Abstract
Background
Good quality sleep, regular physical activity, and limited time spent sedentary are all considered individually important in promoting good mental health in children. However, few studies have examined the influence of each behaviour simultaneously, using compositional analysis which accounts for the closed nature of the 24-h day. Our aim was to determine how compositional time use in early childhood is prospectively related to mental and psychosocial health at 5 years of age.
Methods
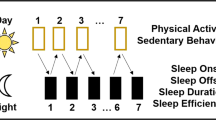
A total of 392 children wore Actical accelerometers 24-h a day for one week at 2, 3.5 and 5 years of age to examine time in sleep, physical activity, and sedentary behaviour. Psychosocial and mental health were assessed at age 5 using both laboratory based (researcher-assessed) and questionnaire (parental-report) measures. Associations were estimated using regression models with isometric log-ratios of time-use components as predictors.
Results
Cross-sectionally, 5-year old children who spent 10% (64 min) more time asleep than average had better inhibitory control (standardised mean difference [d]; 0.19; 95% confidence interal [CI]: 0.02, 0.36 for Statue test and d = 0.16; 95% CI: − 0.01, 0.33 for Heads–Toes–Knees–Shoulders task). A greater proportion of time spent active (10%, 31 min) was associated with poorer inhibitory control (d = − 0.07; 95% CI: − 0.13, − 0.02 for Statue test, d = − 0.06; 95% CI: − 0.11, − 0.01 for Heads–Toes–Knees–Shoulders task). By contrast, differences in time-use were not found to be significantly associated with any measure of self-regulation or mental health at 5 years of age, nor were any significant longitudinal relationships apparent.
Conclusions
We did not find a significant association between 24-h time use in the preschool years and any measure of psychosocial or mental health at 5 years of age, although some relationships with inhibitory control were observed cross-sectionally.
Trial registration: ClinicalTrials.gov number NCT00892983, registered 5th May 2009.
Similar content being viewed by others
Introduction
Young children require positive environments to promote the development of good mental health, to develop resilience to cope with the stresses of life, and to grow into well-rounded, healthy adults [1]. While hesitancy exists around diagnosing very young children as having mental disorders, factors like improving social competence, emotional maturity, and physical wellbeing are known to play a crucial role in bolstering mental health [2]. It is important to consider wellbeing in children holistically, often expressed as psychosocial health which refers to psychological and social factors which contribute to overall mental health. It includes protective characteristics like high self-esteem, higher resilience, greater executive functioning and ability to regulate behaviour (including inhibitory control) as well as risk factors such as anxiety, depression, hyperactivity and attentional problems [3].
Within the physical health domain, ensuring that children receive sufficient good quality sleep, maintain regular activity, and limit sedentary time are all individually important [4,5,6]. However, because time spent in one behaviour will influence time spent in the remaining behaviours across a 24-h day, researchers are increasingly examining the health effects of these movement behaviours in concert rather than in isolation [7]. As a consequence, physical activity guidelines in many countries have expanded to also address sleep and sedentary time, renamed as 24-h guidelines [8,9,10,11,12,13].
To date, little research has determined how sleep, physical activity and sedentary time interact to influence mental health in preschool-aged children, a time when they are rapidly developing. Existing cross-sectional [14,15,16] and longitudinal [17,18,19] studies demonstrate little evidence that adherence to 24-h guidelines is associated with mental health at this age. However, a limitation of assessing health outcomes in this way is that it enforces an all or nothing approach by dichotomising continuous variables (i.e. meeting the guideline or not), resulting in a loss of information [20]. An alternative is to use compositional data analysis, which accounts for the fact that any health effects of changing one behaviour (e.g. getting more sleep) might be partly due to compensatory changes in the remaining behaviours (physical activity, sedentary time), rather than an isolated effect of sleep itself [21]. To date, only two small cross-sectional studies have examined compositional time use in relation to mental health in young children, showing some inconsistency in findings [22, 23]. Given the paucity of data, particularly longitudinal data, the aim of this study was to determine how compositional time use in early childhood is related to mental health outcomes at five years of age.
Methods
This secondary analysis uses data from a randomised controlled trial of early-life obesity prevention (Prevention of Overweight in Infancy [POI] study) in Dunedin, New Zealand, consisting of a 2-year intervention (pre-natal to 2 years of age) [24] and 3-year follow-up (at 3.5 and 5 years of age) [25]. In brief, the interventions promoted the development of good sleep habits from birth (Sleep group), breastfeeding, healthy food and family activity (FAB group), or both (Combination group) in relation to Usual care. The current data have been analysed using the entire cohort with appropriate adjustment for randomisation group, as no significant differences were observed in physical activity, sedentary behaviour, or sleep following the intervention [26,27,28].
Detailed information regarding POI is available in registration documents (ClinicalTrials.gov number NCT00892983, registered 5th May 2009), study protocols [24, 25] and published findings [27, 28]. The intervention was approved by the Lower South Ethics Committee (LRS/12/08/063) and the follow-up study by the University of Otago Human Ethics Committee (12/274). Written informed consent was obtained from the parent/guardian of all child participants. We invited all mothers who had booked into the single maternity hospital (> 97% of all births) in Dunedin to participate when in the latter stages of their pregnancy. The final sample included 802 women (58% response rate) randomised to Usual care; Sleep; Food, Activity and Breastfeeding; or Combination groups. Anthropometric assessments (primary outcome) were performed by researchers blinded to group allocation. Demographic information obtained at baseline included maternal age, education, ethnicity, self-reported pre-pregnancy height and weight, and level of household deprivation. Information on infant gestational age, sex and birth weight was obtained from hospital records.
Measures obtained at 2, 3.5 and 5 years of age
Anthropometric measurements were obtained by trained measurers following standard protocols [29]. Duplicate measures of weight (Tanita WB-100 MA/WB-110 MA) and height (Harpenden stadiometer, Holtain Ltd, UK) were obtained with children wearing light clothing. Body mass index (BMI) z-scores were calculated using the World Health Organization (WHO) growth standards [30], with overweight defined as a BMI z-score ≥ 85th but < 95th percentile, and obesity as BMI ≥ 95th percentile.
Sleep, physical activity, and sedentary behaviour were assessed using Actical (Mini-Mitter, Bend, OR) accelerometers (initialized using 15 s epochs), worn by the children around the waist 24-h a day for one week. Data were scored using an automated count-scaled algorithm that estimates sleep onset (start of first 15 continuous minutes of sleep preceded by 5 min of awake) and offset (last of 15 continuous minutes of sleep followed by 5 min of awake) specific to each individual each day. Total sleep time was calculated as the difference between sleep onset and offset, excluding waking after sleep onset (WASO) as recommended [31]. Naps were determined in children at 1 and 2 years of age only defined as at least 30 min of continuous sleep, preceded by 5 min of being awake between 9am and 5 pm [32]. Awake time was divided into non-wear time (at least 20 min of consecutive zeros [33]), sedentary time (0–6 counts/15 s), light physical activity (LPA, 7–286 counts/15 s), and moderate-to-vigorous physical activity (MVPA, ≥ 287 counts/15 s) [34, 35]. We chose to use 20 min of consecutive zeros with no allowance for artifactual movement, similar to recommendations by Esliger et al. [33] and Janssen et al. [36]. Although allowing for some epochs above zero counts allows for touching or moving the accelerometer by accident and spurious spikes of accelerometer counts during non-wear without turning non-wear into sedentary time, allowing interruptions may also decrease classification accuracy [37] as well as making results vulnerable to variation in wear time if analysed with different epoch lengths [38]. As each 24-h ‘day’ was determined from the time the child woke up on day 1 to the time they woke up on day 2 (and so on), a day was considered valid if the participant had 20–28 h of data to allow for changing wake times. Participants had to have at least three valid days to be included in analyses (data from 161 children were excluded). Snoring at 3.5 and 5 years of age was adjusted for in analyses as it is one of the most common forms of sleep disturbance at this age [39], and can lead to problems with behavioural and emotional regulation [40]. Parents were asked ‘how often does your child snore loudly’ with 7 answer options ranging from ‘never’ to ‘every night’.
Measures obtained at 5 years of age only
Psychosocial factors were measured using laboratory assessment and parental report. We determined levels of inhibitory control using the ‘Statue’ component of the NeuroPSYchological Assessment (NEPSY-2) [41] and the Head-Toes-Knees-Shoulders task [42]. NEPSY-2 is a test battery that is well-normed, reliable, and appropriate for use with 5-year-old children. The Head-Toes-Knees-Shoulders task [42] is a measure of behavioural regulation and inhibition, which determines the ability of a child to follow opposing instructions (e.g. touch the head when directed to touch the toes).
Parental ratings were obtained using the Parent Rating Scale of the Behavioral Assessment System for children (BASC-2), a well-validated and normed scale [43]. We used the ‘Hyperactivity’ (11 items, Cronbach’s α = 0.79), ‘Emotional Self-Control’ (6–8 items, Cronbach’s α = 0.79), ‘Executive Functioning’ (13 items, Cronbach’s α = 0.79) and ‘Attentional Problems’ (6 items, Cronbach’s α = 0.80) subscales as measures of self-regulation, and the ‘Anxiety’ (13 items, Cronbach’s α = 0.82), Depression (11 items, Cronbach’s α = 0.77), and ‘Resilience’ (12 items, Cronbach’s α = 0.82) subscales as indicators of the child’s mental health.
Statistical analyses
Demographic characteristics were described for those with measures at 2, 3.5, or 5 years of age, and those who provided at least one measure (full analysis sample). Differences between the full analysis sample and the remaining POI participants were assessed using a independent samples t-test for continuous variables and a chi-squared test for categorical variables.
Time use components were normalised to sum to 24-h, with non-wear time first reallocated proportionally to wake-time components only (e.g. if the proportion of day-time wear is 80% sedentary and 20% PA, then 80% of the minutes of non-wear time are added to sedentary time and 20% of the minutes of non-wear time are added to PA). Non-wear time does not occur overnight so it is important that these minutes of non-wear time are not inadvertently assigned to sleep [44]. Compositional analyses were undertaken using a 3-component composition (sleep, sedentary, physical activity) because international guidelines for preschoolers focus on light-to-vigorous physical activity (LMVPA), and because most (80%) of our measurements at 5 years were obtain just prior to the child’s birthday. However, a 4-component composition (sleep, sedentary, light physical activity [LPA], and moderate-to-vigorous physical activity [MVPA]) was also undertaken for the cross-sectional analyses at 5 years, and longitudinal analyses using the 3.5 year data, based on the Level 2 Canadian guidelines for 3–4 year olds which recommend that at least 60 of the 180 min a day in LMVPA is spent in energetic play [8]. Compositional means for each component were calculated as geometric means normalised to 24 h [45]. To be able to include all co-dependent compositional variables in a regression model together, compositional data analysis (CoDA) methods were used. This involves using isometric log-ratios of the components, based on a sequential partition of one part to the remaining compositional parts [45], and including these coordinates in a linear regression model as the independent variables with the relevant outcome as the dependent variable. Models were adjusted for sex, household deprivation, randomisation group, and BMI z-score at 5 years of age, and snoring at 3.5 and 5 years of age as previously mentioned.
To report meaningful estimates of association between time-use components and mental or psychosocial health, the regression coefficient of the first isometric log-ratio coordinate (which contains the ratio of one component to all others) was back-transformed to represent the mean difference in the dependent variable for a 10% greater time spent in the component of interest relative to all others. Choosing to report associations in terms of a 10% difference is arbitrary but tends to represent a meaningful, yet still realistic difference in time-use (a 1% difference is not meaningful, while a 20% difference is less plausible). This is the most common way that associations with proportional differences are reported in studies of compositional time-use [46]. Separate regression models were generated to report estimates for each time-use component, with the isometric log-ratios calculated for different permutations of components.
Longitudinal associations between time use at 2 and 3.5 years and mental or psychosocial health at 5 years were assessed in the same way as the cross-sectional associations but without adjustment for 5-year time-use using linear regression models. All mental and psychosocial health variables were standardised so that estimates are presented in units of standard deviations. Standardised mean differences [d] and their 95% confidence intervals [CI] were calculated, estimating the mean difference for a 10% greater time in the component relative to all other components. Residuals of all regression models were plotted and visually assessed for homogeneity of variance and normality. All statistical analyses were carried out in Stata 17.0 (StataCorp, Texas).
Results
Table 1 presents characteristics of the 392 children who provided data for this study. Half of the children were boys, and two-thirds of the mothers were university educated. Included mothers were 2.8 years older than those not included (33.0 vs 30.2; p < 0.001) and were more likely to have a university degree (67.0% vs 55.5%, p < 0.001). There were no meaningful differences in maternal BMI (mean age 25.2 vs 24.9 years, p = 0.403) or infant sex (50.3% vs 52.2% male, p = 0.583) between those who were included in the study and those who were not. Time spent in sleep, sedentary behaviour, and physical activity at each age, and mean (SD) values for each of the mental and psychosocial health outcomes examined are shown in Table 1.
Table 2 presents the cross-sectional associations illustrating how 5-year-old children spend their time using a model with the three-component composition (sleep, sedentary, light-to-vigorous physical activity) in relation to the outcomes measured. These data illustrate that children who spent 10% more sleep time than average (relative to all other time-use components), corresponding to an additional 64 min a night, had better inhibitory control as measured by the Statue test (d = 0.19; 95% CI: 0.02, 0.36) and the Heads–Toes–Knees–Shoulders task (d = 0.16; 95% CI: − 0.01, 0.33). By contrast, a greater proportion of time spent physically active was associated with lower inhibitory control, whether measured by the Statue test (d = 0.07; 95% CI: − 0.13, − 0.02) or the Heads–Toes–Knees–Shoulders task (d = − 0.06; 95% CI: − 0.11, − 0.01). Differences in time-use were not meaningfully associated with any measure of self-regulation or mental health at 5 years of age.
Similar analyses were undertaken at 5 years of age using a model with the 4-part composition (physical activity divided into light PA and moderate-to-vigorous PA, Table 3). These analyses were broadly similar to those observed with the three-part composition; we observed greater inhibitory control in those who had more sleep, and the lower scores for inhibitory control seen with greater time spent physically active were entirely a result of more light PA rather than MVPA. However, some differences in mental wellbeing were observed with spending 10% more time (8.4 min) each day in MVPA; children had lower anxiety (d = − 0.05; 95% CI: − 0.09, − 0.02) and higher resilience (d = 0.05; 95% CI: 0.01, 0.08) scores, albeit by a small amount. A lower score for attentional problems (d = − 0.12; 95% CI: − 0.23, 0.00) was also observed with 10% more time spent sedentary (49 min more).
Table 4 presents the same analyses using the longitudinal data, determining how time use at 2 and 3.5 years of age was related to mental health and wellbeing outcomes at 5 years of age. As Table 4 illustrates, different proportions of time spent in sleep, physical activity, or being sedentary at 2 or 3.5 years was not significantly associated with any measure examined at 5 years of age. Longitudinal analyses were also undertaken using the 4-component model (Table 3). Small differences were observed for greater time spent in MVPA. Spending more time in MVPA at 3.5 years of age was related to higher scores for hyperactivity (0.03; 0.00, 0.06) and lower scores for executive functioning (− 0.04; − 0.06, − 0.01) at 5 years.
Discussion
Our findings show that young children who spend more time asleep have higher levels of inhibitory control, whereas children with greater levels of physical activity have lower inhibitory control, as a result of more time spent in light rather than more intense levels of activity. However, these relationships were not apparent longitudinally, with 24-h time use at 2 or 3.5 years not found to be significantly related to levels of inhibitory control, nor indeed any other measure of psychosocial or mental health at 5 years of age. Findings were broadly comparable, whether determined for the 4-part composition (examines physical activity separated into LPA and MVPA), or the 3-part composition (combines both components), with the following exceptions. Spending more time in MVPA was associated with lower anxiety and higher resilience scores cross-sectionally but also with lower executive functioning and higher hyperactivity longitudinally. Such relationships were not apparent when all categories of physical activity intensity (light, moderate, and vigorous) were combined.
Our finding that sleep was cross-sectionally related to measures of inhibitory control at 5 years of age, but that sleep at earlier ages did not predict later levels of control, fits much of the existing literature. A cross-sectional study in 3–5 year old children reported positive correlations between sleep duration and levels of inhibitory control as measured by a computerized go/no-go test [47]. Such findings have been confirmed through a meta-analysis of 86 predominantly cross-sectional studies in older (5–12 years) children demonstrating that reducing sleep duration compromised overall executive functioning, including inhibitory control [48]. By contrast, while some longitudinal studies have reported that night-time sleep at 12–18 months was proportionately related to strong impulse control at ages 2 and 4 [49, 50], others have not observed any longitudinal association with measurements taken at 4–7 and 9–16 years [51]. However, experimental research has demonstrated extending sleep by just half an hour a night enhances attention and inhibition in children, at least in the short term [52]. Overall, it would seem that sufficient levels of sleep, independent of sedentary time and physical activity, are advantageous for the development of appropriate inhibitory control in young children. However, it should be acknowledged that the differences observed were small, with wide CIs.
Our results also indicate an association between greater physical activity and lower inhibitory control in 5 year olds as a result of more time spent in light activity. These results, although complex, potentially occur because light activity may not be challenging enough to stimulate inhibition skills. Current literature suggests there needs to be an increment in task difficulty in order to improve cognitive functioning [53], and it seems likely that light activity does not produce the same benefit. Previous research in adolescents supports this view showing that light activity predicted lower performance on cognitive tasks whereas MVPA was associated with greater executive functioning [54]. Our study reports the same trends in children at 5 years of age. In line with other findings [55], we also found that higher time spent in MVPA was associated with lower anxiety and greater resilience. Finally, our finding that higher MVPA was associated with higher scores for hyperactivity is similar to other longitudinal studies [56, 57]. As these researchers highlight, there is potential for residual confounding and the possibility that some hyperactive symptoms appear as MVPA. The latter could also help explain the association between MVPA and lower executive functioning, given that this subscale contains five of the items also found within the hyperactivity subscale. Alternatively, variation in findings is possible due to the use of different cutpoints in the literature for delineating intensity of activity, which may have influenced the relationships observed.
Our study has several strengths including the relatively large sample size and longitudinal study design. We also measured 24-h time use with acceleromety rather than a mixture of measures, which has frequently been used in the compositional analysis literature to date. The use of 24-h accelerometry limits the amount of missing (or overlapping) data, problems that arise particularly when multiple methods are combined to assess 24-h time use. Our study had repeat measures of time use, allowing us to examine predictive relationships between time use and psychosocial health over an important stage of development. We also had both questionnaire and objective outcome measures; parental-report providing an overview of ‘usual’ psychosocial health, and laboratory-based assessments providing an objective and independent assessment, albeit only for a snapshot in time.
Our study also had some limitations. Only 392 of the original 802 (49%) children had sufficient data to be included in these analyses. However, this remains a substantial sample size and while there were some slight demographic differences between those who were included and those who were lost to follow-up, these were included as covariates in the models. As some participants did not complete accelerometry at every age, the samples analysed at each age also differed slightly—although demographically they were similar. While there was high variance in the outcome variables, the analysis sample is unlikely to be representative of the New Zealand population and associations could differ by demographic or at-risk groups.
Conclusions
We found no evidence that variation in 24-h time use in preschoolers is associated longitudinally or cross-sectionally with any measure of self-regulation or psychosocial health at 5 years of age. Children who spend more time in sleep and those who spend less time being physically active, did show higher levels of inhibitory control, but differences were small. Our findings support a number of studies that have investigated this question in a different way, by examining adherence to 24-h guidelines in relation to mental health, which have also demonstrated little evidence of any relationship in pre-schoolers [14,15,16,17,18,19]. While absence of evidence is not the same as evidence of absence, the data to date demonstrate little support for the presence of meaningful relationships. Perhaps the discrepancy between literature examining the association with a single one of these behaviours in relation to mental health (which often supports a link) may be at least in part explained by the fact that examining any one behaviour (e.g. sleep) ignores the dependence on the remaining behaviours (physical activity, sedentary time); only compositional analyses can account for this correctly [21].
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- MVPA:
-
Moderate-to-vigorous physical activity
- POI:
-
Prevention of Overweight in Infancy study
- BMI:
-
Body mass index
- WHO:
-
World Health Organisation
- WASO:
-
Wake after sleep onset
- NEPSY-2:
-
NeuroPSYchological Assessment
- BASC-2:
-
Behavioral Assessment System for Children
References
Mental health: a state of well-being. http://www.who.int/features/factfiles/mental_health/en/.
Frydenberg E, Deans J, Liang R. Promoting well-being in the pre-school years. Research, applications and strategies. Oxfordshire: Routledge; 2020.
Thomas K, Nilsson E, Festin K, Henriksson P, Lowén M, Löf M, Kirstenson M. Associations of psychosocial factors with multiple health behaviors: a population-based study of middle-aged men and women. Int J Environ Res Pub Health. 2020;17:1239.
Chaput JP, Gray CE, Poitras VJ, Carson V, Gruber R, Olds TS, Weiss SK, Gorber SC, Kho ME, Sampson M, et al. Systematic review of the relationships between sleep duration and health indicators in school-aged children and youth. Appl Physiol Nutr Metab. 2016;41:S266–82.
Lubans D, Richards J, Hillman C, Faulkner G, Beauchamp M, Nilsson M, Kelly P, Smith J, Raine L, Biddle S. Physical activity for cognitive and mental health in youth: a systematic review of mechanisms. Pediatrics. 2016;138: e20161642.
Tremblay MS, LeBlanc AG, Kho ME, Saunders TJ, Larouche R, Colley RC, Goldfield G, Connor GS. Systematic review of sedentary behaviour and health indicators in school-aged children and youth. Int J Behav Nutr Phys Act. 2011;8:98.
Rollo S, Antsygina O, Tremblay MS. The whole day matters: understanding 24-hour movement guideline adherence and relationships with health indicators across the lifespan. J Sport Health Sci. 2020;9:493–510.
Tremblay MS, Carson V, Chaput JP, Adamo KB, Aubert S, Choquette L, et al. Canadian 24-hour movement guidelines for the early years (0–4 years): an integration of physical activity, sedentary behavior, and sleep. BMC Pub Health. 2017;17:874.
Australian 24-hour movement guidelines for the early years (birth to 5 years): an integration of physical activity, sedentary behaviour, and sleep. https://www1.health.gov.au/internet/main/publishing.nsf/Content/npra-0-5yrs-brochure.
Sit less, move more, sleep well: active play guidelines for under-fives. https://www.health.govt.nz/publication/sit-less-move-more-sleep-well-active-play-guidelines-under-fives.
Jurakic D, Pedisic Z. Croatian 24-hour guidelines for physical activity, sedentary behaviour, and sleep: a proposal based on a systematic review of literature. Medicus. 2019;28:143–53.
Guidelines on physical activity, sedentary behaviour and sleep for children under 5 years of age. http://www.who.int/iris/handle/10665/311664.
Draper CE, Tomaz SA, Beirsteker L, Cook CJ, Couper J, de Milander M, Flynn K, Giese S, Krog S, Lambert EV, et al. The south African 24-hour movement guidelines for birth to 5 years: an integration of physical activity, sitting behavior, screen time, and sleep. J Phys Act Health. 2020;17:109–19.
Cliff DP, McNeill J, Vella SA, Howard SJ, Santos R, Batterham M, Melhuish E, Okely AD, de Rosnay M. Adherence to 24-hour movement guidelines foer the early years and associations with social-cognitive development among Australian preschool children. BMC Pub Health. 2017;17:857.
Carson V, Ezeugwu VE, Tamana SK, Chjikuma J, Lefebvre DL, Azad MB, Moraes TJ, Subbarao P, Becker AB, Turvey SE, et al. Associations between meeting the Canadian 24-hour movement guidelines for the early years and behavioral and emotional problems among 3-year-olds. J Sci Med Sport. 2019;22:797–802.
Chia MYH, Tay LY, Chua TBK. Quality of life and meeting 24-h WHO guidelines among preschool children in Singapore. Early Child Educ J. 2020;48:313–23.
McNeill J, Howard SJ, Vella SA, Cliff DP. Compliance with the 24-Hour movement guidelines for the early years: cross-sectional and longitudinal associations with executive function and psychosocial health in preschool children. J Sci Med Sport. 2020;23:846–53.
Hinkley T, Timperio A, Watson A, Duckham RL, Okely AD, Cliff DP, Carver A, Hesketh KD. Prospective associations with physiological, psychosocial and educational outcomes of meeting Australian 24-hour movement guidelines for the early years. Int J Behav Nutr Phys Act. 2020;17:36.
Taylor RW, Haszard JJ, Healey D, Meredith-Jones KA, Taylor BJ, Galland BC. Adherence to 24-hour movement behavior guidelines and psychosocial functioning in young children: a longitudinal analysis. Int J Behav Nutr Phys Act. 2021;18:110.
Altman DG, Royston P. The cost of dichotomising continuous variables. BMJ. 2006;332:1080.
Dumuid D, Pedisic Z, Palarea-Albaladejo J, Martin-Fernandez J-A, Hron K, Olds T. Compositional data analysis in time-use epidemiology: what, why, how. Int J Environ Res Public Health. 2020;17:2220.
Bezerra TA, Clark CCT, Filho ANDS, Fortes LDS, Mota JAPS, Duncan MJ, Martins CMDL. 24-hour movement behaviour and executive function in preschoolers: a compositional and isotemporal reallocation analysis. Eur J Sport Sci. 2021;21:1064–72.
Kuzik N, Naylor P-J, Spence JC, Carson V. Movement behaviors and physical, cognitive, and social-emotional development in preschool-aged children: cross-sectional associations using compositional analyses. PLoS ONE. 2020;15: e0237945.
Taylor BJ, Heath A-L, Galland BC, Gray AR, Lawrence JA, Sayers RM, Dale K, Coppell KJ, Taylor RW. Prevention of Overweight in Infancy (POI.nz) study: a randomised controlled trial of sleep, food and activity interventions for preventing overweight from birth. BMC Public Health. 2011;11:942.
Taylor RW, Heath A-LM, Galland BC, Cameron SL, Lawrence JA, Gray AR, Tannock GW, Lawley B, Healey D, Sayers RM, et al. Three-year follow-up of a randomised controlled trial to reduce excessive weight gain in the first two years of life: protocol for the POI follow-up study. BMC Pub Health. 2016;16:771.
Moir C, Meredith-Jones K, Taylor BJ, Gray AR, Heath A-LM, Dale K, Galland BC, Lawrence JA, Sayers RM, Taylor RW. Early intervention to encourage physical activity in infants and toddlers: an RCT. Med Sci Sports Exerc. 2016;48:2246–453.
Taylor BJ, Gray AR, Galland BC, Heath A-L, Lawrence JA, Sayers RM, Cameron SL, Hanna M, Dale K, Coppell KJ, Taylor RW. Targeting sleep, food, and activity in infants for obesity prevention: an RCT. Pediatrics. 2017;139: e20162037.
Taylor RW, Gray AR, Heath ALM, Galland BC, Lawrence JA, Sayers RM, Healey D, Tannock GW, Meredith-Jones K, Hanna M, et al. Sleep, nutrition and physical activity interventions to prevent obesity in infancy: follow-up of the POI randomized controlled trial at 3.5 & 5 years. Am J Clin Nutr. 2018;108:228–36.
de Onis M, Onyango AW, Van den Broeck J, Chumlea WC, Martorell R. Measurement and standardization protocols for anthropometry used in the construction of a new international growth reference. Food Nutr Bull. 2004;25:S27-36.
World Health Organization. WHO Child Growth Standards based on length/height, weight and age. Acta Paediatr Suppl. 2006;450:76–85.
Meltzer LJ, Montgomery-Downs HE, Insana SP, Walsh CM. Use of actigraphy for assessment in pediatric sleep research. Sleep Med Rev. 2012;16:463–75.
Meredith-Jones K, Williams SM, Galland BC, Kennedy G, Taylor RW. 24Hr accelerometry: impact of sleep-screening methods on estimates of physical activity and sedentary time. J Sport Sci. 2016;34:679–85.
Esliger DW, Copeland JL, Barnes JD, Tremblay MS. Standardizing and optimizing the use of accelerometer data for free-living physical activity monitoring. J Phys Act Health. 2005;2:366–83.
Adolph A, Puyau M, Vohra F, Nicklas T, Zakeri I, Butte NF. Validation of uniaxial and triaxial accelerometers for the assessment of physical activity in children. J Phys Act Health. 2012;9:944–53.
Janssen X, Cliff DP, Reilly JJ, Hinkley T, Jones R, Batterham M, Ekelund U, Brage S, Okely AD. Evaluation of actical equations and thresholds to predict physical activity intensity in young children. Phys Act Health. 2015;33:498–506.
Janssen X, Basterfield L, Parkinson KN, Pearce MS, Reilly JK, Adamson AJ, Reilly JJ, The Gateshead Millenium Study Core Team. Objective measurement of sedentary behavior: impact of non-wear time rules on changes in sedentary time. BMJ Public Health. 2015;15:504.
Peeters G, van Gellecum Y, Ryde G, Farias NA, Brown WJ. Is the pain of activity log-books worth the gain in precision when distinguishing wear and non-wear time for tri-axial accelerometers? J Sci Med Sport. 2013;16:515–9.
Banda JA, Haydel KF, Davlia T, Desai M, Bryson S, Haskell WL, Matheson D, Robinson TN. Effects of varying epoch lengths, wear time algorithms, and activity cut-points on estimates of child sedentary behavior and physical activity from accelerometer data. PLoS ONE. 2016;11:30150534.
Bonuck KA, Chervin RD, Cole TJ, Emond A, Henderson J, Xu L, Freeman K. Prevalence and persistence of sleep disordered breathing symptoms in young children: a 6-year population-based cohort study. Sleep. 2011;34:875–84.
Beebe DW. Neurobehavioral morbidity associated with disordered breathing during sleep in children: a comprehensive review. Sleep. 2006;29:1115–34.
Korkman M, Kirk U, Kemp S. NEPSY—Second Edition (NEPSY—II). San Antonio: Pearson Education; 2007.
McClelland MM, Cameron CE. Self-regulation in early childhood: improving conceptual clarity and developing ecologically valid measures. Child Dev Perspect. 2012;6:136–42.
Reynolds CR, Kamphaus RW. BASC-2: behavior assessment system for children. 2nd ed. Bloomington, MN: Pearson Assessments; 2004.
Haszard JJ, Meredith-Jones K, Farmer V, Williams SM, Galland BC, Taylor RW. Non-wear time and presentation of compositional 24-hour time-use analyses influence conclusions about sleep and body mass index in children. J Measure Hum Behav. 2020. https://doi.org/10.1123/jmpb.2019-0048.
Chastain SF, Palarea-Albaladejo J, Dontje ML, Skelton DA. Combined effects of time spent in physical activity, sedentary be- haviors and sleep on obesity and cardio-metabolic health markers: a novel compositional data analysis approach. PLoS ONE. 2015;10: e0139984.
Dumuid D, Stanford TE, Martin-Fernandez J-A, Pedisic Z, Maher CA, Lewis LK, Hron K, Katzmarzyk PT, Chaput JP, Fogelholm M, et al. Compositional data analysis for physical activity, sedentary time and sleep research. Stat Methods Med Res. 2017. https://doi.org/10.1177/09062280217710835.
Lam JC, Mahone EM, Mason T, Scharf SM. The effects of napping on cognitive function in preschoolers. J Develop Behav Pediatr. 2011;32:90–7.
Astill RG, Van der Heijden KB, Van Ijzendoorn MH, Van Someren EJ. Sleep, cognition, and behavioral problems in school-age children: a century of research meta-analyzed. Psychol Bull. 2012;138:1109–38.
Bernier A, Beauchamp MH, Bouvette-Turcot AA, Carlson SM, Carrier J. Sleep and cognition in the preschool years: specific links to executive functioning. Child Dev. 2013;84:1542–53.
Bernier A, Carlson SM, Bordeleau S, Carrier J. Relations between physiological and cognitive regulatory systems: infant sleep regulation and subsequen executive functioning. Child Dev. 2010;81:1739–52.
Friedman NP, Corley RP, Hewitt JK, Wright KP. Individual differences in childhood sleep problems predict later cognitive executive control. Sleep. 2009;32:323–33.
Sadeh A, Gruber R, Raviv A. The effects of sleep restriction and extension on school-age children: what a difference an hour makes. Child Dev. 2003;72:444–55.
Diamond A, Lee K. Interventions shown to aid executive function development in children 4 to 12 years old. Science. 2011;333:959–64.
Booth JN, Tomporowski PD, Boyle JM, Ness AR, Joinson C, Leary SD, Reilly JJ. Associations between executive attention and objectively measured physical activity in adolescence: findings from ALSPAC, a UK cohort. Mental Health Phys Act. 2013;6:212–9.
Larun L, Nordheim LV, Ekelund E, Hagen KB, Heian F. Exercise in prevention and treatment of anxiety and depression among children and young people. Cochrane Data Sys Rev. 2006. https://doi.org/10.1002/14651858.cd004691.pub2.
Ahn JV, Sera F, Cummins S, Flouri E. Associations between objectively measured physical activity and later mental health outcomes in children: findings from the UK Millennium Cohort Study. J Epidemiol Comm Health. 2018;72:94–100.
Wiles NJ, Jones GT, Haase AM, Lawlor DA, Macfarlane GJ, Lewis G. Physical activity and emotional problems amongst adolescents. Soc Psychiatry Psychiatr Epidemiol. 2008;43:765–72.
Acknowledgements
We are grateful to all the families who participated in the POI study, and to the POI research staff in the Departments of Women’s and Children’s Health, and Medicine at the University of Otago.
Funding
The POI Study was funded by the Health Research Council of New Zealand (08/374, 12/281, 12/310) and the Southern District Health Board. RWT is supported by a Fellowship from Karitane Products Society. The funding source had no role in the design and conduct of the study; collection, management, analysis, or interpretation of the data; preparation, review, or approval of the manuscript; or the decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Contributions
RWT and BJT are Principal Investigators of POI and designed the project along with KM-J, AAA, BCG, A-LMH and DH; RWT conceived the idea for this study; KMJ undertook the accelerometry analyses; JJH designed and undertook the statistical analyses; RWT wrote the first and subsequent drafts of the manuscript and all authors critically revised the manuscript for important intellectual content. RWT had primary responsibility for final content. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The original intervention to 2 years of age was approved by the Lower South Ethics Committee (LRS/12/08/063) and the follow-up study by the University of Otago Human Ethics Committee (12/274). Written informed consent was obtained from the parent/guardian of all child participants.
Consent for publication
Not applicable.
Competing interests
The authors declare they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Taylor, R.W., Haszard, J.J., Meredith-Jones, K.A. et al. Associations between activity, sedentary and sleep behaviours and psychosocial health in young children: a longitudinal compositional time-use study. JASSB 2, 3 (2023). https://doi.org/10.1186/s44167-022-00011-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s44167-022-00011-3