Abstract
Objectives
To compare plasma levodopa concentrations after repeated doses of levodopa/carbidopa/entacapone (LCE) and levodopa/carbidopa (LC).
Methods
Open-label, randomized, two-period, active-controlled, cross-over study with four dosing regimens: groups I and II (healthy volunteers and Parkinson’s disease patients) received levodopa 100 mg or 150 mg four times daily, respectively, and groups III and IV (healthy volunteers) received the same strengths of levodopa five times daily. Pharmacokinetic (PK) parameters determined for levodopa included Cmin, Cmax, Cmax − Cmin, AUC, t1/2, and tmax.
Results
In healthy volunteers and PD patients, mean trough levels (Cmin), Cmax, and AUC of levodopa were, in general, significantly higher during LCE compared to LC administration. Compared to Cmin, Cmax, and AUC, differences between the treatments in variability of levodopa concentrations (Cmax − Cmin) were less consistent.
Conclusions
The present results on the differences in levodopa PK between LCE and LC provide a basis to evaluate the relationship of levodopa PK and the induction of motor complications in an on-going study in early Parkinson’s disease using similar dosing regimens.
Similar content being viewed by others
Introduction
The motor symptoms of Parkinson’s disease (PD) are mainly due to the loss of dopaminergic innervation of the striatum. Therefore, the most successful treatment strategies are those that replenish striatal dopamine levels or mimic the action of dopamine.
Levodopa is still the most effective treatment for the symptoms of PD. Levodopa is metabolized mainly by two enzymes, dopa decarboxylase (DDC) and catechol O-methyltransferase (COMT). Levodopa is nowadays always combined with a DDC inhibitor (DDCI; carbidopa or benserazide), which improves the delivery of levodopa to the brain. However, blocking DDC shifts the peripheral metabolism of levodopa towards COMT, with O-methylation becoming the prominent metabolic pathway [1]. Therefore, oral levodopa therapy can be further improved by COMT-inhibitors.
Entacapone is a selective, reversible, peripherally acting COMT-inhibitor [2]. The pharmacokinetic (PK) profiles of entacapone and levodopa are comparable and the time course of COMT inhibition by entacapone also follows the plasma-concentration-time curve (AUC) of entacapone [2]. Therefore, entacapone is always taken together with each dose of levodopa/DDCI. Tolcapone is another clinically available COMT-inhibitor [3] that is taken three times daily (t.i.d) regardless of the dosing frequency of levodopa/DDCI. Oral levodopa therapy with levodopa/DDCI and entacapone or tolcapone is associated with an improved levodopa plasma profile (increased AUC and elimination half-life) and prolonged therapeutic response in patients with PD [4–6]. This improved pharmacokinetic profile of levodopa has been shown to translate into decreased “off-time” and increased “on-time” in PD patients with wearing-off symptoms [7–10]. Both COMT-inhibitors also improve levodopa’s effects in the symptomatic treatment of early PD patients [11–12].
The current concept of continuous dopaminergic stimulation (CDS) suggests that a more stable plasma concentration of a given dopaminergic drug will result in a prolonged response to treatment. Additionally, it has been postulated that pulsatile stimulation of striatal post-synaptic dopamine receptors may lead to a series of molecular and physiological changes that are thought to underlie the development of motor complications, such as dyskinesia and wearing-off [13]. In particular, studies with continuous enteral infusion of levodopa indicate that maintaining plasma levodopa concentrations above a minimum antiparkinsonian threshold by avoiding low trough concentrations may be a key factor in optimizing treatment response and reducing motor complications [14–15]. Interestingly, these benefits seem to be independent of maximum levodopa concentrations (Cmax) and some fluctuation in plasma levels [15].
Whether the improved levodopa plasma profile seen with COMT-inhibitors can reduce motor complications has so far been studied in treatment-naive N-methyl-4-phenyl-1,2,3,6-tetrahydropyridine (MPTP) primates, a widely recognized animal model for PD. Smith et al. [16] have shown that treatment of MPTP-treated primates with four daily doses of levodopa/carbidopa (LC) and entacapone was equally effective, but produced less dyskinesia compared with those treated with an equivalent daily-dosing regimen of LC alone. Based on the CDS concept and the results reported by Smith et al. [16], a large, international, double-blind, randomized study is currently on-going in patients with early PD without motor complications who require the initiation of levodopa therapy [17]. The hypothesis of this study is that frequent dosing of levodopa/carbidopa/entacapone (LCE) will delay the onset of dyskinesia compared to treatment with equivalent doses of LC. The two main maintenance-dose levels in this study are LCE 100/25/200 mg or 150/37.5/200 mg, or equivalent doses of LC administered four times daily at 3.5-h intervals.
If the hypothesis of this study holds true, it will be very important to determine which differences in the daily PK profiles of LCE and LC translate into a reduced risk of motor complications during long-term therapy. For this purpose, a study divided into two parts, the first part conducted in healthy volunteers and the other in PD patients, was designed to compare the PK profile of levodopa during treatment with LCE and LC with the above-mentioned treatment regimens. We also studied levodopa plasma profiles in healthy volunteers receiving five daily doses of LCE and LC to see whether more frequent dosing would make any further difference between the two treatments.
Materials and methods
Study design and treatments
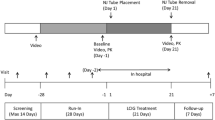
The study was conducted in two parts. Part 1 was an open-label, randomized, active-controlled, two-period, cross-over PK study conducted in healthy volunteers. Subjects were enrolled into one of four dosing groups. Group I received 100 mg levodopa, four times daily every 3.5 h; group II 150 mg levodopa, four times daily every 3.5 h; group III 100 mg levodopa, five times daily every 3.0 h; and group IV 150 mg levodopa, five times daily every 3.0 h. Each parallel group had a cross-over design with their respective LCE and LC strengths. Part 2 was conducted in PD patients and was identical in design to part 1 with groups I and II as described above. The study part conducted in PD patients has been registered at http://www.clinicaltrials.gov/ (study code NCT00693862).
The study medication consisted of LCE 100 or LCE 150 (levodopa/carbidopa/entacapone, 100/25/200 mg or 150/37.5/200 mg tablets, respectively; Stalevo, Orion Corporation Orion Pharma, Espoo, Finland), and LC 100 or LC 150 (levodopa/carbidopa, 100/25 mg tablet or one 100/25 mg tablet given together with one 50/12.5 mg tablet, respectively; Sinemet, Merck, Sharp & Dohme, Haarlem, the Netherlands).
In each group (I–IV) of part 1, subjects were randomized to receive either LCE or LC during period 1 and then subsequently crossed over to the other drug in period 2. Study drug was up-titrated during the first treatment period due to the moderate daily levodopa doses used and to avoid possible adverse events (AEs), such as nausea. Between periods 1 and 2, there was no wash-out period to avoid the need for re-titration. Period 1 lasted for 4–7 days and period 2 lasted for 3 days. The length of the titration period was the same for all subjects within each treatment group. In part 2 conducted in PD patients, the appropriate study group for each subject was selected by the investigator according to the subject’s daily levodopa dose prior to the randomization. There was a wash-out period of 3–7 days between the treatment periods during which time the subjects continued on their individual daily levodopa treatment.
Both healthy volunteers and patients with PD fasted from 10:00 pm, but water was allowed up to 1 h before the first morning dose and subsequent PK assessment. All study treatment doses were ingested with 200 mL of water and the first morning dose was taken at approximately 08:00 am. The timing of food intake was standardized to avoid differences between the two periods in each group in this respect. Breakfast, lunch, dinner, and a light evening meal were served 1 h after each dose and a snack was given either 1 h before the third dose (groups I and II in healthy volunteers and PD patients with four daily doses) or 1 h after the third dose (groups III and IV in healthy volunteers with five daily doses).
Each dosing group had a standard 2 × 2 cross-over design and a block size of two was chosen for the randomization process. Since the study was open, no blinding was applied. The study was performed according to good clinical practice, reviewed by the local ethics committee, and approved by the Finnish national competent authority. All subjects gave their written informed consent.
Study population
Part 1 of the study was conducted in healthy male and female volunteers. Exclusion criteria included any condition requiring regular concomitant medication (except contraceptives or hormone replacement therapy) or other medication that could have affected the outcome of the study. PD patients (male or female) in part 2 had to be on three to five daily doses of levodopa/DDCI ± entacapone with a total daily levodopa dose in the range of 300–600 mg. One or more doses of controlled-release levodopa/DDCI preparations were allowed providing that they were included in the total of three to five daily doses mentioned above. These requirements regarding prior levodopa treatment were selected to ensure that patients could switch smoothly to their study dosing regimen. Levodopa/DDCI ± entacapone and other antiparkinsonian medications (dopamine agonists, MAO-B inhibitor, amantadine, and/or anticholinergics) were to be kept unchanged for at least 2 weeks prior to the first treatment period.
Blood sampling and determination of levodopa, carbidopa, and entacapone concentrations
Venous blood samples for the determination of levodopa and carbidopa levels were collected on PK assessment days prior to the morning dose and subsequently at 0.5- or 1-h intervals up to 16 h (groups I and II) or up to 17 h (groups III and IV in healthy volunteers). An additional blood sample was collected for subjects who received LCE prior to LC to ensure that no detectable levels of entacapone were present before the first dose of LC was administered on the day of the PK assessment for period 2. Plasma samples for levodopa and carbidopa analysis were stored with an antioxidant at –70˚C and samples for entacapone analysis at –20˚C.
Determination of carbidopa and levodopa in human plasma was carried out using HPLC method with EC detection. The sample preparation involved solid-phase extraction of plasma (0.5 mL) on RECIPE Clin Rep cartridges. Samples were stabilized with sodium pyrosulphite. The determination of the analytes was carried out within the calibration range of 2.5 ng/mL (LLOQ, lower limit of quantification) to 500 ng/mL (ULOQ, upper limit of quantification) for carbidopa and 25 ng/mL (LLOQ) to 5,000 ng/mL (ULOQ) for levodopa. During the study, the inter-assay accuracy, indicated by bias, was between -3.6 and 0.0% for carbidopa and 2.7 and 4.2% for levodopa; the precision, indicated by the coefficient of variation, was between 5.5 and 6.6% for carbidopa and 3.7 and 5.1% for levodopa.
Determination of entacapone in human plasma was carried out using the LC-MS/MS method. The sample preparation involved solid-phase extraction of plasma (0.25 mL) on Isolute MFC18 cartridges; D10-entacapone was used as internal standard. The analytical procedure was linear from 10.0 (LLOQ) to 1,000 (ULOQ) ng/mL. During the study (all determinations were done in one batch) the intra-assay inaccuracy was ±3% and the intra-assay imprecision <4%.
Pharmacokinetic analysis
A noncompartmental method was used to calculate the PK parameters of levodopa after each dose. PK parameters of levodopa included minimum observed concentration (Cmin), maximum observed concentration (Cmax), area under the curve calculated with the linear trapezoidal rule for each dose interval (AUCtau), time to reach the maximum observed concentration (tmax), and terminal elimination half-life (t1/2) after the last dose. Additionally, the means of the above PK parameters (except t1/2 and tmax) throughout the day and AUC0–14 or AUC0–15 (depending on the group) were also determined. Variability of levodopa plasma concentration during the day (fluctuation) was calculated by Cmax − Cmin (and not, for example, by the peak-through-fluctuation formula) because day-time variability was assessed after repeated doses during 1 day of study drug administration, and steady-state conditions were not reached. The PK parameters of interest for carbidopa were AUCtau for each dose interval, as well as AUC0–14 or AUC0–15.
Safety
Twelve-lead electrocardiogram (ECG), vital signs (systolic and diastolic blood pressure and heart rate), physical examination and routine laboratory safety parameters were used to monitor safety in each subject. Data on AEs were collected throughout the study and were classified according to version 9.1 of the Medical Dictionary for Regulatory Activities coding system.
Statistical analysis
The sample-size calculation was based on a previous study with four daily doses of controlled-release LC 100/25 mg and entacapone 200 mg given at 4-h intervals [18]. The sample size needed to produce a statistical power of 80% in this study was nine subjects (with a significance level of 5%). As there were no within-subject variance data available, this estimate was considered to be sufficient for a cross-over study. It was, therefore, decided to include 10 subjects in each study group.
The analyses of the primary and secondary variables were based on a comparison of all values after each levodopa dose between the LCE and LC treatments. All analyses were performed separately for each group. These variables were evaluated using analysis of variance for cross-over design, which included repeated measurements within the study periods. The statistical model included treatment, sequence, period, time, sequence × time, period × time, and treatment × time as fixed effects, and subject within sequence, period × subject within sequence, and time × subject within sequence as random effects (Wallenstein-Fisher model [19]). Values for AUC0–14 (or AUC0–15) and t1/2 were also compared using analysis of variance for cross-over design and included treatment, sequence, and period as fixed effects, and subject within sequence as the random effect. These analyses were performed separately for each group.
In all analyses, Cmin, AUCtau, Cmax, Cmax − Cmin, and AUC0–14 (or AUC0–15) were analyzed after logarithmic transformation to achieve normality assumption. Analyses of PK variables included all subjects participating in the study and providing calculable data from one or both periods. All tests were two-sided and used a 5% significance level. The 95% confidence intervals were calculated for the ratio of the geometric means within statistical models. No multiplicity corrections were made in the statistical analyses. All analyses were programmed with SAS 9.1.3 for Windows (SAS Institute, Cary, NC, USA).
Results
Study population
In part 1, a total of 53 healthy subjects were screened; of these, 41 subjects (33 women and 8 men) were enrolled and 37 subjects completed the study. The mean age of the 41 enrolled healthy subjects was 23.7 (range: 18–37) years, mean weight was 63 (50–85) kg, and mean body mass index (BMI) was 21.9 (19–27) kg/m2. No subject had any medical condition or was taking any concomitant medication that could have interfered with the interpretation of the results. In part 2, a total of 23 PD patients were screened, and 19 patients were enrolled, all completing the study. The mean age of the PD patients was 63.3 (range 57–71) years, mean weight was 81.7 (56–103) kg, and mean BMI was 28.2 (22–34) kg/m2. Mean duration of PD was 6.7 (range 0.4–14.1) years, and mean duration of levodopa treatment was 6.2 (0.4–13.3) years. In group I (n = 10), two patients had wearing-off symptoms and eight had stable disease. In group II (n = 9), six patients had wearing-off symptoms, and three had stable disease.
Pharmacokinetic results
Levodopa
Cmin in healthy volunteers
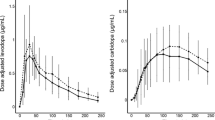
In all four dosing groups, the geometric means of all Cmin values from 0–14 h (0–15 h in groups III and IV) were significantly higher (by 78–105%, all P < 0.0001) with LCE compared with LC treatment (Fig. 1 and Table 1). The Cmin values after each LCE dose were also significantly higher (P < 0.0001) when compared with Cmin values after the respective LC dose (Fig. 1 and Table 2). Time × treatment interaction was statistically significant (P < 0.001) in group IV, i.e., the differences in mean Cmin values between the treatments increased towards the end of the day.
Cmin in PD patients
In groups I and II, the geometric means of all Cmin values from 0–14 h were significantly higher (by 89–100%, both P < 0.0001) with LCE compared with LC treatment. The Cmin values after each LCE dose were also significantly higher (P < 0.0001) when compared with Cmin values after the respective LC dose (Fig. 1).
Cmax in health volunteers
The mean of all Cmax values from 0–14 h (0–15 h for groups III and IV) was significantly higher (by 17–27%) in all groups (P < 0.05) after LCE treatment compared with LC treatment (Tables 1 and 3). In group I, the ratio between the treatments changed from the first dose to the later doses of the day, showing significant (P < 0.05) treatment × time interaction (Table 4).
Cmax in PD patients
The mean of all Cmax values from 0–14 h in group I was 8% higher during LCE treatment compared to LC, the difference being statistically nonsignificant (Table 3, P = 0.17). The difference remained nonsignificant also for each dosing interval (Table 4). In group II, the mean of all Cmax values from 0–14 h was 19% higher during LCE treatment compared to LC (Table 3, P < 0.01). However, when the difference was analyzed separately for each dosing interval, it was statistically significant only after the third and fourth dose due to significant treatment × time interaction (Table 4, P < 0.05).
AUCtau and AUC0–14 and AUC0–15 in healthy volunteers
In all groups, AUC0–14 and AUC0–15 values were significantly (P < 0.001) higher (by 34–46%) following LCE treatment compared with LC treatment (Tables 1 and 3). Similarly, AUCtau values for each dosing interval were generally significantly higher (P < 0.05) with two exceptions: after the first dose in group III and after the third dose in group IV (Table 2). Values for AUCtau increased towards the end of the day with both LCE and LC (the increase being greater with LCE) resulting in a significant treatment × time interaction (P < 0.05) in groups I, III, and IV (Tables 2 and 5).
AUCtau and AUC0–14 and AUC0–15 in PD patients
The AUC0–14 values in groups I and II were significantly (P < 0.0001) higher (by 32–39%) following LCE compared to LC (Table 3). Similarly, AUCtau values for each dosing interval in both groups were significantly higher following LCE (Table 5). The only exception was the first dosing interval (P = 0.06) in group II, in which treatment × time interaction was statistically significant (P < 0.01).
Variability of levodopa plasma concentrations, Cmax − Cmin, in healthy volunteers
The variability of levodopa plasma concentrations (Cmax − Cmin) during the day was slightly smaller (by 8–16%) during LCE treatment in all four groups (Table 1 and 3). However, the difference did not reach statistical difference in any of the groups. Cmax − Cmin values of levodopa between the treatments did not reach statistical significance during any of the individual dosing intervals in groups I, II, and III (Tables 2 and 6). In group IV, Cmax − Cmin of levodopa during LCE was significantly lower (P < 0.05) during the fourth dose of the day (Table 2).
Variability of levodopa plasma concentrations, Cmax − Cmin, in PD patients
In group I, the mean variability (Cmax − Cmin) during the day (0–14 h) was statistically significantly lower (by 18%, P < 0.05) during LCE compared to LC (Table 3). For separate dosing intervals, the difference was statistically significant favoring LCE only after the third dose (Table 6, P < 0.05). In contrast, there was no difference in the mean variability of levodopa plasma concentrations between the treatments in group II (Tables 3 and 6).
T1/2 after the last dose in healthy volunteers
Levodopa t1/2 after the last dose was longer after LCE treatment in all groups. Mean (SD) levodopa t1/2 in groups I and II were 1.3 (0.20) and 1.4 (0.17) h, respectively, following LC treatment, and 2.0 (0.37) and 1.9 (0.23) h, respectively, following LCE treatment (P < 0.001). Similarly, mean levodopa t1/2 in groups III and IV were 1.6 (0.64) and 2.1 (1.2) h, respectively, following LC treatment, and 2.5 (1.2) and 3.0 (1.4) h, respectively, following LCE treatment (P < 0.05 and P = 0.25, respectively).
T1/2 after the last dose in PD patients
Levodopa t1/2 after the last dose was longer after LCE treatment in both groups. Mean (SD) levodopa t1/2 in groups I and II were 1.3 (0.20) and 1.4 (0.17) h, respectively, following LC treatment, and 2.0 (0.37) and 1.9 (0.23) h, respectively, following LCE treatment (P < 0.001).
Tmax in healthy volunteers
In all four groups, median tmax occurred at 0.5–1.0 h and 1.5 h after the first doses of LC and LCE, respectively. After the second dose, the median tmax occurred at 1.0–1.5 h with LC and 1.5–2.0 h with LCE. Median tmax was usually observed at 1.5 h for latter doses of both LC and LCE.
Tmax in PD patients
Median tmax was 1.5 h after all doses of LCE in both groups. With LC, the median tmax was 0.5 h after the first dose and 1.5 h after the next doses.
Carbidopa
In healthy volunteers
There was no statistically significant difference between LCE and LC in terms of AUC covering the entire day (AUC0–14 or AUC0–15) in any of the groups. However, after the first dose of study treatment, AUCtau values were 15–28% lower (P < 0.05) with LCE compared with LC in groups I, III, and IV (data not shown).
In PD patients
There were no statistically significant differences in carbidopa AUC0–14 between LCE and LC treatments in groups I and II. All AUCtau values for each dosing interval during 0–14 h were statistically nonsignificant between the treatments. The only exception was AUCtau after the first dose in group II, which was significantly lower with LCE compared to LC (P < 0.01, data not shown).
Entacapone concentrations
In healthy volunteers and PD patients
In subjects treated with LCE in period 1 (sequence “LCE-LC”), all entacapone concentrations before the first dose of LC on the PK assessment day of period 2 were below the quantification limit of 10 ng/ml.
Safety
In healthy volunteers, the most common AEs reported during the study period were nausea, chromaturia, headache, vomiting, and dizziness. These occurred during LCE and/or LC treatments. The frequency and intensity of nausea and vomiting were higher with higher doses of study drugs.
In PD patients, most common AEs during the study periods were tremor, dizziness, headache, nausea, and chromaturia occurring during LC and/or LCE treatments. Nausea was clearly less common compared to healthy volunteers.
Vital signs and ECG data indicated no safety concerns during the study, and there were no consistent differences between LCE and LC treatment in this respect.
Discussion
This study was primarily designed to compare the levodopa concentration profiles throughout the day with the specific daily-dosing regimens of LCE and LC [100 or 150 mg of levodopa four times daily (q.i.d.) at 3.5-h intervals] that are used as the maintenance dose levels in a long-term clinical study comparing LCE and LC in the treatment of early PD [17].
In the present study, t1/2 of levodopa (measured after the last dose of the day) was longer after LCE administration in all groups compared to LC. Due to prolonged t1/2 of levodopa, both in healthy volunteers and PD patients, mean trough levels (Cmin), maximum observed concentrations (Cmax), and AUC values of levodopa were, in general, significantly higher throughout the day during LCE compared to LC administration. This was seen after all dosing regimens regardless of the dose strength, number of doses, or the dosing interval used. The biggest increases in levodopa PK variables after LCE were generally seen in Cmin and AUC, the mean increases ranging from approximately 1.3-fold (AUC in groups I–II) to 2.0-fold (Cmin in groups III–IV in healthy volunteers) compared to LC. In turn, Cmax of levodopa was 1.1- to 1.3-fold higher after LCE compared to LC in all groups. There were no differences in the Cmax of levodopa between LCE and LC after the first morning dose. This agrees with earlier studies conducted in healthy subjects [2] and patients with PD [5], which have shown that a single administration of LC and entacapone does not increase the Cmax of levodopa. With different dosing regimens, similar kinds of results (regarding t1/2, Cmin, Cmax, and AUC of levodopa) have been reported with repeated dosing of entacapone administered together with standard release levodopa/carbidopa [4–5] or with controlled-release levodopa/carbidopa [18]. It has also been reported that co-administration of tolcapone t.i.d. with four daily doses of levodopa/benserazide has significantly increased Cmin, Cmax, and AUC of levodopa by up to 2- to 3-fold compared to levodopa/benserazide alone [20].
As seen from daily plasma level curves (Figs. 2 and 3), levodopa concentrations tended to accumulate with both treatments towards the end of the day. These results are well in line with phase III results in patients with PD experiencing wearing-off, showing that increases in on-time with levodopa/dopa-decarboxylase inhibitor (DDCI) and entacapone therapy were more pronounced towards the end of the day [7]. In contrast to the pharmacokinetic parameters above, no significant differences were generally seen in variability (Cmax − Cmin) of levodopa concentrations during the day between LCE and LC, although there was a slight trend towards lower variability (by 8–16%) with LCE during all dosing regimens.
It is well known that there is a relatively large interindividual variability in levodopa absorption. There are many possible explanations for this, for example, different rates of gastric emptying [21]. However, our study demonstrated that PK of levodopa in PD patients can be predicted reasonably well based on results obtained from healthy volunteers. This was especially true for relative differences between the two levodopa formulations, but also the absolute levodopa plasma levels in groups I and II were close to each other between healthy volunteers and PD patients. This adds to the previous literature reporting that there are generally no differences in PK of levodopa between de novo PD patients, patients with wearing-off symptoms, or patients with late-stage disease [22].
Carbidopa concentration profiles were generally similar between LCE and LC throughout the day in the present study, i.e., entacapone did not affect carbidopa absorption and plasma concentrations in any clinically significant way during repeated dosing. The lack of quantifiable levels of entacapone prior to the first LC dose on the PK assessment day of period 2 in subjects who received LCE in period 1 ruled out carry-over effects from prior LCE treatment. As entacapone has been in clinical use for approximately 10 years already, our focus was not to study COMT-inhibition in detail. Therefore, no data on 3-OMD or other metabolites of levodopa or dopamine are reported.
The concept of continuous dopaminergic stimulation (CDS) suggests that a more stable plasma concentration of a given dopaminergic drug will result in a more continuous response to treatment with decreased incidence of motor complications [13]. It has also been claimed that maintaining plasma levodopa concentrations above a minimum antiparkinsonian threshold by avoiding low trough concentrations (Cmin) may be a key factor in optimizing treatment response and reducing motor complications [15]. However, in later-stage patients with wearing-off symptoms with or without existing dyskinesia, enhancing dopaminergic therapy with any oral medication will often increase dyskinesia to some extent in addition to expected antiparkinsonian effects. This is true also for enhancement of levodopa therapy with COMT-inhibitors [7, 10, 23–24].
In early (or de novo) PD without wearing-off symptoms and any dyskinesia, the situation may be different. So far there is only experimental evidence showing that, in de novo non-primed MPTP primates, treatment with LC and entacapone (compared to LC alone) induced less dyskinesia despite improving motor symptoms [16]. If the Cmin was the most important PK variable of levodopa for reducing the occurrence of motor complications in early PD, then LCE would better fulfil this criterion compared to LC. However, it is not known whether Cmin levels of levodopa in this study were high enough in this respect even with LCE. On the other hand, if significant difference in the variability of levodopa concentrations (Cmax − Cmin) was the key factor (regardless of the level at which this variability occurs), then the present study might support that there will be no significant difference in inducing motor complications between LCE and LC in early PD. The role of Cmax levels of a given drug in CDS also remains unclear. However, a recent study (in later-stage patients) suggested that it may be more important to avoid low trough levels of levodopa rather than to avoid higher Cmax levels [15].
In conclusion, the results of this study demonstrated that 100 or 150 mg of LCE administered four to five times daily at 3.0- to 3.5-h intervals provides a PK profile with higher Cmin, Cmax, and AUC of levodopa compared to LC. No unexpected tolerability issues were seen in any of the study groups. The avoidance of low troughs in plasma levodopa levels has been suggested to be one of the most important factors resulting in better symptomatic control of PD symptoms and delay in the development of treatment-associated motor complications. Whether the observed differences in trough levels and/or other PK variables of levodopa in this study translate into the delayed onset of motor complications in patients with early PD remains to be seen. The double-blind, randomized, controlled, multicenter, long-term study [17] comparing LCE and LC q.i.d. in early PD may provide an answer to this important question.
References
Männistö PT, Kaakkola S (1989) New selective COMT inhibitors: useful adjuncts for Parkinson’s disease. Trends Pharmacol Sci 10:54–56
Keränen T, Gordin A, Harjola VP et al (1993) The effect of catechol-O-methyltransferase inhibition by entacapone on the pharmacokinetics and metabolism of levodopa in healthy 48 volunteers. Clin Neuropharmacol 16:145–156
Dingemanse J, Jorga KM, Schmitt M et al (1995) Integrated pharmacokinetics and pharmacodynamics of the novel catechol-O-methyltransferase inhibitor tolcapone during first administration to humans. Clin Pharmacol Ther 57:508–17
Müller T, Erdmann C, Muhlack S et al (2006) Pharmacokinetic behaviour of levodopa and 3-O-methyldopa after repeat administration of levodopa/carbidopa with and without entacapone in patients with Parkinson’s disease. J Neural Transm 113:1441–1448
Nutt JG, Woodward WR, Beckner RM et al (1994) Effect of peripheral catechol-O- methyltransferase inhibition on the pharmacokinetics and pharmacodynamics of levodopa in parkinsonian patients. Neurology 44:913–919
Davis TL, Roznoski M, Burns RS (1995) Acute effects of COMT inhibition on L-DOPA pharmacokinetics in patients treated with carbidopa and selegiline. Clin Neuropharmacol 18:333–337
Parkinson Study Group (1997) Entacapone improves motor fluctuations in levodopa-treated Parkinson’s disease patients. Parkinson Study Group. Ann Neurol 42:747–755
Rinne UK, Larsen JP, Siden A et al (1998) Entacapone enhances the response to levodopa in parkinsonian patients with motor fluctuations. Nomecomt Study Group. Neurology 51:1309–1314
Kurth MC, Adler CH, Hilaire MS et al (1997) Tolcapone improves motor function and reduces levodopa requirement in patients with Parkinson’s disease experiencing motor fluctuations: a multicenter, double-blind, randomized, placebo-controlled trial. Tolcapone Fluctuator Study Group I. Neurology 48:81–87
Baas H, Beiske AG, Ghika J et al (1997) Catechol-O-methyltransferase inhibition with tolcapone reduces the “wearing off” phenomenon and levodopa requirements in fluctuating parkinsonian patients. J Neurol Neurosurg Psychiatry 63:421–428
Waters CH, Kurth M, Bailey P et al (1997) Tolcapone in stable Parkinson’s disease: efficacy and safety of long-term treatment. The Tolcapone Stable Study Group. Neurology 49:665–671
Hauser RA, Panisset M, Abbruzzese G et al (2008) Double-blind trial of levodopa/carbidopa/entacapone versus levodopa/carbidopa in early Parkinson’s disease. Mov Disord. doi:10.1002/mds.22343
Olanow CW, Obeso JA, Stocchi F (2006) Continuous dopamine-receptor treatment of Parkinson’s disease: scientific rationale and clinical implications. Lancet Neurol 5:677–687
Nyholm D, Aquilonius SM (2004) Levodopa infusion therapy in Parkinson disease: state of the art in 2004. Clin Neuropharmacol 27:245–256
Stocchi F, Vacca L, Ruggieri S et al (2005) Intermittent vs continuous levodopa administration in patients with advanced Parkinson disease: a clinical and pharmacokinetic study. Arch Neurol 62:905–910
Smith LA, Jackson MJ, Al-Barghouthy G et al (2005) Multiple small doses of levodopa plus entacapone produce continuous dopaminergic stimulation and reduce dyskinesia induction in MPTP-treated drug-naive primates. Mov Disord 20:306–314
Olanow CW (2006) The STRIDE-PD (Stalevo Reduction in Dyskinesia Evaluation) study: a long-term, controlled study to evaluate the effect of initiating Stalevo or carbidopa/levodopa in early PD. Eur J Neurol 13(Suppl 2):93
Paija O, Laine K, Kultalahti ER et al (2005) Entacapone increases levodopa exposure and reduces plasma levodopa variability when used with Sinemet CR. Clin Neuropharmacol 28:115–119
Wallenstein S, Fisher AC (1977) The analysis of the two-period repeated measurements crossover design with application to clinical trials. Biometrics 33:261–269
Baas H, Zehrden F, Selzer R et al (2001) Pharmacokinetic-pharmacodynamic relationship of levodopa with and without tolcapone in patients with Parkinson’s disease. Clin Pharmacokinet 40:383–393
Kurlan R, Rothfield KP, Woodward WR et al (1988) Erratic gastric emptying of levodopa may cause “random” fluctuations of parkinsonian mobility. Neurology 38:419–421
Fabbrini G, Juncos J, Mouradian MM et al (1987) Levodopa pharmacokinetic mechanisms and motor fluctuations in Parkinson’s disease. Ann Neurol 21:370–376
Kaakkola S, Teräväinen H, Ahtila S et al (1994) Effect of entacapone, a COMT inhibitor, on clinical disability and levodopa metabolism in parkinsonian patients. Neurology 44:77–80
Roberts JW, Cora-Locatelli G, Bravi D et al (1993) Catechol-O-methyltransferase inhibitor tolcapone prolongs levodopa/carbidopa action in parkinsonian patients. Neurology 43:2685–2688
Acknowledgements
The authors gratefully acknowledge levodopa/carbidopa bioanalytical work of AAIParma Deutschland, Neu-Ulm Germany, supervised by Carmen Dilger. The validation of the entacapone method and analysis of clinical samples was performed at SGS Life Science Services, 90 avenue des Hauts de la Chaume, 86281 Saint-Benoît Cedex, France, using an analytical method validated under the supervision of Murielle Brault. The authors would like to thank Iina Elo, MSc, for her assistance in the preparation of this manuscript, and Rachel Hood, MSc, for her editorial assistance with the figures and tables. Editorial assistance was funded by Orion Corporation Orion Pharma and Novartis Pharmaceuticals AG. The study was sponsored by Orion Corporation Orion Pharma.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Additional information
Marita Kailajärvi and Päivi Ruokoniemi were employed by CRST, University of Turku. Orion Corporation Orion Pharma was the sponsor of the study and paid compensation to CRST. Jutta Hänninen, Kirsi Korpela, Eliisa Löyttyniemi, Mikko Kuoppamäki and Juha Ellmén are employees of Orion Corporation Orion Pharma.
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Kuoppamäki, M., Korpela, K., Marttila, R. et al. Comparison of pharmacokinetic profile of levodopa throughout the day between levodopa/carbidopa/entacapone and levodopa/carbidopa when administered four or five times daily. Eur J Clin Pharmacol 65, 443–455 (2009). https://doi.org/10.1007/s00228-009-0622-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-009-0622-y