Abstract
Purpose
Modern impartation of both anatomic and radiation oncology (RO) knowledge in medical education enables a transfer of preclinical knowledge to clinical practice, which may be addressed by multidisciplinary concepts. The faculty’s “Anatomy and imaging” course attempts to integrate RO, radiology and nuclear medicine into the preclinical curriculum. The present analysis focuses on the description of the course concept and discusses the potential didactic impact of the implementation of RO.
Methods
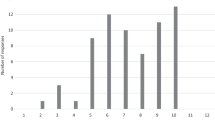
In total 5 semester cohorts have undertaken the course since the introduction of RO in the winter semester of 2015/2016 with 682 students participating. It is designed as a small group circuit training with a teaching content of 8 h daily. Course evaluation was performed on a 100-item Likert scale.
Results
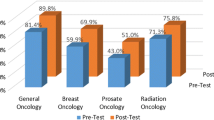
General evaluation showed an average of 9.3–12.7 on a Likert scale (0 being the best, 100 being the worst grade). Use of media, relevance for medical training, gain of interest in medicine in general and overall satisfaction with the course received excellent mean values. For RO, there was a high degree of consent with the following statements: “the course was well organized”, “subjects and presentation were well-structured”, “topics were well chosen”, “the time for exercises was sufficient” and “teaching by student tutors and physicians was adequate”.
Conclusion
The present evaluation demonstrates the feasibility of introducing RO in the preclinical part of medical education. The course concept shows excellent results in evaluation and may help in broadening RO knowledge and in recruiting new doctoral candidates and residents.
Zusammenfassung
Ziel
Die moderne Vermittlung von anatomischen und radioonkologischem (RO) Lehrinhalten schafft eine Verknüpfung von präklinischem und klinischem Wissen, was in Form interdisziplinärer Konzepte gelingen kann. Der Kurs „Anatomie und Bildgebung“ integriert RO, Radiologie und Nuklearmedizin in das präklinische Curriculum. Die vorliegende Analyse liefert eine Beschreibung des Kurskonzeptes und diskutiert die potentiellen didaktischen Auswirkungen der Implementierung der RO.
Methodik
Insgesamt durchliefen 5 Semesterkohorten mit 682 Studierenden den Kurs seit der Einführung der RO im Wintersemester 2015/2016. Der Kurs ist als Kleingruppenunterricht im Sinne eines Zirkeltrainings aufgebaut mit 8 Lehrmodulen täglich. Die Kursevaluation fand mittels einer 100-Punkt Likert-Skala statt.
Ergebnisse
Die Gesamtevaluation zeigte einen Durchschnittswert von 9,3–12,7 auf der Likert-Skala (0 als beste, 100 als schlechteste Note). Der Medieneinsatz, die Relevanz für die spätere ärztliche Tätigkeit, die Steigerung des Interesses am Studienfach Medizin sowie die Zufriedenheit mit dem Kurs wurden sehr gut bewertet. Für die RO bestand ein hoher Konsens mit den Aussagen: „Das Lehrmodul war gut organisiert“. „Lehrstoff und Präsentation waren gut strukturiert“. „Die Themen waren gut ausgewählt“. „Die Übungszeit war ausreichend“. „Die Vermittlung durch studentische Tutoren und Ärzte war adäquat“.
Schlussfolgerung
Die vorliegende Auswertung zeigt die Möglichkeit auf, die RO in die präklinische Lehre zu integrieren. Das Konzept weist exzellente Evaluationsergebnisse auf und kann dazu beitragen RO Wissen zu vermitteln und potentielle neue Doktoranden und Assistenzärztinnen und -ärzte zu rekrutieren.

Similar content being viewed by others
References
Robert Koch-Institut (2017) Krebs in Deutschland für 2013/2014 https://doi.org/10.17886/rkipubl-2017-007
Cronin KA, Lake AJ, Scott S et al (2018) Annual Report to the Nation on the Status of Cancer, part I: National cancer statistics: Annual Report National Cancer Statistics. Cancer 124:2785–2800. https://doi.org/10.1002/cncr.31551
Kim YS, Kim JW, Yoon WS et al (2016) Interobserver variability in gross tumor volume delineation for hepatocellular carcinoma: Results of Korean Radiation Oncology Group 1207 study. Strahlenther Onkol 192:714–721. https://doi.org/10.1007/s00066-016-1028-2
Schimek-Jasch T, Troost EGC, Rücker G et al (2015) A teaching intervention in a contouring dummy run improved target volume delineation in locally advanced non-small cell lung cancer: Reducing the interobserver variability in multicentre clinical studies. Strahlenther Onkol 191:525–533. https://doi.org/10.1007/s00066-015-0812-8
Spoelstra FO, Senan S, Le Péchoux C et al (2010) Variations in target volume definition for postoperative radiotherapy in stage III non-small-cell lung cancer: Analysis of an international contouring study. Int J Radiat Oncol Biol Phys 76:1106–1113. https://doi.org/10.1016/j.ijrobp.2009.02.072
Dietzel CT, Jablonska K, Niyazi M et al (2018) Quality of training in radiation oncology in Germany: Where do we stand? Strahlenther Onkol 194:293–302. https://doi.org/10.1007/s00066-017-1250-6
Dettmer S, Tschernig T, Galanski M et al (2010) Teaching surgery, radiology and anatomy together: The mix enhances motivation and comprehension. Surg Radiol Anat 32:791–795. https://doi.org/10.1007/s00276-010-0694-5
Dettmer S, Schmiedl A, Meyer S et al (2013) Radiological anatomy—Evaluation of integrative education in radiology. Rofo 185:838–843. https://doi.org/10.1055/s-0033-1335048
Rengier F, Doll S, von Tengg-Kobligk H et al (2009) Integrated teaching of anatomy and radiology using three-dimensional image post-processing. Eur Radiol 19:2870–2877. https://doi.org/10.1007/s00330-009-1507-2
Schober A, Pieper C, Schmidt R, Wittkowski W (2013) “Anatomy and Imaging”: 10 years of experience with an interdisciplinary teaching project in preclinical medical education—From an elective to a curricular course. Rofo 186:458–465. https://doi.org/10.1055/s-0033-1355567
Schober A, Schmitz M, Zimmer S, Schmidt R, Oertel M, Vrachimis A, Marschall B (2017) Vom Know-what zum Know-how – 15 Jahre „Anatomie und Bildgebung“. Joint Congress of the Gesellschaft für Medizinische Ausbildung (GMA) and the Arbeitskreis zur Weiterentwicklung der Lehre in der Zahnmedizin (AKWLZ), Münster, 20.–23.09.2017
Zumwalt AC, Marks L, Halperin EC (2007) Integrating gross anatomy into a clinical oncology curriculum: The oncoanatomy course at Duke University School of Medicine. Acad Med 82(5):469–474. https://doi.org/10.1097/ACM.0b013e31803ea96a
Zaorsky NG, Shaikh T, Handorf E et al (2016) What are medical students in the United States learning about radiation oncology? Results of a multi-institutional survey. Int J Radiat Oncol Biol Phys 94(2):235–242. https://doi.org/10.1016/j.ijrobp.2015.10.008
Brower JV, Mohindra P, Bradley KA, Golden DW (2014) Radiation oncology residency selection: A targeted assessment of factor importance among fourth-year medical students. Int J Radiat Oncol Biol Phys 88:967–968. https://doi.org/10.1016/j.ijrobp.2013.12.020
Dennis KEB, Duncan G (2010) Radiation oncology in undergraduate medical education: A literature review. Int J Radiat Oncol Biol Phys 76(3):649–655. https://doi.org/10.1016/j.ijrobp.2009.08.038
Agarwal A, Koottappillil B, Shah B et al (2015) Medical student—Reported outcomes of a radiation oncologist—Led preclinical course in oncology: A five-year analysis. Int J Radiat Oncol Biol Phys 92(4):735–739. https://doi.org/10.1016/j.ijrobp.2015.03.008
Agarwal A, Shah A, Shah B et al (2017) The impact of a radiation oncologist led oncology curriculum on medical student knowledge. J Cancer Educ. https://doi.org/10.1007/s13187-017-1227-2
Golden DW, Kauffmann GE, McKillip RP et al (2018) Objective evaluation of a didactic curriculum for the radiation oncology medical student clerkship. Int J Radiat Oncol Biol Phys 101:1039–1045. https://doi.org/10.1016/j.ijrobp.2018.04.052
Carraccio CL, Englander R (2013) From Flexner to competencies: Reflections on a decade and the journey ahead. Acad Med 88:1067–1073. https://doi.org/10.1097/ACM.0b013e318299396f
Desy JR, Reed DA, Wolanskyj AP (2017) Milestones and millennials: A perfect pairing-competency-based medical education and the learning preferences of Generation Y. Mayo Clin Proc 92:243–250. https://doi.org/10.1016/j.mayocp.2016.10.026
Bundesministerium für Bildung und Forschung (2017) Masterplan Medizinstudium 2020
Jünger J (2018) Competence-based assessment in the national licensing examination in Germany. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz 61:171–177. https://doi.org/10.1007/s00103-017-2668-9
Akademie der DEGRO (2016) Curriculum zur Weiterbildung zum „Facharzt für Strahlentherapie“ der Akademie der „Deutschen Gesellschaft fur Radioonkologie’(DEGRO) zur ’Fort- und Weiterbildung in der Radioonkologie“
Ertl-Wagner B, Barkhausen J, Mahnken AH et al (2016) White paper: Radiological curriculum for undergraduate medical education in Germany. Rofo 188:1017–1023. https://doi.org/10.1055/s-0042-116026
Marienhagen J, Brenner W, Buck A et al (2018) Development of a national competency-based learning objective catalogue for undergraduate medical education in Germany. Nuklearmedizin 57(04):137–145. https://doi.org/10.3413/Nukmed-0969-18-03
MFT Medizinischer Fakultätentag der Bundesrepublik Deutschland e. V. (2015) Nationaler Kompetenzbasierter Lernzielkatalog Medizin (NKLM)
Matthes J, Marxen B, Linke R‑M et al (2002) The influence of tutor qualification on the process and outcome of learning in a problem-based course of basic medical pharmacology. Naunyn Schmiedebergs Arch Pharmacol 366:58–63. https://doi.org/10.1007/s00210-002-0551-0
Krug D, Baumann R, Rieckmann T et al (2016) Situation of young radiation oncologists, medical physicists and radiation biologists in German-speaking countries: Results from a web-based survey of the Young DEGRO working group. Strahlenther Onkol 192:507–515. https://doi.org/10.1007/s00066-016-1003-y
Evans DJ, Watt DJ (2005) Provision of anatomical teaching in a new British medical school: Getting the right mix. Anat Rec B New Anat 284:22–27. https://doi.org/10.1002/ar.b.20065
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
M. Oertel, M. Schmitz, J.C. Becker, H.T. Eich and A. Schober declare that they have no competing interests.
Rights and permissions
About this article
Cite this article
Oertel, M., Schmitz, M., Becker, J.C. et al. Successful integration of radiation oncology in preclinical medical education. Strahlenther Onkol 195, 1104–1109 (2019). https://doi.org/10.1007/s00066-019-01492-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00066-019-01492-z