Abstract
Introduction
Some people with type 2 diabetes (T2D) require intensive insulin therapy to manage their diabetes. This can increase the risk of diabetes-related hospitalizations. We hypothesize that initiation of real-time continuous glucose monitoring (RT-CGM), which continuously measures a user’s glucose values and provides threshold- and trend-based alerts, will reduce diabetes-related emergency department (ED) and inpatient hospitalizations and concomitant costs.
Methods
A retrospective analysis of US healthcare claims data using Optum’s de-identified Clinformatics® Data Mart database was performed. The cohort consisted of commercially insured, CGM-naïve individuals with T2D who initiated Dexcom G6 RT-CGM system between August 1, 2018, and March 31, 2021. Twelve months of continuous health plan enrollment before and after RT-CGM initiation was required to capture baseline and follow-up rates of diabetes-related hospitalizations and associated healthcare resource utilization (HCRU) costs. Analyses were performed for claims with a diabetes-related diagnosis code in either (1) any position or (2) first or second position on the claim.
Results
A total of 790 individuals met the inclusion criteria. The average age was 52.8 (10.5) [mean (SD)], 53.3% were male, and 76.3% were white. For claims with a diabetes-related diagnosis code in any position, the number of individuals with ≥ 1 ED visit decreased by 30.0% (p = 0.01) and with ≥ 1 inpatient visit decreased by 41.5% (p < 0.0001). The number of diabetes-related visits and average number of visits per person similarly decreased by at least 31.4%. Larger relative decreases were observed for claims with a diabetes-related diagnosis code in the first or second position on the claim. Total diabetes-related costs expressed as per-person-per-month (PPPM) decreased by $341 PPPM for any position and $330 PPPM for first or second position.
Conclusion
Initiation of Dexcom G6 among people with T2D using intensive insulin therapy was associated with a significant reduction in diabetes-related ED and inpatient visits and related HCRU costs. Expanded use of RT-CGM could augment these benefits and result in further cost reductions.
Similar content being viewed by others
Why carry out this study? |
Individuals with type 2 diabetes (T2D) using intensive insulin therapy may be at increased risk for diabetes-related hospitalizations |
Real-time continuous glucose monitoring (RT-CGM) systems provide threshold- and trend-based alerts which notify users of current or impending glucose excursions |
We hypothesize that initiation of the Dexcom G6 RT-CGM system will reduce diabetes-related emergency department (ED) and inpatient hospitalizations and the costs associated with these events |
What was learned from the study? |
Among 790 included individuals, ED visits and inpatient visits decreased significantly after RT-CGM initiation (− 30.0%, p = 0.01, and − 41.5%, p < 0.0001, respectively). Relatedly, diabetes-related costs decreased by > $300 per-person-per-month |
Initiation of Dexcom G6 among people with T2D using intensive insulin therapy was associated with reductions in healthcare costs. Expanded use of RT-CGM could extend these benefits and result in further cost reductions |
Introduction
Type 2 diabetes (T2D) is a significant health concern in the USA with > 30 million adults diagnosed with the disease [1]. The already high prevalence of T2D is expected to increase by almost 50% globally by 2045 [2]. About one in four people with T2D use insulin [3, 4], and some require intensive insulin therapy to manage their condition, putting them at increased risk for acute diabetes-related events and hospitalizations.
The economic burden of T2D is significant and continues to strain the US health care system. In 2022, the total estimated cost of diabetes was > $410 billion, about three-fourths of which was due to direct medical costs [5]. Almost 30% of all hospital inpatient days were incurred by people with diabetes, a figure that far exceeds the roughly 10% of the US population who have diabetes [1, 5].
Increasingly, people with T2D use real-time continuous glucose monitoring (RT-CGM) systems to monitor their glucose levels and make treatment decisions. RT-CGM systems contain an adhesive patch and are applied to the body (usually the abdomen or upper arm) for 10–14 days. A thin wire measures glucose levels in the interstitial fluid and transmits a glucose value to a compatible smartphone or dedicated receiver every 1–5 min. Numerous randomized controlled trials and real-world studies have shown that RT-CGM use can improve glycemic control in people with T2D [6,7,8,9,10] and reduce diabetes-related hospitalizations [7, 9, 11]. The present study employed a retrospective analysis of administrative claims data to investigate the association between initiation of the Dexcom G6 RT-CGM system among people with T2D using intensive insulin therapy and the rate of diabetes-related emergency department (ED) and inpatient hospital visits. We hypothesize that these hospitalizations and the associated health care resource utilization (HCRU) costs will decrease after RT-CGM initiation.
Methods
Study Design
This observational, retrospective analysis used administrative claims data from US beneficiaries with commercial health insurance contained within Optum’s de-identified Clinformatics® Data Mart (CDM) database. The CDM database includes > 65 million unique lives over a 15-year period (January 2007 through March 2022). CDM administrative claims submitted for payment by providers and pharmacies are verified, adjudicated, and de-identified prior to inclusion. These data, including beneficiary-level enrollment information, are derived from claims submitted for all medical and pharmacy health care services with information related to health care costs and resource utilization. The authors licensed the use of the CDM from Optum and because the database is statistically de-identified and compliant with the Health Insurance Portability and Accountability Act (HIPAA), the study was deemed exempt from an ethics committee review.
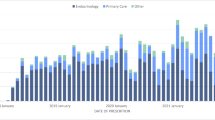
A modified Klompas algorithm was used to identify individuals with T2D [12]. The Klompas algorithm is used to classify and segregate individuals with type 1 versus type 2 diabetes using a combination of International Classification of Diseases (ICD)-9 or ICD-10 codes, medications, and laboratory test results. National drug codes (NDC) were used to identify those with at least one pharmacy claim for a Dexcom G6 RT-CGM system between August 1, 2018, and March 31, 2021 (study identification period). The index date was the earliest observed claim for Dexcom G6 within the identification period. Individuals were required to have 12 months of continuous health plan enrollment before the index date (baseline period) and after the index date (follow-up period). Individuals’ complete diabetes medication therapy (including therapies indicative of treatment with intensive insulin therapy), as well as diabetes-related comorbidities during baseline, was determined from NDC and Healthcare Common Procedure Coding System (HCPCS). Intensive insulin therapy required evidence of mixed insulin use or bolus insulin use with or without basal insulin use. People with type 1 diabetes, indication of pregnancy, Medicare health plan coverage, or any CGM use during baseline were excluded. Demographics, such as age, gender, and race, were captured from enrollment records.
Outcome Measure
Diabetes-related hospital visits (ED or inpatient) and associated HCRU costs were determined during the 12-month baseline and follow-up periods from ICD-10 diagnosis codes. Healthcare costs outside the ED or inpatient setting were not included. Events were defined as diabetes-related if the claim contained a diabetes diagnosis code. Codes related to hypoglycemia, hyperglycemia, and diabetic ketoacidosis are summarized in Supplementary Table 1. Events and related HCRU costs were separately analyzed by the position of the diagnosis code (any position on the claim or first or second position on the claim). These separate analyses based on the position of the diabetes-related code on the claim exist to capture situations where hyperglycemia or hypoglycemia was the likely primary reason for the visit (first or second position) as well as those where it was simply present (any position). Main outcomes included the difference in the prevalence of ED or inpatient visits, the proportion of individuals with at least one visit, and per-person-per-month (PPPM) HCRU costs (in 2021 US dollars) between the baseline and follow-up period.
Statistical Analysis
Descriptive statistics, including percentages, means, and standard deviations, were calculated for demographic characteristics and study outcomes. Differences in ED and inpatient encounters and PPPM costs between the baseline and follow-up periods were tested with paired t-tests or McNemar’s chi-squared tests, as appropriate, using Instant Health Data (Panalgo, Boston, MA). All statistical tests were two-tailed with p-values < 0.05 considered statistically significant.
Results
Data from 790 individuals with T2D using intensive insulin therapy were included in the analysis (see Supplementary Fig. 1 for a cohort attrition diagram). Average age was 52.8 ± 10.5 (mean ± SD) years, and the majority were male (53.3%) and white race (76.3%) (Table 1). The average Charlson comorbidity score was 1.72 ± 1.84, and the most common comorbidities were obesity (51.7%) and peripheral neuropathy (35.6%). The most-used medications were metformin (50.8%) and glucagon-like peptide 1 receptor agonists (37.7%).
Table 2 summarizes the prevalence of diabetes-related ED visits and inpatient hospitalizations experienced by people with T2D using intensive insulin therapy and the associated HCRU costs. The proportion of individuals experiencing either encounter decreased significantly, by at least 30%, independent of the position of the diabetes-related code on the claim. The number of hypoglycemia-related encounters declined during follow-up in all cases, and the proportion of claims with a hypoglycemia-related code in the first or second position declined during follow-up. In addition, the average number of diabetes-related visits to the ED or inpatient setting also significantly decreased.
Average hospitalization (ED + inpatient) costs for claims with a diabetes-related code in any position were $10,282 ± $34,594 during baseline and $6181 ± $34,642 during the follow-up period. The average PPPM hospitalization cost decreased by $341 from $856 during baseline to $515 during follow-up (p = 0.01) (Table 2). Similarly, average hospitalization costs for claims with a diabetes-related code in the first or second position on the claim were $6521 ± $28,475 during baseline and $2561 ± $17,391 during the follow-up period. In this analysis, the average PPPM hospitalization cost decreased by $330 from $543 to $213 (p = 0.0008) (Table 2).
Discussion
In this observational retrospective analysis of administrative claims data, initiation of RT-CGM was associated with significant reductions in diabetes-related ED or inpatient visits as well as significant reductions in diabetes-related HCRU costs. These results are in line with a similar analysis of people with T2D treated with insulin or non-insulin therapies who initiated RT-CGM [11].
Despite over $400 billion spent on diabetes in the US in 2022 [5], about half of those with T2D are not meeting treatment targets such as A1C < 7.0% [1]. This increases the risk of acute diabetes-related events and hospitalizations, as examined in this study, as well as long-term diabetes-related complications [13]. The risks associated with these complications can be mitigated with proper diabetes management and knowledge of one’s glucose values, which is particularly critical in the context of insulin dosing.
People with T2D using intensive insulin therapy are increasingly using RT-CGM to manage their diabetes and improve their health. The findings in this study indicate that significant reductions in diabetes-related HCRU were associated with initiation of Dexcom G6 RT-CGM in this population. This is supported by multiple studies that similarly demonstrate the cost reductions or cost-effectiveness of RT-CGM use in the insulin-using T2D population in the US [9, 11, 14] and globally [15,16,17].
While this study only analyzed individuals with T2D using intensive insulin therapy, the benefits of RT-CGM have been demonstrated in people using less intensive insulin therapy. In a recent randomized controlled trial, people with T2D treated with basal insulin experienced a significantly larger A1C improvement when using RT-CGM compared to those self-monitoring their blood glucose (i.e., fingerstick testing) [8]. In a large database study of people with T2D using insulin, the event rate for hypoglycemia-related ED or inpatient visits decreased by > 50% for RT-CGM initiators compared to a small increase for noninitiators [7]. Additional real-world evidence and cost effectiveness analyses are needed in basal insulin and non-insulin-using populations.
The benefits of RT-CGM and the continuous stream of glucose values it provides extend beyond practical items such as insulin dosing decisions. The use of remote monitoring features can improve quality of life and overall wellbeing among insulin-using individuals [18] and their caregivers or spouses/partners [19]. Additionally, a recent survey found that most users of retrospective data analysis software (such as Dexcom Clarity) reported improved hypoglycemic confidence and reduced diabetes distress [20]. Finally, CGM systems can act as motivational tools, encouraging users to engage in more healthful practices [21,22,23,24]. In fact, when use of RT-CGM systems is discontinued, about half of the glycemic improvements are lost [25].
Limitations of this study include the all-US population with commercial health insurance, which limits generalizability to other countries or insurance providers, such as Medicare or Medicaid. Demographic information was also limited and prevented further analysis of factors such as social determinants of health on CGM access [26, 27]. We also do not know whether, or to what extent, individuals used the RT-CGM to monitor their glucose. The study did not include a control group, and biases such as self-selection to RT-CGM and regression to the mean cannot be ruled out. It is possible that people who experienced a diabetes-related hospitalization initiated RT-CGM to prevent another occurrence. Relatedly, the follow-up period of 1 year was too short to derive conclusions related to durability of outcomes. However, this study provides real-world evidence that use of Dexcom G6 RT-CGM was associated with reduced event rates and lower medical costs, and it is possible that a longer observation window would amplify these cost savings. Finally, we only analyzed users of one RT-CGM system, Dexcom G6, so the results may not generalize to other CGM systems.
Conclusion
Overall, initiation of RT-CGM among people with T2D using intensive insulin therapy was associated with a significant reduction in diabetes-related ED and inpatient visits. This decrease in health care utilization resulted in a significant PPPM reduction in hospitalization costs. Greater awareness of the benefits of RT-CGM among payors and providers could result in expanded access and continued cost reductions.
Data Availability
The datasets generated and analyzed during the current study are not publicly available due to confidentiality.
References
Centers for Disease Control and Prevention National Diabetes Statistics Report. https://www.cdc.gov/diabetes/data/statistics-report/index.html. Accessed 12 Oct 2023.
International Diabetes Federation. IDF Diabetes Atlas, 10th edn. 2021. https://diabetesatlas.org/atlas/tenth-edition/. Accessed 29 Feb 2024.
Chehal PK, Uppal TS, Turbow S, et al. Continuity of medication use by US adults with diabetes, 2005–2019. JAMA Netw Open. 2023;6(1): e2253562. https://doi.org/10.1001/jamanetworkopen.2022.53562.
Diabetes UK. Insulin and type 2 diabetes. 2022. https://www.diabetes.org.uk/guide-to-diabetes/managing-your-diabetes/treating-your-diabetes/insulin/type-2-diabetes. Accessed 18 Jan 2024.
Parker ED, Lin J, Mahoney T, et al. Economic costs of diabetes in the U.S. in 2022. Diabetes Care. 2024;47(1):26–43. https://doi.org/10.2337/dci23-0085.
Beck RW, Riddlesworth TD, Ruedy K, et al. Continuous glucose monitoring versus usual care in patients with type 2 diabetes receiving multiple daily insulin injections: a randomized trial. Ann Intern Med. 2017;167(6):365–74. https://doi.org/10.7326/M16-2855.
Karter AJ, Parker MM, Moffet HH, Gilliam LK, Dlott R. Association of real-time continuous glucose monitoring with glycemic control and acute metabolic events among patients with insulin-treated diabetes. JAMA. 2021;325(22):2273–84. https://doi.org/10.1001/jama.2021.6530.
Martens T, Beck RW, Bailey R, et al. Effect of continuous glucose monitoring on glycemic control in patients with type 2 diabetes treated with basal insulin: a randomized clinical trial. JAMA. 2021;325(22):2262–72. https://doi.org/10.1001/jama.2021.7444.
Reaven PD, Newell M, Rivas S, Zhou X, Norman GJ, Zhou JJ. Initiation of continuous glucose monitoring is linked to improved glycemic control and fewer clinical events in type 1 and type 2 diabetes in the veterans health administration. Diabetes Care. 2023;46(4):854–63. https://doi.org/10.2337/dc22-2189.
Shields S, Norman GJ, Thomas R, Ciemins EL. HbA1c improvements after initiation of real-time continuous glucose monitoring in primary care patients with type 2 diabetes. J Diabetes Sci Technol. 2023;17(5):1423–4. https://doi.org/10.1177/19322968231171176.
Norman GJ, Paudel ML, Parkin CG, Bancroft T, Lynch PM. Association between real-time continuous glucose monitor use and diabetes-related medical costs for patients with type 2 diabetes. Diabetes Technol Ther. 2022;24(7):520–4. https://doi.org/10.1089/dia.2021.0525.
Klompas M, Eggleston E, McVetta J, Lazarus R, Li L, Platt R. Automated detection and classification of type 1 versus type 2 diabetes using electronic health record data. Diabetes Care. 2013;36(4):914–21. https://doi.org/10.2337/dc12-0964.
Diabetes Control and Complications Trial Research Group, Nathan DM, Genuth S, et al. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med. 1993;329(14):977–86. https://doi.org/10.1056/NEJM199309303291401.
Alshannaq H, Norman GJ, Lynch PM. 141-LB: Cost-effectiveness of real-time continuous glucose monitoring (rt-CGM) vs. intermittent-scanning continuous glucose monitoring (is-CGM) from a U.S. payer perspective in patients with type 2 diabetes on multiple daily injections of insulin (PwT2D on MDI). Diabetes. 2023. https://doi.org/10.2337/db23-141-LB.
Alshannaq H, Isitt JJ, Pollock RF, et al. Cost-utility of real-time continuous glucose monitoring versus self-monitoring of blood glucose in people with insulin-treated type 2 diabetes in Canada. J Comp Eff Res. 2023;12(10):e230075. https://doi.org/10.57264/cer-2023-0075.
Alshannaq H, Norman GJ, Willis M, Nilsson A. 142-LB: Cost-effectiveness of real-time continuous glucose monitoring (rt-CGM) vs. intermittent-scanning continuous glucose monitoring (is-CGM) in patients with type 2 diabetes on multiple daily injections of insulin (T2D MDI) in Canada. Diabetes. 2023. https://doi.org/10.2337/db23-142-LB.
Isitt JJ, Roze S, Sharland H, et al. Cost-effectiveness of a real-time continuous glucose monitoring system versus self-monitoring of blood glucose in people with type 2 diabetes on insulin therapy in the UK. Diabetes Ther. 2022;13(11–12):1875–90. https://doi.org/10.1007/s13300-022-01324-x.
Polonsky WH, Fortmann AL. Impact of real-time continuous glucose monitoring data sharing on quality of life and health outcomes in adults with type 1 diabetes. Diabetes Technol Ther. 2021;23(3):195–202. https://doi.org/10.1089/dia.2020.0466.
Polonsky WH, Fortmann AL. Impact of real-time CGM data sharing on quality of life in the caregivers of adults and children with type 1 diabetes. J Diabetes Sci Technol. 2022;16(1):97–105. https://doi.org/10.1177/1932296820978423.
Polonsky WH, Soriano EC, Fortmann AL. The role of retrospective data review in the personal use of real-time continuous glucose monitoring: perceived impact on quality of life and health outcomes. Diabetes Technol Ther. 2022;24(7):492–501. https://doi.org/10.1089/dia.2021.0526.
Yoo HJ, An HG, Park SY, et al. Use of a real time continuous glucose monitoring system as a motivational device for poorly controlled type 2 diabetes. Diabetes Res Clin Pract. 2008;82(1):73–9. https://doi.org/10.1016/j.diabres.2008.06.015.
Farhan HA, Bukhari K, Grewal N, Devarasetty S, Munir K. Use of continuous glucose monitor as a motivational device for lifestyle modifications to improve glycaemic control in patients with type 2 diabetes treated with non-insulin therapies. BMJ Case Rep. 2022. https://doi.org/10.1136/bcr-2021-248579.
Fritschi C, Kim MJ, Srimoragot M, Jun J, Sanchez LE, Sharp LK. “Something tells me I can’t do that no more”: experiences with real-time glucose and activity monitoring among underserved black women with type 2 diabetes. Sci Diabetes Self Manag Care. 2022;48(2):78–86. https://doi.org/10.1177/26350106221076042.
Vallis M, Ryan H, Berard L, et al. How continuous glucose monitoring can motivate self-management: can motivation follow behaviour? Can J Diabetes. 2023;47(5):435–44. https://doi.org/10.1016/j.jcjd.2023.04.001.
Aleppo G, Beck RW, Bailey R, et al. The effect of discontinuing continuous glucose monitoring in adults with type 2 diabetes treated with basal insulin. Diabetes Care. 2021;44(12):2729–37. https://doi.org/10.2337/dc21-1304.
Ni K, Tampe CA, Sol K, Richardson DB, Pereira RI. Effect of CGM access expansion on uptake among patients on Medicaid with diabetes. Diabetes Care. 2023;46(2):391–8. https://doi.org/10.2337/dc22-1287.
Kanbour S, Jones M, Abusamaan MS, et al. Racial disparities in access and use of diabetes technology among adult patients with type 1 diabetes in a U.S. academic medical center. Diabetes Care. 2023;46(1):56–64. https://doi.org/10.2337/dc22-1055.
Funding
Dexcom, Inc. funded the analysis and the journal’s Rapid Service Fee.
Author information
Authors and Affiliations
Contributions
Katia L. Hannah, Poorva M. Nemlekar, and Gregory J. Norman conceived of the study. Katia L. Hannah collected and analyzed the data. Katia L. Hannah, Poorva M. Nemlekar, Courtney R. Green, and Gregory J. Norman contributed to data interpretation. Courtney R. Green wrote the first draft of the manuscript. Katia L. Hannah, Poorva M. Nemlekar, Courtney R. Green, and Gregory J. Norman critically revised the manuscript and approved the final manuscript version.
Corresponding author
Ethics declarations
Conflict of Interest
Katia L. Hannah, Poorva M. Nemlekar, Courtney R. Green, and Gregory J. Norman are employees of Dexcom, Inc.
Ethical Approval
This submitted work did not involve study subject recruitment, enrollment, or participation in a trial. As a retrospective observational study, it used only existing anonymized electronic medical record and billing data licensed by the authors from Optum. The Optum Clinformatics® database is statistically de-identified and HIPAA-compliant, and therefore the study was deemed exempt from an ethics committee review. No intervention was implemented for the purpose of the study and no patient-identifiable information was used in the study. The study was compliant with the Helsinki Declaration of 1964 and its later amendments.
Additional information
Prior presentation: Portions of this article were presented at the 83rd Scientific Sessions of the American Diabetes Association held in San Diego, CA, on June 23–26, 2023.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Hannah, K.L., Nemlekar, P.M., Green, C.R. et al. Reduction in Diabetes-Related Hospitalizations and Medical Costs After Dexcom G6 Continuous Glucose Monitor Initiation in People with Type 2 Diabetes Using Intensive Insulin Therapy. Adv Ther (2024). https://doi.org/10.1007/s12325-024-02851-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12325-024-02851-8