Abstract
Aim
To assess the role of perilesional edema (PE) in non-small cell lung carcinoma (NSCLC) brain metastases (BM) undergoing radiosurgery (SRS).
Methods
This series includes 46 patients with 1–2 BM treated with SRS, selected out of all patients referred for radiotherapy (RT) for BMs over 5 years (2013 to 2017). Both the PE and gross tumor volume (GTV) were contoured on MRI images, and the PE/GTV ratio and PE + GTV value (TV, total volume) were calculated. Our clinical endpoints were brain recurrence free-survival, divided into local brain control (in field, LBC) and distant brain control (out of field, DBC) and overall survival (OS). We analyzed the role of the previously described volumetric parameters and of known clinical prognosticators (disease specific GPA, DS-GPA; chemotherapy, CHT) with Cox regression analyses.
Results
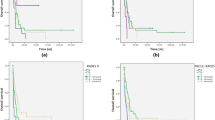
Only four patients (9%) developed in-field progression, whereas 10 patients (22%) showed new out-of-field BM and thirty-eight patients died in the follow up (83%). In univariate analysis, both volumetric parameters and clinical parameters were correlated with DBC and OS, whereas we did not find any correlation with LBC. In the multivariate analysis of DBC, the significant parameters were PE/GTV ratio (HR 0.302), sex (HR 0.131), and DS-GPA (HR 0.261). The OS multivariate analysis showed that the only significant parameters were DS-GPA (HR 0.478) and TV (HR: 1.038).
Conclusion
Our study, although with the limitations of a monocentric retrospective study analyzing a small cohort of patients, suggests the role of PE/GTV ratio for the development of new BMs. TV also seems to be correlated with OS, together with known clinical prognosticators. These findings, if validated in a larger prospective dataset, could help in selecting patients for the most suitable RT modality (or systemic therapy approach).
Zusammenfassung
Ziel
Beurteilung der Rolle des perilesionalen Ödems (PE) bei der Radiochirurgie (SRS) von Hirnmetastasen (BM) beim nicht-kleinzelligen Lungenkarzinom (NSCLC).
Methoden
Diese Serie umfasst 46 Patienten mit 1–2 mit SRS behandelten BM, die aus allen Patienten ausgewählt wurden, bei denen über einen Zeitraum von 5 Jahren (2013–2017) eine Radiotherapie (RT) zur BM-Behandlung eingesetzt wurde. Sowohl das PE- als auch das Bruttovolumen des Tumors (GTV) wurde auf MRT-Bildern konturiert, um das PE/GTV-Verhältnis und den PE + GTV-Wert (TV, Gesamtvolumen) zu erhalten. Unsere klinischen Endpunkte waren die rezidivfreie Zeit des Gehirns, welche in die lokale Hirnkontrolle (LBC, „in field“) und die entfernte Hirnkontrolle (DBC, „out of field“) unterteilt wurde, sowie das Gesamtüberleben des Patienten (OS). Wir haben die Rolle der zuvor beschriebenen volumetrischen Parameter und der bekannten klinischen Faktoren (krankheitsspezifische GPA: DS-GPA, Chemotherapie: CHT) mit den Cox-Regressionsanalysen analysiert.
Ergebnisse
Nur 4 Patienten (9%) entwickelten eine In-field-Progression, wohingegen 10 Patienten (22%) neue Out-of-field-BM zeigten und 38 Patienten im Follow-up starben (83%). Bei der univariaten Analyse wurden sowohl die volumetrischen Parameter als auch die klinischen Parameter mit DBC und OS korreliert, wohingegen wir keine Korrelation mit LBC fanden. Bei der multivariaten DBC-Analyse waren das PE/GTV-Verhältnis (HR 0,302), das Geschlecht des Patienten (HR 0,131) und das DS-GPA (HR 0,261) signifikante Parameter.
Schlussfolgerung
Unsere Studie legt – trotz der Einschränkungen einer monozentrischen retrospektiven Studie, die eine kleine Patientengruppe analysiert – die Rolle des PE/GTV-Verhältnisses für die Entwicklung neuer BMs nahe. Das TV scheint auch mit OS, zusammen mit bekannten klinischen Faktoren, zu korrelieren. Diese Erkenntnisse könnten, wenn sie in einem größeren, prospektiven Datensatz validiert würden, bei der Auswahl der Patienten für die geeignetste RT-Modalität (oder den systemischen Therapieansatz) helfen.




Similar content being viewed by others
References
Sawaya RBR, Lang FF et al (2001) Metastatic brain tumors. In: Kaye EL (ed) Brain tumors, 2nd edn. An encyclopedic approach. Churchill Livingstone, London, UK, pp 999–1026
Peters S, Camidge DR, Shaw AT, Gadgeel S, Ahn JS, Kim DW, Ou SI, Perol M, Dziadziuszko R, Rosell R et al (2017) Alectinib versus Crizotinib in untreated ALK-positive non-small-cell lung cancer. N Engl J Med 377(9):829–838
Levy A, Faivre-Finn C, Hasan B, De Maio E, Berghoff AS, Girard N, Greillier L, Lantuejoul S, O’Brien M, Reck M et al (2018) Diversity of brain metastases screening and management in non-small cell lung cancer in Europe: Results of the European Organisation for Research and Treatment of Cancer Lung Cancer Group survey. Eur J Cancer 93:37–46
Lukas RV, Lesniak MS, Salgia R (2014) Brain metastases in non-small-cell lung cancer: better outcomes through current therapies and utilization of molecularly targeted approaches. CNS Oncol 3(1):61–75
Franchino F, Rudà R, Soffietti R (2018) Mechanisms and therapy for cancer metastasis to the brain. Front Oncol 8:161
Soffietti R, Abacioglu U, Baumert B, Combs SE, Kinhult S, Kros JM, Marosi C, Metellus P, Radbruch A, Villa Freixa SS et al (2017) Diagnosis and treatment of brain metastases from solid tumors: guidelines from the European Association of Neuro-Oncology (EANO). Neuro-oncology 19(2):162–174
Hunter GK, Suh JH, Reuther AM, Vogelbaum MA, Barnett GH, Angelov L, Weil RJ, Neyman G, Chao ST (2012) Treatment of five or more brain metastases with stereotactic radiosurgery. Int J Radiat Oncol Biol Phys 83(5):1394–1398
Raldow AC, Chiang VL, Knisely JP, Yu JB (2013) Survival and intracranial control of patients with 5 or more brain metastases treated with gamma knife stereotactic radiosurgery. Am J Clin Oncol 36(5):486–490
Loganadane G, Hendriks L, Le Pechoux C, Levy A (2017) The current role of whole brain radiation therapy in non-small cell lung cancer patients. J Thorac Oncol 12(10):1467–1477
Yang JJ, Zhou C, Huang Y, Feng J, Lu S, Song Y, Huang C, Wu G, Zhang L, Cheng Y et al (2017) Icotinib versus whole-brain irradiation in patients with EGFR-mutant non-small-cell lung cancer and multiple brain metastases (BRAIN): a multicentre, phase 3, open-label, parallel, randomised controlled trial. Lancet Respir Med 5(9):707–716
Mulvenna P, Nankivell M, Barton R, Faivre-Finn C, Wilson P, McColl E, Moore B, Brisbane I, Ardron D, Holt T et al (2016) Dexamethasone and supportive care with or without whole brain radiotherapy in treating patients with non-small cell lung cancer with brain metastases unsuitable for resection or stereotactic radiotherapy (QUARTZ): results from a phase 3, non-inferiority, randomised trial. Lancet 388(10055):2004–2014
Reginelli A, Silvestro G, Fontanella G, Sangiovanni A, Conte M, Nuzzo I, Di Lecce A, Martino A, Grassi R, Murino P et al (2016) Performance status versus anatomical recovery in metastatic disease: the role of palliative radiation treatment. Int J Surg 33(Suppl 1):126–131
Nieder C, Hintz M, Oehlke O, Bilger A, Grosu AL (2017) Validation of the graded prognostic assessment for lung cancer with brain metastases using molecular markers (lung-molGPA). Radiat Oncol 12:107
Miyazawa K, Shikama N, Okazaki S, Koyama T, Takahashi T, Kato S (2018) Predicting prognosis of short survival time after palliative whole-brain radiotherapy. J Radiat Res 59(1):43–49
Partl R, Fastner G, Kaiser J, Kronhuber E, Cetin-Strohmer K, Steffal C, Bohmer-Breitfelder B, Mayer J, Avian A, Berghold A (2016) KPS/LDH index: a simple tool for identifying patients with metastatic melanoma who are unlikely to benefit from palliative whole brain radiotherapy. Support Care Cancer 24(2):523–528
Pietrantonio F, Aprile G, Rimassa L, Franco P, Lonardi S, Cremolini C, Biondani P, Sbicego EL, Pasqualetti F, Tomasello G et al (2015) A new nomogram for estimating survival in patients with brain metastases secondary to colorectal cancer. Radiother Oncol 117(2):315–321
Ashworth AB, Senan S, Palma DA, Riquet M, Ahn YC, Ricardi U, Congedo MT, Gomez DR, Wright GM, Melloni G et al (2014) An individual patient data metaanalysis of outcomes and prognostic factors after treatment of oligometastatic non-small-cell lung cancer. Clin Lung Cancer 15(5):346–355
Sperduto PW, Wang M, Robins HI, Schell MC, Werner-Wasik M, Komaki R, Souhami L, Buyyounouski MK, Khuntia D, Demas W et al (2013) A phase 3 trial of whole brain radiation therapy and stereotactic radiosurgery alone versus WBRT and SRS with temozolomide or erlotinib for non-small cell lung cancer and 1 to 3 brain metastases: Radiation Therapy Oncology Group 0320. Int J Radiat Oncol Biol Phys 85(5):1312–1318
Lin NU, Lee EQ, Aoyama H, Barani IJ, Barboriak DP, Baumert BG, Bendszus M, Brown PD, Camidge DR, Chang SM et al (2015) Response assessment criteria for brain metastases: proposal from the RANO group. Lancet Oncol 16(6):e270–e278
Tini P, Nardone V, Pastina P, Pirtoli L, Correale P, Giordano A (2018) The effects of radiotherapy on the survival of patients with unresectable non-small cell lung cancer. Expert Rev Anticancer Ther 18(6):593–602. https://doi.org/10.1080/14737140.2018.1458615
Kocher M, Soffietti R, Abacioglu U, Villa S, Fauchon F, Baumert BG, Fariselli L, Tzuk-Shina T, Kortmann RD, Carrie C et al (2011) Adjuvant whole-brain radiotherapy versus observation after radiosurgery or surgical resection of one to three cerebral metastases: results of the EORTC 22952-26001 study. J Clin Oncol 29(2):134–141
Aoyama H, Shirato H, Tago M, Nakagawa K, Toyoda T, Hatano K, Kenjyo M, Oya N, Hirota S, Shioura H et al (2006) Stereotactic radiosurgery plus whole-brain radiation therapy vs stereotactic radiosurgery alone for treatment of brain metastases: a randomized controlled trial. JAMA 295(21):2483–2491
Chang EL, Wefel JS, Hess KR, Allen PK, Lang FF, Kornguth DG, Arbuckle RB, Swint JM, Shiu AS, Maor MH et al (2009) Neurocognition in patients with brain metastases treated with radiosurgery or radiosurgery plus whole-brain irradiation: a randomised controlled trial. Lancet Oncol 10(11):1037–1044
Brown PD, Jaeckle K, Ballman KV, Farace E, Cerhan JH, Anderson SK, Carrero XW, Barker FG 2nd, Deming R, Burri SH et al (2016) Effect of Radiosurgery alone vs Radiosurgery with whole brain radiation therapy on cognitive function in patients with 1 to 3 brain metastases: a randomized clinical trial. JAMA 316(4):401–409
Robin TP, Rusthoven CG (2018) Strategies to preserve cognition in patients with brain metastases: a review. Front Oncol 8:415
Brown PD, Ahluwalia MS, Khan OH, Asher AL, Wefel JS, Gondi V (2018) Whole-brain radiotherapy for brain metastases: evolution or revolution? J Clin Oncol 36(5):483–491
Sperduto PW, Chao ST, Sneed PK, Luo X, Suh J, Roberge D, Bhatt A, Jensen AW, Brown PD, Shih H et al (2010) Diagnosis-specific prognostic factors, indexes, and treatment outcomes for patients with newly diagnosed brain metastases: a multi-institutional analysis of 4,259 patients. Int J Radiat Oncol Biol Phys 77(3):655–661
Golden DW, Lamborn KR, McDermott MW, Kunwar S, Wara WM, Nakamura JL, Sneed PK (2008) Prognostic factors and grading systems for overall survival in patients treated with radiosurgery for brain metastases: variation by primary site. J Neurosurg 109(Suppl):77–86
Rades D, Dziggel L, Haatanen T, Veninga T, Lohynska R, Dunst J, Schild SE (2011) Scoring systems to estimate intracerebral control and survival rates of patients irradiated for brain metastases. Int J Radiat Oncol Biol Phys 80(4):1122–1127
Rodrigues G, Bauman G, Palma D, Louie AV, Mocanu J, Senan S, Lagerwaard F (2013) Systematic review of brain metastases prognostic indices. Pract Radiat Oncol 3(2):101–106
Wang X, Xu Y, Tang W, Liu L (2018) Efficacy and safety of radiotherapy plus EGFR-TKis in NSCLC patients with brain metastases: a meta-analysis of published data. Transl Oncol 11(5):1119–1127
Shumakovich MA, Mencio CP, Siglin JS, Moriarty RA, Geller HM, Stroka KM (2017) Astrocytes from the brain microenvironment alter migration and morphology of metastatic breast cancer cells. FASEB J. https://doi.org/10.1096/fj.201700254R
Priego N, Zhu L, Monteiro C, Mulders M, Wasilewski D, Bindeman W, Doglio L, Martinez L, Martinez-Saez E, Cajal SRY et al (2018) STAT3 labels a subpopulation of reactive astrocytes required for brain metastasis. Nat Med 24(7):1024–1035
Zakaria R, Das K, Bhojak M, Radon M, Walker C, Jenkinson MD (2014) The role of magnetic resonance imaging in the management of brain metastases: diagnosis to prognosis. Cancer Imaging 14:8
Venur VA, Ahluwalia MS (2015) Prognostic scores for brain metastasis patients: use in clinical practice and trial design. Chin Clin Oncol 4(2):18
Reginelli A, Silvestro G, Fontanella G, Sangiovanni A, Conte M, Nuzzo I, Calvanese M, Traettino M, Ferraioli P, Grassi R et al (2016) Validation of DWI in assessment of radiotreated bone metastases in elderly patients. Int J Surg 33(Suppl 1):148–153
Nardone V, Pastina P, Giannicola R, Agostino R, Croci S, Tini P, Pirtoli L, Giordano A, Tagliaferri P, Correale P (2018) How to increase the efficacy of immunotherapy in NSCLC and HNSCC: role of radiation therapy, chemotherapy, and other strategies. Front Immunol. https://doi.org/10.3389/fimmu.2018.02941
Papadopoulos MC, Saadoun S, Binder DK, Manley GT, Krishna S, Verkman AS (2004) Molecular mechanisms of brain tumor edema. Neuroscience 129(4):1009–1018
Papadopoulos MC, Saadoun S, Woodrow CJ, Davies DC, Costa-Martins P, Moss RF, Krishna S, Bell BA (2001) Occludin expression in microvessels of neoplastic and non-neoplastic human brain. Neuropathol Appl Neurobiol 27(5):384–395
Roitbak T, Sykova E (1999) Diffusion barriers evoked in the rat cortex by reactive astrogliosis. Glia 28(1):40–48
Berghoff AS, Fuchs E, Ricken G, Mlecnik B, Bindea G, Spanberger T, Hackl M, Widhalm G, Dieckmann K, Prayer D et al (2016) Density of tumor-infiltrating lymphocytes correlates with extent of brain edema and overall survival time in patients with brain metastases. Oncoimmunology 5(1):e1057388
Tini P, Nardone V, Pastina P, Battaglia G, Vinciguerra C, Carfagno T, Rubino G, Carbone SF, Sebaste L, Cerase A et al (2017) Perilesional edema in brain metastasis from non-small cell lung cancer (NSCLC) as predictor of response to radiosurgery (SRS). Ital J Neurol Sci 38(6):975–982
Nardone V, Vinciguerra C, Federico A, Cerase A, Pirtoli L, Tini P (2018) Perilesional edema in brain cancer: Independent prognosticator or epiphenomenon of biomolecular signature? Radiother Oncol 129(1):183–184. https://doi.org/10.1016/j.radonc.2017.12.020
Schoenegger K, Oberndorfer S, Wuschitz B, Struhal W, Hainfellner J, Prayer D, Heinzl H, Lahrmann H, Marosi C, Grisold W (2009) Peritumoral edema on MRI at initial diagnosis: an independent prognostic factor for glioblastoma? Eur J Neurol 16(7):874–878
Buttigliero C, Bertaglia V, Novello S (2016) Anti-angiogenetic therapies for central nervous system metastases from non-small cell lung cancer. Transl Lung Cancer Res 5(6):610–627
Ludwig HC, Ahkavan-Shigari R, Rausch S, Schallock K, Quentin C, Ziegler D, Bockermann V, Markakis E (2000) Oedema extension in cerebral metastasis and correlation with the expression of nitric oxide synthase isozymes (NOS I–III). Anticancer Res 20(1a):305–310
Spanberger T, Berghoff AS, Dinhof C, Ilhan-Mutlu A, Magerle M, Hutterer M, Pichler J, Wohrer A, Hackl M, Widhalm G et al (2013) Extent of peritumoral brain edema correlates with prognosis, tumoral growth pattern, HIF1a expression and angiogenic activity in patients with single brain metastases. Clin Exp Metastasis 30(4):357–368
Berghoff AS, Ilhan-Mutlu A, Wohrer A, Hackl M, Widhalm G, Hainfellner JA, Dieckmann K, Melchardt T, Dome B, Heinzl H et al (2014) Prognostic significance of Ki67 proliferation index, HIF1 alpha index and microvascular density in patients with non-small cell lung cancer brain metastases. Strahlenther Onkol 190(7):676–685
Hanahan D, Weinberg RA (2011) Hallmarks of cancer: the next generation. Cell 144(5):646–674
Shaverdian N, Wang J, Levin-Epstein R, Schaue D, Kupelian P, Lee P, Yang I, Kaprealian T (2016) Pro-inflammatory state portends poor outcomes with Stereotactic Radiosurgery for brain metastases. Anticancer Res 36(10):5333–5337
Mostofa AG, Punganuru SR, Madala HR, Al-Obaide M, Srivenugopal KS (2017) The process and regulatory components of inflammation in brain Oncogenesis. Biomolecules. https://doi.org/10.3390/biom7020034
Bhatnagar AK, Flickinger JC, Kondziolka D, Lunsford LD (2006) Stereotactic radiosurgery for four or more intracranial metastases. Int J Radiat Oncol Biol Phys 64(3):898–903
Likhacheva A, Pinnix CC, Parikh NR, Allen PK, McAleer MF, Chiu MS, Sulman EP, Mahajan A, Guha-Thakurta N, Prabhu SS et al (2013) Predictors of survival in contemporary practice after initial Radiosurgery for brain metastases. Int J Radiat Oncol Biol Phys 85(3):656–661
Baschnagel AM, Meyer KD, Chen PY, Krauss DJ, Olson RE, Pieper DR, Maitz AH, Ye H, Grills IS (2013) Tumor volume as a predictor of survival and local control in patients with brain metastases treated with Gamma Knife surgery. J Neurosurg 119(5):1139–1144
Routman DM, Bian SX, Diao K (2018) The growing importance of lesion volume as a prognostic factor in patients with multiple brain metastases treated with stereotactic radiosurgery. Cancer Med 7(3):757–764
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
V. Nardone, S. Nanni, P. Pastina, C. Vinciguerra, A. Cerase, P. Correale, C. Guida, A. Giordano, P. Tini, A. Reginelli, S. Cappabianca, and L. Pirtoli declare that they have no competing interests.
Rights and permissions
About this article
Cite this article
Nardone, V., Nanni, S., Pastina, P. et al. Role of perilesional edema and tumor volume in the prognosis of non-small cell lung cancer (NSCLC) undergoing radiosurgery (SRS) for brain metastases. Strahlenther Onkol 195, 734–744 (2019). https://doi.org/10.1007/s00066-019-01475-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00066-019-01475-0