Abstract
Using advanced gene editing technologies, xenotransplantation from multi-transgenic alpha-1,3-galactosyltransferase knockout pigs has demonstrated marked prolongation of renal xenograft survival, ranging from days to greater than several months for life-supporting kidneys and >2 years in a heterotopic non-life-supporting cardiac xenograft model. However, continuous administration of multiple immunosuppressive drugs continues to be required, and attempts to taper immunosuppression have been unsuccessful. These data are consistent with previous reports indicating that the human-anti-porcine T cell response is similar or stronger than that across allogeneic barriers. Due to the strength of both the innate and adaptive immune responses in xenotransplantation, the level of continuous immunosuppression needed to control these responses and prolong xenograft survival has been associated with prohibitive morbidity and mortality. These facts provide compelling rationale to pursue a clinically applicable strategy for the induction of tolerance.
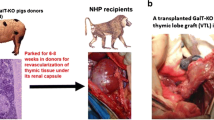
Mixed chimerism and thymic tissue transplantation have both achieved xenogeneic tolerance in pig-to-mouse models, and both have recently been extended to pig-to-baboon models. Although these strategies are promising in small animal models, neither direct intravenous injection of porcine bone marrow cells nor direct fetal thymic tissue transplantation into recipients was able to achieve >2 days chimerism following BM Tx or the engraftment of thymic tissues across xenogeneic barriers in pig-to-nonhuman primate models. Several innovative procedures have been largely developed by Kazuhiko Yamada to overcome these failures. These include vascularized thymic transplantation, combined with either thymokidney (TK) or vascularized thymic lobe (VTL) transplantation. Utilizing the strategy of transplanting vascularized thymic grafts with kidney from the same GalT-KO donor without further gene modification, we have achieved longer than 6 months survival of life-supporting kidneys in a baboon. Notably, the recipient became donor specific unresponsive and developed new thymic emigrants. In this chapter, we introduce a brief summary of our achievements to date toward the successful induction of tolerance by utilizing our novel strategy of vascularized thymic transplantation (including thymokidney transplantation), as well as describe the step-by-step methodology of surgical and in vitro procedures which are required for this experiment.
Access this chapter
Tax calculation will be finalised at checkout
Purchases are for personal use only
Similar content being viewed by others
References
Moses RD, Pierson RN 3rd, Winn HJ, Auchincloss H Jr (1990) Xenogeneic proliferation and lymphokine production are dependent on CD4+ helper T cells and self antigen-presenting cells in the mouse. J Exp Med 172(2):567–575
Deschamps JY, Roux FA, Sai P, Gouin E (2005) History of xenotransplantation. Xenotransplantation 12(2):91–109. https://doi.org/10.1111/j.1399-3089.2004.00199.x
Murray AG, Khodadoust MM, Pober JS, Bothwell AL (1994) Porcine aortic endothelial cells activate human T cells: direct presentation of MHC antigens and costimulation by ligands for human CD2 and CD28. Immunity 1(1):57–63
Yamada K, Sachs DH, DerSimonian H (1995) Human anti-porcine xenogeneic T cell response. Evidence for allelic specificity of mixed leukocyte reaction and for both direct and indirect pathways of recognition. J Immunol 155(11):5249–5256
Cozzi E, White DJ (1995) The generation of transgenic pigs as potential organ donors for humans. Nat Med 1(9):964–966
Mollnes TE, Fiane AE (2003) Perspectives on complement in xenotransplantation. Mol Immunol 40(2–4):135–143
Adams DH, Kadner A, Chen RH, Farivar RS (2001) Human membrane cofactor protein (MCP, CD 46) protects transgenic pig hearts from hyperacute rejection in primates. Xenotransplantation 8(1):36–40
Buhler L, Yamada K, Kitamura H et al (2001) Pig kidney transplantation in baboons: anti-Gal(alpha)1-3Gal IgM alone is associated with acute humoral xenograft rejection and disseminated intravascular coagulation. Transplantation 72(11):1743–1752
Kolber-Simonds D, Lai L, Watt SR et al (2004) Production of alpha-1,3-galactosyltransferase null pigs by means of nuclear transfer with fibroblasts bearing loss of heterozygosity mutations. Proc Natl Acad Sci U S A 101(19):7335–7340. https://doi.org/10.1073/pnas.0307819101
Yamada K, Yazawa K, Shimizu A et al (2005) Marked prolongation of porcine renal xenograft survival in baboons through the use of alpha1,3-galactosyltransferase gene-knockout donors and the cotransplantation of vascularized thymic tissue. Nat Med 11(1):32–34. https://doi.org/10.1038/nm1172
Chen G, Qian H, Starzl T et al (2005) Acute rejection is associated with antibodies to non-Gal antigens in baboons using Gal-knockout pig kidneys. Nat Med 11(12):1295–1298. https://doi.org/10.1038/nm1330
Benda B, Karlsson-Parra A, Ridderstad A, Korsgren O (1996) Xenograft rejection of porcine islet-like cell clusters in immunoglobulin- or Fc-receptor gamma-deficient mice. Transplantation 62(9):1207–1211
Sandberg JO, Benda B, Lycke N, Korsgren O (1997) Xenograft rejection of porcine islet-like cell clusters in normal, interferon-gamma, and interferon-gamma receptor deficient mice. Transplantation 63(10):1446–1452
Shin JS, Kim JM, Kim JS et al (2015) Long-term control of diabetes in immunosuppressed nonhuman primates (NHP) by the transplantation of adult porcine islets. Am J Transplant 15(11):2837–2850. https://doi.org/10.1111/ajt.13345
Shin JS, Min BH, Kim JM et al (2016) Failure of transplantation tolerance induction by autologous regulatory T cells in the pig-to-non-human primate islet xenotransplantation model. Xenotransplantation 23(4):300–309. https://doi.org/10.1111/xen.12246
Zhao Y, Swenson K, Sergio JJ, Arn JS, Sachs DH, Sykes M (1996) Skin graft tolerance across a discordant xenogeneic barrier. Nat Med 2(11):1211–1216
Nikolic B, Gardner JP, Scadden DT, Arn JS, Sachs DH, Sykes M (1999) Normal development in porcine thymus grafts and specific tolerance of human T cells to porcine donor MHC. J Immunol 162(6):3402–3407
Rodriguez-Barbosa JI, Zhao Y, Barth R et al (2001) Enhanced CD4 reconstitution by grafting neonatal porcine tissue in alternative locations is associated with donor-specific tolerance and suppression of preexisting xenoreactive T cells. Transplantation 72(7):1223–1231
Haller GW, Esnaola N, Yamada K et al (1999) Thymic transplantation across an MHC class I barrier in swine. J Immunol 163(7):3785–3792
Yamada K, Shimizu A, Ierino FL et al (1999) Thymic transplantation in miniature swine. I. Development and function of the “thymokidney”. Transplantation 68(11):1684–1692
Yamada K, Shimizu A, Utsugi R et al (2000) Thymic transplantation in miniature swine. II. Induction of tolerance by transplantation of composite thymokidneys to thymectomized recipients. J Immunol 164(6):3079–3086
Yamada K, Vagefi PA, Utsugi R et al (2003) Thymic transplantation in miniature swine: III. Induction of tolerance by transplantation of composite thymokidneys across fully major histocompatibility complex-mismatched barriers. Transplantation 76(3):530–536. https://doi.org/10.1097/01.Tp.0000080608.42480.E8
LaMattina JC, Kumagai N, Barth RN et al (2002) Vascularized thymic lobe transplantation in miniature swine: I. Vascularized thymic lobe allografts support thymopoiesis. Transplantation 73(5):826–831
Kamano C, Vagefi PA, Kumagai N et al (2004) Vascularized thymic lobe transplantation in miniature swine: thymopoiesis and tolerance induction across fully MHC-mismatched barriers. Proc Natl Acad Sci U S A 101(11):3827–3832. https://doi.org/10.1073/pnas.0306666101
Nobori S, Shimizu A, Okumi M et al (2006) Thymic rejuvenation and the induction of tolerance by adult thymic grafts. Proc Natl Acad Sci U S A 103(50):19081–19086. https://doi.org/10.1073/pnas.0605159103
Postrach J, Bauer A, Schmoeckel M, Reichart B, Brenner P (2012) Heart xenotransplantation in primate models. Methods Mol Biol 885:155–168. https://doi.org/10.1007/978-1-61779-845-0_10
Tanabe T, Watanabe H, Shah JA et al (2017) Role of intrinsic (graft) versus extrinsic (host) factors in the growth of transplanted organs following allogeneic and xenogeneic transplantation. Am J Transplant Off J Am Soc Transplant Am Soc Transplant Surg 17(7):1778–1790. https://doi.org/10.1111/ajt.14210
Rivard CJ, Tanabe T, Lanaspa MA et al (2018) Upregulation of CD80 on glomerular podocytes plays an important role in development of proteinuria following pig-to-baboon xeno-renal transplantation—an experimental study. Transpl Int 31(10):1164–1177. https://doi.org/10.1111/tri.13273
Tena AA, Sachs DH, Mallard C et al (2017) Prolonged survival of pig skin on baboons after administration of pig cells expressing human CD47. Transplantation 101(2):316–321. https://doi.org/10.1097/TP.0000000000001267
Yamada K, Gianello PR, Ierino FL et al (1997) Role of the thymus in transplantation tolerance in miniature swine. I. Requirement of the thymus for rapid and stable induction of tolerance to class I-mismatched renal allografts. J Exp Med 186(4):497–506
Acknowledgments
We thank Ms. Haruna Shimizu for her editorial assistance. This research was supported by NIH grant (NIAID 5P01AI045897). All procedures and animal care were performed in accordance with the Principles of Laboratory Animal Care formulated by the National Society for Medical Research and the Guide for the Care and Use of Laboratory Animals prepared by Columbia University Medical Center.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Science+Business Media, LLC, part of Springer Nature
About this protocol
Cite this protocol
Yamada, K., Ariyoshi, Y., Pomposelli, T., Sekijima, M. (2020). Co-transplantation of Vascularized Thymic Graft with Kidney in Pig-to-Nonhuman Primates for the Induction of Tolerance Across Xenogeneic Barriers. In: Costa, C. (eds) Xenotransplantation. Methods in Molecular Biology, vol 2110. Humana, New York, NY. https://doi.org/10.1007/978-1-0716-0255-3_11
Download citation
DOI: https://doi.org/10.1007/978-1-0716-0255-3_11
Published:
Publisher Name: Humana, New York, NY
Print ISBN: 978-1-0716-0254-6
Online ISBN: 978-1-0716-0255-3
eBook Packages: Springer Protocols