Abstract
Background
Adhesions due to the reactions caused by the grafts used in primary vascular operations can lead to various problems when a secondary operation is necessary. These problems include bleeding, injuries to neighboring organs, and complications occurring due to a prolonged operation. We investigated the effects of sirolimus, which has antiproliferative features, on vascular adhesions.
Methods
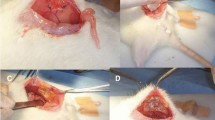
The abdominal aorta of rats was explored and abrasions applied. Following the fixation of a polytetrafluoroethylene (PTFE) graft on the abdominal aorta, sirolimus (rapamycin) is applied (in powdered form) onto the grafts of the study group. Eight weeks later a laparotomy was repeated and any adhesions were evaluated.
Results
In the study group the adhesions were determined to be fewer in number and milder in severity. Severe cases of adhesion were determined in the control group.
Conclusions
Therefore, sirolimus applied around the prosthesis in vascular operations was determined to be effective at preventing possible adhesions.


Similar content being viewed by others
References
Gutmann J, Penzias A, Diamond MP. Adhesions in reproductive surgery. In: Wallach E, Zacur HI, editors. Reproductive medicine and surgery. Missouri, Mosby 1995, pp 691–693
Whawell SA, Vipond MN, Scott-Coombes DM, et al. Plasminogen activator inhibitor-2 reduces peritoneal fibrinolytic activity in inflammation. Br J Surg 1993;80:107–109
Sehgal SN, Baker H, Vezina C. Sirolimus (AY-22,989), a new antifungal antibiotic. II. Fermentation, isolation, and characterization. J Antibiot 1975;28:727–731
Morris RE. Sirolimus: antifungal, antitumor, antiproliferative and immunosuppressive macrolides. Transplant Rev 1992;6:39–87
Roque M, Reis ED, Cordon-Cardo C, et al. Effect of p27 deficiency and sirolimus on intimal hyperplasia: in vivo and in vitro studies using a p27 knockout mouse model. Lab Invest 2001;81:895
Marx SO, Marks AR. The development of sirolimus and its application to stent restenosis. Circulation 2001;104:852–855
Sousa JE, Costa MA, Abizaid A, et al. Lack of neointimal proliferation after implantation of sirolimus-coated stents in human coronary arteries: a quantitative coronary angiography and three-dimensional intravascular ultrasound study. Circulation 2001;103:192–195
Sousa JE, Costa MA, Abizaid A, et al. Sustained suppression of neointimal proliferation by sirolimus-eluting stents. One-year angiographic and intravascular ultrasound follow-up. Circulation 2001;104:2007–2011
Linsky CB, Diamond MP, Cunningham T, et al. Adhesion reduction in a rabbit uterine horn model using an absorbable barrier, TC-7. J Reprod Med 1987;32:17–20
Naylor AR, Ah-See AK, Engeset J, et al. Graft occlusion following aortofemoral bypass for peripheral ischaemia. Br J Surg 1989;76(6):572–575
Holmdahl L. Making and covering of surgical footprints. Lancet 1999;353(9163):1456–1457
Hendrikx M, Mees U, Hill AC, et al. Evaluation of a novel synthetic sealant for inhibition of cardiac adhesions and clinical experience in cardiac surgery procedures. Heart Surg Forum 2001;4(3):204–210
Becker JM, Dayton MT, Fazio VW, et al. Prevention of postoperative abdominal adhesions by a sodium hyaluronate-based bioresorbable membrane: a prospective, randomized, double-blind multicenter study. J Am Coll Surg 1996;183:297–306
Bakkum EA, Van Blitterswijk CA, Dalmeijer RAJ, et al. A semiquantitative rat model for intraperitoneal postoperative adhesion formation. Gynecol Obstet Invest 1994;37:99–105
Buckman RF, Woods M, Sargent L, et al. A unifying pathogenetic mechanism in the etiology of intraperitoneal adhesions. J Surg Res 1976;20(1):1–5
Holmdahl L, Al-Jabreen M, Xia G, et al. The impact of starch powdered gloves on the formation of adhesions in rats. Eur J Surg 1994;160:257–261
Belluco C, Meggiolaro F, Pressato D. Prevention of postsurgical adhesions with an autocrosslinked hyaluronan derivative gel. J Surg Res 2001;100:217–221
Wiseman DM, Haung WJ, Johns DB, et al. Time-dependent effect of tolmetin sodium in rabbit uterine adhesion model. J Invest Surg 1994;7:527–532
Kahan BD, Gibbons S, Tejpal N, et al. Synergistic interactions of cyclosporine and sirolimus to inhibit immune performances of normal human peripheral blood lymphocytes in vitro. Transplantation 1991;51:232–239
Tu Y, Stepkowski SM, Chou T-C, et al. The synergistic effects of cyclosporine, sirolimus, and brequinar on heart allograft survival in mice. Transplantation 1995;59(2):177–183
Knight R, Ferraresso M, Serino F, et al. Low-dose sirolimus potentiates the effects of subtherapeutic doses of cyclosporine to prolong renal allograft survival in the mongrel canine model. Transplantation 1993;55(4):947–949
Ferraresso M, Tian L, Ghobrial R, et al. Sirolimus inhibits production of cytotoxic but not noncytotoxic antibodies and preferentially activates T helper 2 cells that mediate long-term survival of heart allografts in rats. J Immunol 1994;153(7):3307–3318
Segal SN, Camardo JS, Scarola JA, et al. Sirolimus (Sirolimus, rapamune). Curr Opin Nephrol Hypertens 1995;4:482–487
Molnar-Kimber KL, Rhoad A, Warner L, et al. Evidence that the anti-tumor and immunosuppressive effects of sirolimus are mediated via similar mechanisms. Cold Spring Harbor Meeting on Cell Cycle, 18–22 May 1994. New York, Cold Spring Harbor Laboratory, 1994, p 141
Schachner T, Zou Y, Oberhuber A, et al. Local application of sirolimus inhibits neointimal hyperplasia in experimental vein grafts. Ann Thorac Surg 2004;77:1580–1585
Schatz RA, Penn IM, Baim DS. Stent restenosis study (STRESS): analysis of in-hospital results [abstract]. Circulation 1993;88[Suppl I]:1–594
Roque M, Cordon-Cardo C, Fuster V, et al. Modulation of apoptosis, proliferation, and p27 expression in a porcine coronary angioplasty model. Atherosclerosis 2000;153:315–322
Suzuki T, Kopia G, Hayashi S-I, et al. Stent based delivery of sirolimus reduces neointimal formation in a porcine coronary model. Circulation 2001;104:1188–1193
Fukuda D, Sata M, Tanaka K, et al. Potent inhibitory effect of sirolimus on circulating vascular progenitor cells. Circulation 2005;111:926–931
Braun-Dullaeus RC, Mann MJ, Dzau VJ. Cell cycle progression: new therapeutic target for vascular proliferative disease. Circulation 1998;98:82–89
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kanko, M., Ozbudak, E., Ozerdem, A. et al. Effect of Sirolimus in the Prevention of Adhesions Around Intraabdominal Prosthetic Graft. World J. Surg. 30, 1648–1652 (2006). https://doi.org/10.1007/s00268-005-0750-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-005-0750-1