS and MAIS, and higher preclinical mortality. Alcohol. 2012;46:681–6.
Chen CM, Yi HY, Yoon YH, Dong C. Alcohol use at time of injury and survival following traumatic brain injury: result from National Trauma Data Bank. J Stud Alcohol Drug. 2012;73:531–41.
Rubin DB. Estimating causal effects from large data sets using propensity scores. Ann Intern Med. 1997;127(8pt2):757–63.
Hansen Ben B, Bowers Jake. Covariate balance in simple, stratified and clustered comparative studies. Stat Sci. 2008;23(2):219–36.
Bowers J, Fredrickson M, Hansen B (2016) RItools: Randomization Inference Tools. R package version 0.1–15.
Austin CP. The performance of different propensity-score methods for estimating differences in proportions (risk differences or absolute risk reductions) in observational studies. Statist Med. 2010;29:2137–48.
Austin CP. The performance of different propensity-score methods for estimating relative risks. J Clinic Epidem. 2008;61:537–45.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All procedures followed were in accordance with the ethical standards of the Institutional Review Board of Meridian Health and with the Helsinki Declaration of 1975, as revised in 2008. Since the study was done using a de-identified National database from the American College of Surgeons that is available to all researchers, this study was exempted from IRB review as per policy.
Conflict of interest
The authors (Nasim Ahmed and Patricia Greenberg) declare that they have no conflicts of interest.
Informed consent
Given that this study was done using a de-identified National database from the American College of Surgeons that is available to all researchers, this study was exempted from IRB review as per policy and no informed consent was required.
Rights and permissions
About this article
Cite this article
Ahmed, N., Greenberg, P. Patient mortality following alcohol use and trauma: a propensity-matched analysis. Eur J Trauma Emerg Surg 45, 151–158 (2019). https://doi.org/10.1007/s00068-017-0794-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-017-0794-6