Abstract
Applications of bioluminescence for the in vivo study of pathogenic microorganisms are numerous, ranging from the quantification of virulence gene expression to measuring the effect of antimicrobial molecules on the colonization of tissues and organs by the pathogen. Most studies are performed in mice, but recent works demonstrate that this technique is applicable to larger animals like fish, guinea pigs, ferrets, and chickens. Here, we describe the construction and the utilization of a constitutively luminescent strain of Salmonella Typhimurium to monitor in vivo and ex vivo the colonization of mice in the gastroenteritis, typhoid fever, and asymptomatic carriage models of Salmonella infection.
You have full access to this open access chapter, Download protocol PDF
Similar content being viewed by others
Key words
1 Introduction
Bacterial infections are an important economic and public burden. Given the great diversity of potential hosts and their respective pathogens, the complexity of their interactions and the diversity of induced pathologies, numerous models were designed during the last decades to investigate these processes in vivo, sometimes focusing on one particular phenomenon. These experiments often aim to study how the pathogen colonizes and survives within the host. Usually, it involves the sacrifice of numerous animals and it is clear that bacterial infections might differ from one individual to another, even in the toughest experimental conditions.
Salmonella for example, is an enteric pathogen responsible for typhoid fever and gastroenteritis in a broad range of species, depending on the infecting serovar. Sometimes an asymptomatic carrier state can also be observed. Three murine models are commonly used to study these phenomena in vivo [1, 2]. The first model involves Slc11a1+/+ (Nramp1) mice (such as CBA/J or 129sv mice) which present an asymptomatic carrier state when infected with the pathogen. After oral inoculation, no inflammation is induced in the intestine, and postintestinal colonization is rigorously controlled by the host’s immune system, thus limiting deep organs damaging. Salmonella-induced typhoid fever can be studied through oral infection of Slc11a1-deficient mice (e.g., BALB/c, C57BL/6) with S. Typhimurium. As the pathogen crosses the intestinal barrier, its replication is not repressed, leading to a systemic colonization of deeper organs. This model is used to study human infections with typhoidal serovars like S. Typhi or S. Paratyphi which are human restricted and are consequently not able to infect mice. The use of S. Typhimurium in mice simulates well typhoidal infections in humans. Finally, the third model is based on antibiotic pretreatment of mice which results in microbiota alteration, leading to a bloom of S. Typhimurium intestinal colonization, and the induction of inflammation responsible for the gastroenteritis phenomenon [3]. This model is thus more relevant to study pathogenesis following human or animal infection with nontyphoidal serovars (e.g., S. Typhimurium and S. Enteritidis).
As an alternative to theses burdensome protocols, in vivo bioluminescence and fluorescence imaging is increasingly being used to perform real-time monitoring of disease process, especially infectious diseases [4], and to analyze the effect of therapeutic molecules or vaccines against pathogens [5,6,7]. Luminescence monitoring is allowed by devices such as the IVIS Spectrum (PerkinElmer) or the PhotonIMAGER (Biospace Lab), engineered to detect low levels of light emitted from luciferase or fluorescent reporters on small living animals. One of the most used bioluminescence reporters is the luxCDABE operon of Photorhabdus luminescens [8]. Basically, the LuxAB (Luciferase) complex enzyme catalyzes the oxidation of reduced flavin mononucleotide (FMNH2) and a long-chain fatty aldehyde to oxidized flavin and a long-chain fatty acid. On the other hand, the LuxCDE (fatty acid reductase) complex produces long chain fatty aldehyde by reducing the fatty acid previously produced. The excess energy for the reaction catalyzed by the LuxAB complex will result in the emission of blue/green light (490 nm).
Using the constitutive synthetic promoter described by Shivak et al. [9], termed sig70c35 and designed on the basis of the consensus binding sequence of the transcription factor σ70, we performed week-long monitoring of Salmonella colonization in the three main murine models of Salmonella infection described above. A strain harbouring the same construct, but depleted from any promoter, was also used in these experiments as a negative control. It allowed us to quantify the basal signals emitted by mice and their organs (spleen, liver, mesenteric lymph nodes [MLN], gut), and to determine a threshold for bioluminescence detection. This work provides relevant information about tracking of pathogenic microorganisms in animal models and can be adapted to other fields of research, for example as a tool to assess the impact of potential antimicrobial molecules on pathogen colonization [10, 11] or gene expression measurement [12, 13]. The most popular animal model for these imaging studies remains the mouse, but some recent works have used larger animals. For example, ferrets and guinea pigs have been used for bioluminescent imaging of influenza virus infection or colonization by a luciferase-expressing Brucella suis vaccine strain, respectively [14, 15]. Furthermore, infection of rainbow trout by the fish pathogen Vibrio anguillarum was directly analyzed by bioluminescent imaging and a luminescent avian E. coli strain was imaged in chicken to follow its colonization of the gastrointestinal tract [16, 17].
2 Materials
2.1 Tn7 Chromosomal Integration of Reporter Fusions
-
1.
Bacterial strain with a single attTn7 insertion site, S. Typhimurium 14028 in our experiments (see Note 1).
-
2.
TSB (Tryptic soy broth) medium.
-
3.
TSA (Tryptic soy agar) medium.
-
4.
Antibiotics: chloramphenicol (Cm) or kanamycin (Kan), and ampicillin (Amp) or carbenicillin (Cb).
-
5.
pCS26-sig70c35-luxCDABE (CmR or KanR) [9].
-
6.
pUC18R6K-miniTn7T-PacI (AmpR) [9].
-
7.
pHSG415-tnsABCD (AmpR) (see Note 2) [9].
-
8.
Escherichia coli CC118 λpir (or any E. coli λpir strain) [18] and MC1061 [19].
-
9.
Restriction enzymes and their appropriate buffer: PacI, XhoI, and BamHI.
-
10.
DNA Blunting kit (e.g., DNA Blunting kit, Takara).
-
11.
Clean-Up PCR kit (e.g., Macherey Nagel™ Nucleospin ™ Gel and PCR Clean-Up kit).
-
12.
Ligation kit (e.g., DNA Ligation kit v2.1, Takara).
-
13.
Genomic DNA extraction kit (e.g., Macherey Nagel™ NucleoSpin® Tissue kit).
-
14.
Primer glmS-For: 5′-AACCATCAGCGCGGAACAACTGGTC-3′ (see Note 3).
-
15.
Primer glmS-Rev: 5′-ATGCCGCATGTGGAAGAGGTCATTG-3′ (see Note 3).
2.2 Inoculum Preparation
-
1.
1 L Erlenmeyer.
-
2.
1.8 mL cryogenic vials.
-
3.
50% glycerol solution in saline water (0.85% NaCl).
2.3 Mouse Models
-
1.
6–8-week-old BALB/c (Slc11a1−/−) or CBA/J (Slc11a1+/+) female mice.
-
2.
200 mg/mL streptomycin solution.
-
3.
Mouse clipper and depilatory cream.
-
4.
Appropriate syringe and gavage needles [a dosing curved cannula 25 mm × 20G (Harvard Apparatus) and a 1 mL syringe in our case].
2.4 In Vivo Experiment and Bacterial Numeration
-
1.
Imaging instrument suitable for in vivo bioluminescence imaging equipped with a cooled −90 °C camera with large CCD area and low F-stop (e.g., IVIS Spectrum In Vivo Imaging System [PerkinElmer] or any equivalent imaging instrument).
-
2.
Anesthesia device coupled to the imaging instrument (e.g., XGI-8 Anesthesia system, PerkinElmer).
-
3.
Nose cones depending on the animal model and the in vivo imaging device. In our case, we used XNC-2 Mouse Nose Cones branded by PerkinElmer.
-
4.
Low luminescence matt black sheet.
-
5.
Dissection kit.
-
6.
Weighted blender bags (1/organ of interest/mouse).
-
7.
Petri dishes containing selective medium [Salmonella-Shigella (SS) agar supplemented with antibiotic, 30 μg/mL chloramphenicol in our case]. We recommend 150 mm diameter petri dishes when using an automatic plater.
-
8.
Bagmixer (e.g., MiniMix CC, Interscience).
-
9.
Automatic plater (e.g., easySpiral Pro, Interscience) or dilution tubes with 1.8 mL saline water.
-
10.
Automatic colonies counter (e.g., Scan 4000, Interscience).
3 Methods
3.1 Construction of a No Promoter (NoP) Reporter Transcriptional Fusion (See Note 4)
-
1.
Bacterial cultures are always performed at 37 °C in TSB or TSA medium containing appropriate antibiotics unless otherwise stated (strains grown at 30 °C).
-
2.
Digest pCS26-sig70c35-luxCDABE (CmR or KanR) by XhoI and BamHI and purify the resulting linear DNA product.
-
3.
Blunt the XhoI-BamHI restricted pCS26-sig70c35-luxCDABE vector (using a DNA Blunting kit) and perform ligation on the resulting DNA molecule.
-
4.
Transform the ligated product into competent E. coli MC1061 and plate the bacteria on TSA supplemented with the appropriate antibiotic (30 μg/mL Cm or 50 μg/mL Kan).
-
5.
Successful clones can be easily selected using IVIS Spectrum (or any other imaging instrument suitable for bioluminescence imaging) by checking the loss of bioluminescence. Constructions are then checked by PCR and DNA sequencing.
3.2 Chromosomal Integration of Reporter Fusions (See Note 5)
-
1.
Electroporate pHSG415-tnsABCD in competent bacteria of interest harbouring an attTn7 site (S. Typhimurium ATCC 14028 in our case) and select on TSA containing 100 μg/mL Amp at 30 °C. Verify the introduction of the plasmid into the bacteria and freeze the strain in 25% glycerol at −80 °C.
-
2.
Digest pCS26-sig70c35-luxCDABE (or the plasmid built in Subheading 3.1) and pUC18R6K-miniTn7T-PacI by PacI.
-
3.
Purify the resulting linear DNA products (pCS26-sig70c35-luxCDABE: 8086 bp; pUC18R6K-miniTn7T-PacI: 3216 bp).
-
4.
Ligate both purified DNA fragments using the DNA ligation kit, transform the ligated product into competent E. coli CC118 λpir cells and select on TSA containing 100 μg/mL Amp supplemented with the appropriate antibiotic (30 μg/mL Cm or 50 μg/mL Kan). Verify the plasmid by restriction digestion and freeze the strain in 25% glycerol at −80 °C.
-
5.
Cultivate the AmpR/CmR or AmpR/KanR clones and isolate the resulting plasmid (see Note 6). Electroporate it in pHSG415-tnsABCD-carrying bacteria cultivated at 30 °C with antibiotics. After resuspension, let the bacteria multiply for 2 h at 30 °C with agitation (190 rpm), before plating on TSA supplemented with the appropriate antibiotic (30 μg/mL Cm or 50 μg/mL Kan) at 37 °C to eliminate pHSG415-tnsABCD.
-
6.
Removal of pHSG415-tnsABCD plasmid is checked by plating the clones on TSA containing 30 μg/mL Cm (or 50 μg/mL Kan) and TSA containing 100 μg/mL Amp. Only clones sensitive to 100 μg/mL Amp are kept.
-
7.
Cultivate AmpS/CmR or AmpS/KanR clones in standard conditions and extract total DNA.
-
8.
Confirm the insertion of the reporting fusion by PCR using primers glmS-For and glmS-Rev (Fig. 1).
-
9.
After verification by DNA sequencing, freeze selected clones in 25% glycerol at −80 °C: two with the no promoter fusion (NoP) and two with the constitutive promoter fusion (Lux+).
Schematic representation of the insertion of the transcriptional fusion expressing constitutively the lux operon into the chromosome of S. Typhimurium 14028. Orange arrows represent genes carried by the Salmonella chromosome while the lux operon as well as the antibiotic resistance gene are indicated by blue arrows. The constitutive sig70c35 promoter is symbolized by the red broken arrow. The left and rights ends of Tn7 are indicated with black triangles. Restriction sites (X, XhoI; B, BamHI) are shown in black letters on both sides of the constitutive promoter. Deletion of the DNA sequence located between these two restriction sites in the pCS26-sig70c35-luxCDABE plasmid yielded the no promoter transcriptional fusion (NoP). Primers used to verify the chromosomal insertion of the transcriptional fusion are represented by grey arrows above phoS and glmS genes. The two possible insert orientations in the chromosome after Tn7 transposition are shown
3.3 Preparation of Inocula (See Note 7)
-
1.
Grow the previously constructed bacteria in 10 mL of TSB supplemented with the appropriate antibiotic overnight at 37 °C with agitation (190 rpm). The next day, sow 400 mL of TSB supplemented with the appropriate antibiotic with 4 mL of preculture and incubate for 24 h at 37 °C with agitation (190 rpm).
-
2.
Centrifuge (4800 × g; 20 min), and discard the supernatant. Resuspend the bacteria in 20 mL of saline water containing 50% glycerol. The volume of resuspension depends on the desired final concentration of the inoculum. In our case, this protocol generates inocula at a concentration of approximately 1 × 1011 CFU/mL.
-
3.
Distribute 1.2 mL of the obtained solution within 1.8 mL cryogenics vials and store them at −80 °C.
-
4.
The following day, thaw one inoculum and numerate it to help adjusting the bacterial concentration before inoculation. Numeration can be performed on the automatic plater (easySpiral Pro) or by serial dilutions in saline water.
3.4 Preparation of Animals
Animal experiments have to be performed with the approval of an Ethical Committee for Animal Research, in compliance with ethical guidelines respecting the “Replacement, Reduction and Refinement” rule as much as possible and they must be carried out in a certified animal facility.
-
1.
It is strongly recommended prior to the experiment, especially in case of gastrointestinal imaging study, to perform quantification of bioluminescence on isolated food chip to check if it is signal-free.
-
2.
A few days before inoculation, shave the fur in areas where signals will be looked for (e.g., ventral side and left side for the digestive tract and spleen for Salmonella) (see Note 8) and apply a depilatory cream (choose a cream without autoluminescent signal) on the mowed areas to remove the remaining hair. Leave to act for 3 min then rinse with lukewarm water (see Note 9). Dry the animals as much as possible by placing them in a cage under a heating lamp. Then place back the animals in their cages and increase the temperature of the room, where the animals are housed, at 24 °C.
3.5 Mice Infection, Anesthesia, and Imaging
-
1.
For the gastroenteritis-induced Salmonella model, animals must be fasted 4 h prior to streptomycin inoculation. Orally inoculate the mice with streptomycin (20 mg/animal in 0.1 mL of saline water) 24 h prior to Salmonella inoculation.
-
2.
Prior to Salmonella inoculation, animals must also be fasted for food and water (2 h prior inoculation for the typhoid fever and the asymptomatic carriage models; 4 h for the gastroenteritis model).
-
3.
Before inoculation, unfreeze one (or more depending on the number of mice) inoculum and adjust the bacterial concentration to the desired concentration (2.5 × 109 CFU/mL in our case) in saline water.
-
4.
Using a dosing curved cannula 25 mm × 20G (Harvard Apparatus) and a 1 mL syringe, orally inoculate 5 × 108 CFU of the reporter strains suspended in 0.2 mL of saline water per mice (see Note 7). Replace animals in boxes, provide water and food ad libitum.
-
5.
At each time point of interest, anesthetize first one negative control mouse (NoP) and second 4 tested mice (Lux+) in the induction chamber following institutional guidelines (e.g., 3% Vetflurane mixed 1.5 liter per minute O2). Then transfer them on the black flat sheet placed on the 37 °C thermostated platform inside the imager. Put the nose of each mouse in one nose cone that delivers Vetflurane (3%) mixed oxygen (1.5 L/min) gas (see Note 10). The induction chamber is sanitized with 70% alcohol after the anesthesia of each group of mice.
-
6.
Acquire a photographic image and the bioluminescence signal (Living Image 4.5.5 software from PerkinElmer allows data acquisition) first automatically and then manually if required (Fig. 2a). Exposure time depends on the intensity of the luminescent signal, ranging from 0.75 to 600 s. Exposing for a too long time may generate saturated signals, but exposing for too short time may not allow the detection of weak signals. Reiterate on all relevant sides of the mouse body. After imaging, it is important to ensure that the animals wake up well (see Note 11).
-
7.
Euthanize an animal for each required time point (see Note 12), remove aseptically each organ of interest (e.g., gut, spleen, liver) and place them in a nonreflective sterile petri dish inside the imaging device. Acquire the bioluminescence signal first automatically and then manually if required (Fig. 2b). This step will allow to identify the positive organ(s) and to quantify the signal in this organ.
-
8.
Collect imaged organs in preweighted blender bag with filter and weigh the bag to estimate organ’s weight. Small organs such as the ileal Peyer’s patches can be collected in preweighted tubes, and ground with sterile glass stirring rod.
-
9.
Depending on the size of the organ, add aseptically 1 mL (e.g., Peyer’s patches), 3 mL (e.g., MLN, spleen) or 5 mL (e.g., liver, gut) of TSB and homogenize using a Bagmixer (in our case, with the MiniMix CC set at speed 4 for 2 min).
-
10.
Plate 50 μL of the homogenized solution on one 150 mm petri dish containing SS medium with 30 μg/mL Cm or with 50 μg/mL Kan using an automatic plater (e.g., easySpiral Pro, Interscience) set on exponential mode. Depending on the colonization level of the organ and on the dilution apparatus used, it could be necessary to dilute the sample (10−2 or 10−4) and to plate it on a second petri dish using the automatic plater on exponential mode (see Note 13).
-
11.
Incubate overnight at 37 °C and count the colonies using a colony counter after adjusting dilution parameters (see Note 14).
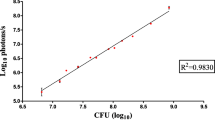
In vivo imaging of infection with a Salmonella strain expressing constitutively the lux operon in a murine gastroenteritis model. BALB/c mice pretreated with streptomycin were orally infected with S. Typhimurium 14028 carrying the mock fusion (no promoter: NoP) or the sig70c35-luxCDABE transcriptional fusion (Lux+). (a) One control mouse (NoP) and four Lux+ mice were imaged at 24 h and 76 h postinfection with the IVIS Spectrum. The exposure time expressed in seconds is indicated in the upper left corner of each image. The color scale shows relative signal intensity or radiance (expressed in p/sec/cm2/sr), red being the most intense and blue the least intense. The minimal and maximal values measured are indicated in the box below the color scale. (b) Isolated organs from one Lux+ mouse (indicated by a white asterisk in the upper part of the figure) were imaged at both time points. Organs on the images are indicated with white arrows. C cecum, Co colon, L liver, MLN mesenteric lymph nodes, PP Peyer’s patches, S spleen. (c) Quantification of luminescence (calculated from the ROI of each organ) and bacterial loads on the different isolated organs. Orange and blue bars represent the radiance of the different organs from Lux+ and NoP mice, respectively. For NoP mice, average values (±standard error of the mean) of radiance were calculated based on all euthanized control mice. For both time points, note that some organs which appeared negative on the images in (b) were really positive when the radiance was quantified (for example, MLN at 24 h postinfection). Black dashes correspond to bacterial loads of the organs from the Lux+ mouse
3.6 Bioluminescence Quantification
Living Image 4.5.5 software (PerkinElmer) allows data analysis. After acquisition, each image is displayed and is the result of the coregistration of a photographic image and a luminescent image.
-
1.
Visualize each image of interest in pseudocolors that represent intensity, for example violet for the smallest number on the color scale, red for the largest number, and all of the spectral colors of the rainbow for the values in between (Fig. 2a, b). Pixels reporting less intense signals might not be displayed at the selected scale.
-
2.
Define one or more regions of interest (ROI) in the optical image, for example measurement on abdominal area from the whole-body animal (Fig. 3a) or subject ROI on isolated organs such as spleen, liver, mesenteric lymph nodes, Peyer’s patches and gut defined regions (Fig. 3b). The Living Image 4.5.5 software (PerkinElmer) records information about the ROIs. Display the ROI measurements table and export as an Excel format.
-
3.
Analyze data. Quantification could be expressed in counts/second, or using the calibrated measurement units of the photon emission from the subject in photons/second/cm2/steradian, that is, radiance. The radiance unit is the number of photons per second that leave a square centimeter of tissue into a solid angle of one steradian (Fig. 2c). Working with image data in radiance mode allows the quantitative comparison of images or ROI data regardless of the acquisition settings and the imaging device used.
Examples of ROI (regions of interest) measurements on mice orally infected with S. Typhimurium 14028 in the murine gastroenteritis model. (a) One control mouse (NoP) and four Lux+ mice were imaged at 76 h postinfection with the IVIS Spectrum. The color scale shows relative signal intensity or radiance (expressed in p/sec/cm2/sr), red being the most intense and blue the least intense. The ROIs were defined manually and are expressed in p/sec/cm2/sr. The ROI measurements of the 4 Lux+ mice were 16 to 188 times higher than that of the NoP mouse which corresponds to the background. (b) Isolated organs from the Lux+ mouse indicated by a white asterisk in the upper part of the figure were imaged and the ROIs were carefully defined in order to take into account the entire organs. In accordance with the bacterial loads of the different organs shown in Fig. 2c at 76 h postinfection, the cecum and the ileum exhibit the highest ROI measurements. C cecum, Co colon, D duodenum, I ileum, J jejunum, L liver, MLN mesenteric lymph nodes, PP Peyer’s patches, S spleen
4 Notes
-
1.
Tn7 transposition was shown to be very effective in several enterobacterial species including E. coli, numerous S. enterica serovars, Klebsiella pneumoniae, Cronobacter sakazakii, and Citrobacter rodentium [20] and in Pseudomonas aeruginosa [21]. Since almost all bacterial genomes contain a single attTn7 site, this technique should be applicable to many other bacterial species [22].
-
2.
pHSG415-tnsABCD is a thermosensitive plasmid. Bacterial strain carrying such a plasmid should not be cultivated over 30 °C except for the curing step.
-
3.
Primers glmS-For and glmS-Rev were designed for S. Typhimurium ATCC 14028 genome (GenBank accession number CP001363). They hybridize with the 3′ end of the genes glmS and phoS respectively (Fig. 1). Other primers hybridizing on both sides of the insertion site should be designed if chromosomal integration is performed on any other bacterial genomes.
-
4.
Construction of a mock reporting transcriptional fusion (no promoter fusion) will allow determining the background bioluminescence emitted by both living animals and isolated organs.
-
5.
In vivo studies can also be performed using luminescent transcriptional fusions carried by plasmids. The advantage is an increase of the sensitivity due to the higher copy number compared to the chromosomal fusion. A potential drawback is a possible instability and therefore loss of the plasmid for experiments spanning several days. This is the case for pCS26-derived constructions which were starting to be lost in our murine models as early as 48 h postinoculation.
-
6.
Insertion of pCS26-luxCDABE restriction products can result in two possible orientations within pUC18R6K-miniTn7T-PacI vector and therefore in the bacterial strains after Tn7 transposition (Fig. 1). In order to homogenize multiple reporting strains, it is strongly recommended to check the orientation of the insert before electroporation. However, it should be noted that, in agreement with previous results [9], both orientations exhibited only a weak difference of lux expression in liquid culture.
-
7.
Depending on the Salmonella serovar and strain used, it is recommended to adapt the inoculum according to the virulence properties of the strain. For other pathogens of interest, please refer to literature in order to prepare the inoculum in the recommended conditions.
-
8.
If an animal is accidently hurt during this step, it is not recommended to apply depilatory cream as it could irritate the animal.
-
9.
For the comfort of the animals during the experiment, it is recommended to watch over them after application of the cream to avoid spread of the depilatory cream on their face (especially the eyes and the mouth).
-
10.
It is not recommended to anesthetize an animal more than three times a day, especially during the later stage of infection due to a certain fragility of infected mice at these times. Moreover, in order not to leave the mice anesthetized for a too long period, the negative control mouse (NoP) should be changed every 20–30 min.
-
11.
According to the kinetics of infection and the severity of the disease, animals can be imaged one or more times a day (up to three times). The first week, for all our Salmonella models, mice were imaged three times the first day and two times the other days. During the second week of the asymptomatic carriage experiment, mice were imaged once a day.
-
12.
Cervical elongation is the simplest method and does not requires any special equipment. It can be performed on anesthetized animals. Other methods of euthanasia can be applied depending on the sensitivity of the experimenter toward this method (CO2, etc.). Be careful to use a euthanizing method allowed by your institutional ethic committee regulations.
-
13.
Alternatively, each sample can be serially diluted and plated on petri dishes. The use of an automatically diluter allows to save time and petri dishes as maximum two dishes are required for an organ.
-
14.
When studying Salmonella and using SS plates, it is not recommended to note the petri dish with any other color than green as it could be interpreted by the apparatus as a colony.
References
Ruby T, McLaughlin L, Gopinath S et al (2012) Salmonella’s long-term relationship with its host. FEMS Microbiol Rev 36:600–615. doi:https://doi.org/10.1111/j.1574-6976.2012.00332.x
Simon R, Tennant SM, Galen JE et al (2011) Mouse models to assess the efficacy of non-typhoidal Salmonella vaccines: revisiting the role of host innate susceptibility and routes of challenge. Vaccine 29:5094–5106. https://doi.org/10.1016/j.vaccine.2011.05.022
Barthel M, Hapfelmeier S, Quintanilla-Martínez L et al (2003) Pretreatment of mice with streptomycin provides a Salmonella enterica serovar Typhimurium colitis model that allows analysis of both pathogen and host. Infect Immun 71:2839–2858
Avci P, Karimi M, Sadasivam M et al (2018) In vivo monitoring of infectious diseases in living animals using bioluminescence imaging. Virulence 9:28–63. https://doi.org/10.1080/21505594.2017.1371897
Bailleul G, Guabiraba R, Virlogeux-Payant I et al (2019) Systemic administration of avian defensin 7: distribution, cellular target, and antibacterial potential in mice. Front Microbiol 10:541. https://doi.org/10.3389/fmicb.2019.00541
Bernocchi B, Carpentier R, Lantier I et al (2016) Mechanisms allowing protein delivery in nasal mucosa using NPL nanoparticles. J Control Release 232:42–50. https://doi.org/10.1016/j.jconrel.2016.04.014
Ducournau C, Nguyen TT, Carpentier R et al (2017) Synthetic parasites: a successful mucosal nanoparticle vaccine against Toxoplasma congenital infection in mice. Future Microbiol 12:393–405. https://doi.org/10.2217/fmb-2016-0146
Waidmann MS, Bleichrodt FS, Laslo T et al (2011) Bacterial luciferase reporters: the Swiss army knife of molecular biology. Bioeng Bugs 2:8–16. https://doi.org/10.4161/bbug.2.1.13566
Shivak DJ, MacKenzie KD, Watson NL et al (2016) A modular, Tn7-based system for making bioluminescent or fluorescent Salmonella and Escherichia coli strains. Appl Environ Microbiol 82:4931–4943. https://doi.org/10.1128/AEM.01346-16
McCloskey MC, Shaheen S, Rabago L et al (2019) Evaluation of in vitro and in vivo antibiotic efficacy against a novel bioluminescent Shigella flexneri. Sci Rep 9:13567. https://doi.org/10.1038/s41598-019-49729-2
Xiong YQ, Willard J, Kadurugamuwa JL et al (2005) Real-time in vivo bioluminescent imaging for evaluating the efficacy of antibiotics in a rat Staphylococcus aureus endocarditis model. Antimicrob Agents Chemother 49:380–387. https://doi.org/10.1128/AAC.49.1.380-387.2005
Aviv G, Elpers L, Mikhlin S et al (2017) The plasmid-encoded Ipf and Klf fimbriae display different expression and varying roles in the virulence of Salmonella enterica serovar Infantis in mouse vs. avian hosts. PLoS Pathog 13:e1006559. https://doi.org/10.1371/journal.ppat.1006559
Azriel S, Goren A, Rahav G et al (2016) The stringent response regulator DksA is required for Salmonella enterica serovar Typhimurium growth in minimal medium, motility, biofilm formation, and intestinal colonization. Infect Immun 84:375–384. https://doi.org/10.1128/IAI.01135-15
Karlsson EA, Meliopoulos VA, Savage C et al (2015) Visualizing real-time influenza virus infection, transmission and protection in ferrets. Nat Commun 6:6378. https://doi.org/10.1038/ncomms7378
Wang X, Li Z, Li B et al (2016) Bioluminescence imaging of colonization and clearance dynamics of Brucella suis vaccine strain S2 in mice and Guinea pigs. Mol Imaging Biol 18:519–526. https://doi.org/10.1007/s11307-015-0925-6
Litvak Y, Mon KKZ, Nguyen H et al (2019) Commensal Enterobacteriaceae protect against Salmonella colonization through oxygen competition. Cell Host Microbe 25:128–139. https://doi.org/10.1016/j.chom.2018.12.003
Weber B, Chen C, Milton DL (2010) Colonization of fish skin is vital for Vibrio anguillarum to cause disease. Environ Microbiol Rep 2:133–139. https://doi.org/10.1111/j.1758-2229.2009.00120.x
Herrero M, de Lorenzo V, Timmis KN (1990) Transposon vectors containing non-antibiotic resistance selection markers for cloning and stable chromosomal insertion of foreign genes in gram-negative bacteria. J Bacteriol 172:6557–6567. https://doi.org/10.1128/jb.172.11.6557-6567.1990
Casadaban MJ, Cohen SN (1980) Analysis of gene control signals by DNA fusion and cloning in Escherichia coli. J Mol Biol 138:179–207. https://doi.org/10.1016/0022-2836(80)90283-1
Crépin S, Harel J, Dozois CM (2012) Chromosomal complementation using Tn7 transposon vectors in Enterobacteriaceae. Appl Environ Microbiol 78:6001–6008. https://doi.org/10.1128/AEM.00986-12
Choi K-H, Schweizer HP (2006) mini-Tn7 insertion in bacteria with single attTn7 sites: example Pseudomonas aeruginosa. Nat Protoc 1:153–161. https://doi.org/10.1038/nprot.2006.24
Choi K-H, Gaynor JB, White KG et al (2005) A Tn7-based broad-range bacterial cloning and expression system. Nat Methods 2:443–448. https://doi.org/10.1038/nmeth765
Acknowledgments
The authors wish to thank A. White for the kind gift of pCS26-sig70c35-luxCDABE, pUC18R6K-miniTn7T-PacI, and pHSG415-tnsABCD plasmids. This work was supported by the ERANET InfectERA project “Sal host trop” funded by the Agence Nationale pour la Recherche and by the European Union’s Horizon 2020 Research and Innovation Programme under grant agreement No. 731014 (VetBioNet—Veterinary Biocontained facility Network). M. Koczerka holds a doctoral fellowship from the University of Tours (France).
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Open Access This chapter is licensed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence and indicate if changes were made.
The images or other third party material in this chapter are included in the chapter's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the chapter's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
Copyright information
© 2022 The Author(s)
About this protocol
Cite this protocol
Koczerka, M. et al. (2022). In Vivo Tracking of Bacterial Colonization in Different Murine Models Using Bioluminescence: The Example of Salmonella. In: Gal-Mor, O. (eds) Bacterial Virulence. Methods in Molecular Biology, vol 2427. Humana, New York, NY. https://doi.org/10.1007/978-1-0716-1971-1_19
Download citation
DOI: https://doi.org/10.1007/978-1-0716-1971-1_19
Published:
Publisher Name: Humana, New York, NY
Print ISBN: 978-1-0716-1970-4
Online ISBN: 978-1-0716-1971-1
eBook Packages: Springer Protocols