Abstract
Background and Purpose
Subpial hemorrhage is a rare form of neonatal stroke, still poorly understood. The aim of this study was to characterize a cohort of term and preterm neonates with subpial hemorrhages and contribute to a better knowledge of this condition.
Material and Methods
Clinical records and magnetic resonance (MR) imaging data of all neonates with subpial hemorrhage followed at a pediatric hospital between 2010 and 2020 were retrospectively reviewed.
Results
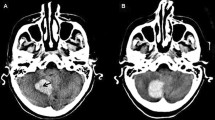
A total of 10 patients were included in the analysis, 40% of whom were term neonates. Operative vaginal delivery was registered in 30%. Temporal was the most common location of subpial hemorrhage (70%), and all patients displayed underlying brain infarction. A characteristic yin-yang pattern was present in 90% of the study cohort, and ingurgitation of medullary veins on susceptibility weighted imaging in 80%. Cerebellar microbleeds were observed in 60% of neonates, both term and preterm. When available, MR angiography and venography were unremarkable. Patients’ clinical outcome was variable, with early prematurity not associated to worse outcomes.
Conclusion
Subpial hemorrhage has a distinctive MR pattern, with underlying parenchymal venous infarction, and can occur in term and preterm neonates. This study results suggest an association between subpial hemorrhage and cerebellar microbleeds but further studies are required to confirm it and better understand the pathophysiology of subpial hemorrhage.







Similar content being viewed by others
References
Dunbar M, Kirton A. Perinatal stroke: mechanisms, management, and outcomes of early cerebrovascular brain injury. Lancet Child Adolesc Health. 2018;2:666–76.
Friede RL. Subpial hemorrhage in infants. J Neuropathol Exp Neurol. 1972;31:548–56.
Huang AH, Robertson RL. Spontaneous superficial parenchymal and leptomeningeal hemorrhage in term neonates. AJNR Am J Neuroradiol. 2004;25:469–75. Erratum in: AJNR Am J Neuroradiol. 2004;35:666.
Lee S, Mirsky DM, Beslow LA, Amlie-Lefond C, Danehy AR, Lehman L, Stence NV, Vossough A, Wintermark M, Rivkin MJ; International Paediatric Stroke Study Neuroimaging Consortium and the Paediatric Stroke Neuroimaging Consortium. Pathways for Neuroimaging of Neonatal Stroke. Pediatr Neurol. 2017;69:37–48.
Cain DW, Dingman AL, Armstrong J, Stence NV, Jensen AM, Mirsky DM. Subpial Hemorrhage of the Neonate. Stroke. 2020;51:315–8.
Assis Z, Kirton A, Pauranik A, Sherriff M, Wei XC. Idiopathic Neonatal Subpial Hemorrhage with Underlying Cerebral Infarct: Imaging Features and Clinical Outcome. AJNR Am J Neuroradiol. 2021;42:185–93.
Cole L, Dewey D, Letourneau N, Kaplan BJ, Chaput K, Gallagher C, Hodge J, Floer A, Kirton A. Clinical Characteristics, Risk Factors, and Outcomes Associated With Neonatal Hemorrhagic Stroke: A Population-Based Case-Control Study. JAMA Pediatr. 2017;171:230–8. Erratum in: JAMA Pediatr. 2017;171:602.
Bergman I, Bauer RE, Barmada MA, Latchaw RE, Taylor HG, David R, Painter MJ. Intracerebral hemorrhage in the full-term neonatal infant. Pediatrics. 1985;75:488–96.
Hanigan WC, Powell FC, Palagallo G, Miller TC. Lobar hemorrhages in full-term neonates. Childs Nerv Syst. 1995;11:276–80.
Slaughter L, Egelhoff J, Balmakund T. Neurologic outcome in neonatal temporal lobe hemorrhagic venous infarcts. J Child Neurol. 2009;24:1236–42.
Bruno CJ, Beslow LA, Witmer CM, Vossough A, Jordan LC, Zelonis S, Licht DJ, Ichord RN, Smith SE. Haemorrhagic stroke in term and late preterm neonates. Arch Dis Child Fetal Neonatal Ed. 2014;99:F48–53.
Kersbergen KJ, Groenendaal F, Benders MJ, de Vries LS. Neonatal cerebral sinovenous thrombosis: neuroimaging and long-term follow-up. J Child Neurol. 2011;26:1111–20.
Khalatbari H, Wright JN, Ishak GE, Perez FA, Amlie-Lefond CM, Shaw DWW. Deep medullary vein engorgement and superficial medullary vein engorgement: two patterns of perinatal venous stroke. Pediatr Radiol. 2021;51:675–85.
Barreto ARF, Carrasco M, Dabrowski AK, Sun LR, Tekes A. Subpial Hemorrhage in Neonates: What Radiologists Need to Know. AJR Am J Roentgenol. 2021;216:1056–65.
Villamor-Martinez E, Fumagalli M, Alomar YI, Passera S, Cavallaro G, Mosca F, Villamor E. Cerebellar Hemorrhage in Preterm Infants: A Meta-Analysis on Risk Factors and Neurodevelopmental Outcome. Front Physiol. 2019;10:800.
Limperopoulos C, du Plessis AJ. Disorders of cerebellar growth and development. Curr Opin Pediatr. 2006;18:621–7.
Johnsen SD, Tarby TJ, Lewis KS, Bird R, Prenger E. Cerebellar infarction: an unrecognized complication of very low birthweight. J Child Neurol. 2002;17:320–4.
Limperopoulos C, Benson CB, Bassan H, Disalvo DN, Kinnamon DD, Moore M, Ringer SA, Volpe JJ, du Plessis AJ. Cerebellar hemorrhage in the preterm infant: ultrasonographic findings and risk factors. Pediatrics. 2005;116:717–24.
Volpe JJ. Cerebellum of the premature infant: rapidly developing, vulnerable, clinically important. J Child Neurol. 2009;24:1085–104.
Funding
No funds, grants, or other support were received.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
C. Pinto, B. Cunha, M.M. Pinto and C. Conceição declare that they have no competing interests.
Ethical standards
This retrospective study was performed after consultation with the institutional ethics committee and in accordance with national legal requirements. This study was approved by local Ethics Committee. Consent to participate: Informed consent was waived. Consent for publication: Informed consent was waived.
Additional information
Availability of Data and Material
All data are available on request.
Code Availability
Not applicable.
Rights and permissions
About this article
Cite this article
Pinto, C., Cunha, B., Pinto, M.M. et al. Subpial Hemorrhage. Clin Neuroradiol 32, 1057–1065 (2022). https://doi.org/10.1007/s00062-022-01149-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00062-022-01149-y