Abstract
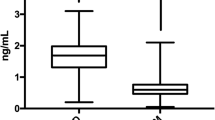
Platelet-derived microparticles (PDMP), selectins, and adiponectin play an important role in the development of atherosclerosis in diabetes. Acarbose has been shown to have a beneficial effect on postprandial hyperglycemia in diabetic patients. However, its influence on PDMP, selectins, and adiponectin in these patients is poorly understood. We investigated the effect of acarbose on circulating levels of PDMP, selectins, and adiponectin in patients with type 2 diabetes. Acarbose (300 mg/day) was administered for 3 months. Levels of PDMP, sP-selectin, sL-selectin, and adiponectin were measured by ELISA at baseline and after 1 and 3 months of treatment. The levels of PDMP, sP-selectin, and sL-selectin were higher in diabetic patients than in hypertensive patients (PDMP; 35.1 ± 34.2 vs. 53.3 ± 56.7 U/ml, P < 0.05: sP-selectin; 134 ± 52 vs. 235 ± 70 ng/dl, P < 0.01: sL-selectin; 569 ± 183 vs. 805 ± 146 ng/ml, P < 0.05), while there were no significant differences between hypertensive and hyperlipidemic patients. Before acarbose treatment, the adiponectin level of diabetic patients was lower than that of hypertensive patients. Acarbose therapy significantly decreased the plasma PDMP level relative to baseline. Acarbose also caused a significant decrease of sP-selectin and sL-selectin. On the other hand, acarbose therapy led to a significant increase of adiponectin after 3 months of administration compared with baseline (adiponectin: diabetes versus hypertension, 3.61 ± 1.23 vs. 5.87 ± 1.92 μg/ml, P < 0.05; diabetes versus controls, 2.81 ± 0.95 vs. 6.13 ± 1.24 μg/ml, P < 0.01). Twelve of the 30 diabetic patients had a history of thrombotic complications. Furthermore, the reduction of PDMP and selectins during acarbose therapy was significantly greater in the thrombotic group (12 of 30) than in the nonthrombotic group (18 of 30) of diabetic patients. Acarbose may be beneficial for primary prevention of atherothrombosis in patients with type 2 diabetes. However, it requires a large clinical trial to test this hypothesis.



Similar content being viewed by others
References
Chobanian AV (1991) Single risk factor intervention may be inadequate to inhibit atherosclerosis progression when hypertension and hypercholesterolemia co-exist. Hypertension 18:130–131
Schafer AI (1985) The hypercoagulable states. Ann Intern Med 102:814–818
Frade LJG, de la Calle H, Alava I et al (1987) Diabetes as a hypercoagulable state: its relationship with fibrin fragments and vascular damage. Thromb Res 47:533–540. doi:10.1016/0049-3848(87)90358-6
Nomura S (2001) Function and clinical significance of platelet-derived microparticles. Int J Hematol 74:397–404. doi:10.1007/BF02982082
Nomura S, Ozaki Y, Ikeda Y (2008) Function and role of microparticles in various clinical settings. Thromb Res 123:8–23. doi:10.1016/j.thromres.2008.06.006
Cominacini L, Pasini AF, Garbin U et al (1995) Elevated levels of soluble E-selectin in patients with IDDM and NIDDM: relation to metabolic control. Diabetologia 38:1122–1124. doi:10.1007/BF00402185
Lim YC, Snapp K, Kansas GS et al (1998) Important contributions of P-selectin glycoprotein ligand-1-mediated secondary capture to human monocyte adhesion to P-selectin, E-selectin, and TNF-α-activated endothelium under flow in vitro. J Immunol 161:2501–2508
Tschope D, Esser J, Schwippert B et al (1991) Large platelets circulate in an activated state in diabetes. Semin Thromb Hemost 17:433–439. doi:10.1055/s-2007-1002650
Nomura S, Shouzu A, Omoto S et al (2000) Significance of chemokines and activated platelets in patients with diabetes. Clin Exp Immunol 121:437–443. doi:10.1046/j.1365-2249.2000.01324.x
Rodriguez BL, Lau N, Burchfiel CM et al (1999) Glucose intolerance and 23-year risk of coronary heart disease and total mortality: the Honolulu Heart Program. Diabetes Care 22:1262–1265. doi:10.2337/diacare.22.8.1262
Coutinho M, Gerstein HC, Wang Y et al (1999) The relationship between glucose and incident cardiovascular events. A metaregression analysis of published data from 20 studies of 95, 783 individuals followed for 12.4 years. Diabetes Care 22:233–240. doi:10.2337/diacare.22.2.233
The DECODE study group on behalf of the European Diabetes Epidemiology Group (1999) Glucose tolerance and mortality: comparison of WHO and American Diabetic Association diagnostic criteria. Diabetes Epidemiology: collaborative analysis of diagnostic criteria in Europe. Lancet 354:617–621
Nakagami T (2004) Hyperglycaemia and mortality from all cause and from cardiovascular disease in five populations of Asian origin. Diabetologia 47:385–394. doi:10.1007/s00125-004-1334-6
Puls W, Keup U, Krause HP et al (1977) Glucosidase inhibition. A new approach to the treatment of diabetes, obesity, and hyperlipoproteinaemia. Naturwissenschaften 64:536–537. doi:10.1007/BF00483562
Chiasson JL, Josse RG, Gomis R et al (2002) Acarbose for prevention of type 2 diabetes mellitus: the STOP-NIDDM randomized trial. Lancet 359:2072–2077. doi:10.1016/S0140-6736(02)08905-5
Chiasson JL, Josse RG, Gomis R et al (2003) Acarbose treatment and the risk of cardiovascular disease and hypertension in patients with impaired glucose tolerance: the STOP-NIDDM trial. JAMA 290:486–494. doi:10.1001/jama.290.4.486
Hanefield M, Chiasson JL, Koehler C et al (2004) Acarbose slows progression of intima-media thickness of the carotid arteries in subjects with impaired glucose tolerance. Stroke 35:1073–1078. doi:10.1161/01.STR.0000125864.01546.f2
Hanefeld M, Cagatay M, Petrowitsch T et al (2004) Acarbose reduces the risk for myocardial infarction in type 2 diabetic patients: meta-analysis of seven long-term studies. Eur Heart J 25:10–16. doi:10.1016/S0195-668X(03)00468-8
Osumi K, Ozeki Y, Saito S et al (2001) Development and assessment of enzyme immunoassay for platelet-derived microparticles. Thromb Haemost 85:326–330
Nomura S, Uehata S, Saito S (2003) Enzyme immunoassay detection of platelet-derived microparticles and RANTES in acute coronary syndrome. Thromb Haemost 89:506–512
Packham MA, Mustard JF (1986) The role of platelets in the development and complications of atherosclerosis. Semin Hematol 23:8–19
Sims PJ, Faioni EM, Wiedmer T et al (1988) Complement proteins C5b-9 cause release of membrane vesicles from the platelet surface that are enriched in the membrane receptor for coagulation factor Va and express prothrombinase activity. J Biol Chem 263:18205–18212
Nomura S, Suzuki M, Katsura K et al (1995) Platelet-derived microparticles may influence the development of atherosclerosis in diabetes mellitus. Atherosclerosis 116:235–240. doi:10.1016/0021-9150(95)05551-7
Nomura S, Tandon NN, Nakamura T et al (2001) High-shear-stress-induced activation of platelets and microparticles enhances expression of cell adhesion molecules in THP-1 and endothelial cells. Atherosclerosis 158:277–287. doi:10.1016/S0021-9150(01)00433-6
Nomura S, Shouzu A, Omoto S et al (1998) Effect of cilostazol on soluble adhesion molecules and platelet-derived microparticles in patients with diabetes. Thromb Haemost 80:388–392
Nomura S, Inami N, Iwasaka T et al (2004) Platelet activation markers, microparticles and soluble adhesion molecules are elevated in patients with arteriosclerosis obliterans: therapeutic effects by cilostazol and potentiation by dipyridamole. Platelets 15:167–172. doi:10.1080/09537100410001682779
Nomura S, Takahashi N, Inami N et al (2004) Probucol and ticlopidine: effect on platelet and monocyte activation markers in hyperlipidemic patients with and without type 2 diabetes. Atherosclerosis 174:329–335
Ceriello A (1999) Hyperglycaemia: the bridge between non-enzymatic glycation and oxidative stress in the pathogenesis of diabetic complications. Diabetes Nutr Metab 12:42–46
Yamagishi S, Nakamura K, Takeuchi M (2005) Inhibition of postprandial hyperglycemia by acarbose is a promising therapeutic strategy for the treatment of patients with the metabolic syndrome. Med Hypotheses 65:152–154. doi:10.1016/j.mehy.2004.12.008
Ouchi N, Kihara S, Arita Y et al (1999) Novel modulator for endothelial adhesion molecules: adipocyte-derived plasma protein, adiponectin. Circulation 100:2473–2476
Ouchi N, Kihara S, Arita Y et al (2000) Adiponectin, an adipocyte-derived plasma protein, inhibits endothelial NF-kappa B signaling through a cAMP-dependent pathway. Circulation 102:1296–1301
Hotta K, Funahashi T, Arita Y et al (2000) Plasma concentrations of a novel, adipose-specific protein, adiponectin, in type 2 diabetes patients. Arterioscler Thromb Vasc Biol 20:1595–1599
Shimabukuro M, Higa N, Asahi T et al (2003) Hypoadiponectinemia is closely linked to endothelial dysfunction in man. J Clin Endocrinol Metab 88:3236–3240. doi:10.1210/jc.2002-021883
Chen H, Montagnani M, Funahashi T et al (2003) Adiponectin stimulates production of nitric oxide in vascular endothelial cells. J Biol Chem 278:45021–45026. doi:10.1074/jbc.M307878200
Hattori Y, Suzuki M, Hattori S et al (2003) Globular adiponectin upregulates nitric oxide production in vascular endothelial cells. Diabetologia 46:1543–1549. doi:10.1007/s00125-003-1224-3
Nomura S, Shouzu A, Omoto S et al (2008) Correlation between adiponectin and reduction of cell adhesion molecules after pitavastatin treatment in hyperlipidemic patients with type 2 diabetes mellitus. Thromb Res 122:39–45. doi:10.1016/j.thromres.2007.08.013
Wang Y, Lam KS, Chan L et al (2006) Post-translational modifications of the four conserved lysine residues within the collagenous domain of adiponectin are required for the formation of its high molecular weight oligomeric complex. J Biol Chem 281:16391–16400. doi:10.1074/jbc.M513907200
Fülöp N, Marchase RB, Chatham JC (2007) Role of protein O-linked N-acetyl-glucosamine in mediating cell function and survival in the cardiovascular system. Cardiovasc Res 73:288–297. doi:10.1016/j.cardiores.2006.07.018
Fülöp N, Mason MM, Dutta K et al (2007) Impact of Type 2 diabetes and aging on cardiomyocyte function and O-linked N-acetylglucosamine levels in the heart. Am J Physiol Cell Physiol 292:C1370–C1378. doi:10.1152/ajpcell.00422.2006
Ochiai H, Ooka H, Shida C et al (2008) Acarbose treatment increases serum total adiponectin levels in patients with type 2 diabetes. Endocr J 55:549–556. doi:10.1507/endocrj.K07E-107
Acknowledgments
This study was partly supported by a grant from the Japan Foundation of Neuropsychiatry and Hematology Research, a Research Grant for Advanced Medical Care from the Ministry of Health and Welfare of Japan, and a Grant (13670760 to S. Nomura) from the Ministry of Education, Science and Culture of Japan.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Shimazu, T., Inami, N., Satoh, D. et al. Effect of acarbose on platelet-derived microparticles, soluble selectins, and adiponectin in diabetic patients. J Thromb Thrombolysis 28, 429–435 (2009). https://doi.org/10.1007/s11239-008-0301-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11239-008-0301-3