Abstract
Background
Obstructive sleep apnea (OSA) and metabolic syndrome (MetS) are two diseases associated with an increased risk of cardio-metabolic complications and both share the same risk factors such as obesity and smoking.
Objectives
To study the clinical features and predictors of MetS in OSA patients.
Methodology
A cross-sectional study was conducted in the sleep lab of the Pulmonology Department at Kasr Al-Ainy Hospital, Cairo University, during the period from September 2022 to March 2023. Eighty OSA patients were included, and each patient was subjected to history taking, body measurements, blood pressure measurements, Epworth sleepiness scale, STOP-BANG score, polysomnography, and laboratory investigations including lipid profile and (HBA1C), MetS was defined based on the International Diabetes Federation (IDF) guidelines. Then patients were classified into two groups; OSA with MetS and OSA without MetS, we compared both groups using a one-way (ANOVA) test.
Results
MetS was diagnosed in 66.3% of the study group. OSA with MetS had higher BMI (44.76 ± 9.55) with significant p values (< 0.001), lower average O2 saturation % (90.23 ± 5.5, p value = 0.013), and longer SPO2 time < 90% (37.39 ± 34.14, p value = 0.034) than the other group. BMI, waist, hip, and neck circumferences and SPO2 < 90% were predictors of MetS among OSA patients with significant p values. Females had significantly higher BMI (46.64 ± 9.58), p value = 0.015. Males had significantly higher AHI than females (32.99 ± 24.02 versus 19.83 ± 14.74 respectively), p value = 0.031.
Conclusion
MetS was diagnosed in 66.3% of OSA. BMI, neck, hip, waist circumferences, and SPO2 < 90% were predictors of MetS among OSA.
Trial registration
Retrospectively registered, date of registration is 18/09/2023, and number of registration is NCT06051097. The link to the study on clinicaltrials.gov.
Similar content being viewed by others
Background
Obstructive sleep apnea (OSA) is a common disorder that is marked by repeated upper airway obstruction during sleep resulting in apneas and hypopneas [1]. Previous studies have linked OSA to an increased risk of type 2 diabetes mellitus, hypertension, stroke, and other cardiovascular diseases. The risk of OSA is increasing with the increased prevalence of obesity and is estimated to be 17% among adults [2].
Metabolic syndrome (MetS) is a combination of central obesity, hypertension, hyperglycemia, and dyslipidemia. The prevalence of metabolic syndrome ranges from 20 to 40% all over the world with a tendency to increase proportionately with the increase in the prevalence of obesity. Previous studies found that Obesity was strongly linked to MetS and a well-established risk factor for OSA. They noticed that as the prevalence of obesity is rising, the link between OSA and MetS has become increasingly apparent, this is important because the coexistence of the two disorders within the same patient can increase the potential for complications such as cardiovascular events [3].
So, the aim of our study was to assess the prevalence of MetS among patients with OSA and to study clinical features and predictors of MetS in OSA patients.
Methodology
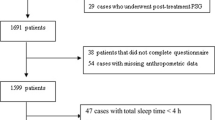
The present study is a cross-sectional study. It was conducted in the sleep lab unit of the pulmonology department at Kasr Al-Ainy Hospital, Faculty of Medicine, Cairo University during the period from September 2022 to March 2023. The study was approved by the research ethical committee of Cairo University (code: MS-258-2022). Patients were recruited from inpatient or outpatient clinics, 102 patients were referred to a sleep lab for symptoms suggestive of OSA, 22 patients were excluded from the study (15 patients did not fulfill diagnostic criteria of OSA and 7 patients refused to participate in the study). Eighty OSA patients were finally registered for the current study.
Inclusion criteria
All patients above 18 years of both sexes who fulfilled the OSA diagnostic criteria based on the American Academy of Sleep Medicine Guidelines 2014 [4].
Exclusion criteria
Patients with cerebrovascular accident within the preceding 30 days, patients on sedatives and antipsychotics.
All patients were interviewed using structured questionnaires which included OSA symptoms, history of smoking and alcohol consumption, history of diabetes, hypertension, and drug history including anti-diabetics, anti-hypertensives, and lipid-lowering medications. Clinical examination was performed with special emphasis on body measurements (neck, hip, and waist circumferences in cm), BMI in kg/m2, and measurement of blood pressure. Assessment of daytime sleepiness was done using the Epworth sleepiness scale (ESS) and STOP-BANG questionnaire. Overnight polysomnography study with detailed analysis of the recorded data using Medicom-MTD, Model: Encephalan-EEGR-19/26) screen TM plus (cardio-respiratory screening) which is a computer-based high technology polysomnography. The following data could be obtained from the recording; Apnea hypopnea index (AHI) is the total number of apneas and hypopneas/hour of sleep, respiratory disturbance index (RDI) is the number of apneas, hypopneas plus RERAs (respiratory effort related arousals). Arrhythmia index is the events of cardiac arrhythmias/hour of sleep. The oxygen desaturation index is the sum of desaturations/sleep hour. Oxygen desaturation is defined as a decrease in the mean oxygen saturation of ≥ 4% that exists for a minimum of 10 s. SPO2 time < 90% is the duration during which O2 saturation percent is below 90% measured as % from total sleep time. Obstructive sleep apnea was defined based on the American Academy of Sleep Medicine Guidelines 2014 [4], The severity of OSA will be assessed by AHI values, patients with AHI ≥ 5 and < 15 are considered mild, AHI ≥ 15 and < 30 are considered moderate and AHI ≥ 30 are considered severe. Based on the International Diabetes Federation (IDF) the diagnosis of MetS is considered if a patient has central obesity (waist circumference ≥ 90 cm for men and ≥ 80 cm for women, with ethnicity-specific values, assumed if BMI is > 30 kg/m2), plus any two of the following four factors: (a) raised triglycerides (≥ 150 mg/dL) or specific treatment for this lipid abnormality; (b) reduced HDL cholesterol (< 40 mg/dL in males, < 50 mg/dL in females) or specific treatment for this lipid abnormality; (c) raised blood pressure (blood pressure ≥ 130/85 mmHg) or treatment of previously identified hypertension; and (d) raised fasting plasma glucose (≥ 100 mg/dL) or previously diagnosed type 2 DM [5]. Patients were classified based on a concomitant diagnosis of MetS into two groups: OAS with MetS and OSA without MetS.
Statistical analysis
Analysis of data was performed using SPSS for Windows version 23 for statistical analysis. The description of variables was presented as follows: the description of quantitative variables was described as mean, standard deviation (SD), minimum, and maximum. Description of qualitative variables was described as numbers (No.) and percentages (%). Data was explored for normality using the Kolmogorov-Smirnov test of normality. Parametric tests were used for most of the comparisons. Comparison between quantitative variables was carried out by one-way analysis of variance (ANOVA) to test the difference between the means of several subgroups of a variable.
Relation between qualitative variables was carried out by Chi-squared test to determine the relationship between two or more classification factors. The binary correlation was carried out by the Pearson correlation test. Results were expressed in the form of correlation coefficient(R) and P values. The significance of the results was assessed in the form of a P value that is differentiated into: Non-significant when P value > 0.05, significant when P value ≤ 0.05, and highly significant when P value ≤ 0.01. ROC curve was constructed with the area under curve analysis performed to detect the best cut-off values of BMI and other variables for detection of MetS in OSA. The best cut-off value of each variable was chosen according to the highest Youden index.
Results
The current study involved 80 OSA patients, 33 males (41%) and 47 females (59%) with a mean age of 53 ± 12. History of diabetes was found in 27.5%, hypertension in 45%, and ischemic heart disease in 31%. Regarding OSA severity based on AHI, 40% of the study group had mild OSA, 32.5% had moderate and 27.5% had severe disease. The study group was classified according to concomitant diagnosis of metabolic syndrome (MetS) into two groups; OSA with MetS included 53 patients ( 66.3%) and OSA without MetS included 27 patients (33.7%). There is no age difference between the two groups, OSA patients with MetS had higher waist, neck, and hip circumferences and higher BMI with significant p values (0.001, 0.022, 0.023, and < 0.001 respectively). Laboratory tests revealed elevated LDL, total cholesterol, and triglycerides values (p values < 0.001), decreased HDL level (p value < 0.001), and elevated HB A1c (p value 0.001) in OSA patients with MetS than OSA without MetS (Table 1). Regarding polysomnographic findings, OSA patients with MetS had significantly lower average O2 saturation % (90.23 ± 5.5, p value = 0.013) and longer SPO2 time < 90% (37.39 ± 34.14, p value = 0.034). AHI, RDI, arrhythmia index, desaturation index, and minimal saturation show insignificant differences between both groups. STOP-BANG questionnaire was statistically higher in OSA with MetS (4.77 ± 1.51, p value = 0.049), while ESS shows an insignificant difference between the two groups (Table 1). It was found that 67.9% of OSA with MetS were females and 32.1% were males while in OSA without MetS 40.7% were female and 59.3% were males with a significant p value of 0.02, 20% of OSA patients with MetS were diabetics, 31% were hypertensive and 22% were known to have ischemic heart disease which was significantly higher than OSA patients without MetS (p value 0.004, 0.001, and 0.006 respectively), we did not find a significant difference between both groups regarding the smoking history and OSA severity (Table 2).
It was found that BMI was a predictor that can be used for the detection of MetS among OSA patients with a cut-off value equal to 38 kg/m2, sensitivity was 84.9%, specificity was 66.7% and p value < 0.001, other predictors of MetS in OSA patients were waist, hip and neck circumferences with cut-off values 134, 142, and 46 cm and p values < 0.001, 0.006 and 0.008 respectively. Regarding polysomnographic data, SPO2 < 90% can detect MetS in OSA patients with a cut-off value of 23% (as a % of total sleep time) with p value = 0.024, specificity = 74%, and low sensitivity = 54.7% (Table 3 and Fig. 1). We further subdivided the OSA group with MetS into two groups based on the sex; 17 males (32.1%) and 36 females (67.9%). It was noticed that females had significantly higher BMI (46.64 ± 9.58) versus (40.78 ± 8.42) for males, p value = 0.015, and higher HBA1C values 7.42 ± 1.3 g/dl versus 6.66 ± 1.17 for males with p value = 0.047. Males had statistically significantly higher AHI than females (32.99 ± 24.02 versus 19.83 ± 14.74 respectively) with p value = 0.031 (Table 4). All males were current smokers and all females were non-smokers, p value < 0.001. Comparison between males and females regarding OSA severity revealed that most males had moderate and severe disease (47% and 35% respectively), while 52.8% of females had mild disease with significant p value = 0.043 (Fig. 2).
Discussion
The current study included 80 participants fulfilling the diagnosis of OSA. It was found that 66.3% of the study group had a concomitant diagnosis of MetS. It was noticed that 67.9% of OSA with MetS were females and 32.1% were males. This was matched with the results of recent studies which found that the prevalence of MetS among OSA patients ranged from 72.7 to 80% and female patients with OSA had a significantly higher percentage of metabolic syndrome than males [6, 7].
The current study demonstrated that OSA patients with MetS had significantly higher BMI, waist, hip, and neck circumferences than OSA without MetS, these results agreed with previous studies which proved the strong association between large waist and neck circumferences and MetS in OSA patients [7,8,9].
Previous research found that BMI was higher in OSA patients than in the control group and suggested that obesity was the primary determinant of metabolic syndrome in those patients rather than sleep apnea [10]. More recent studies have raised the possibility of a significant association between MetS and high BMI [11, 12]. So, researchers suggest that obesity is strongly linked to MetS and is a well-recognized risk factor for OSA. So, as the prevalence of obesity increases the association between MetS and OSA becomes more apparent [13].
Moreover, one of the interesting results of the current study was that BMI could be considered a good tool to detect MetS among the study population by using the ROC curve, with a cut-off value of 38 kg/m2, sensitivity of 84.9%, and specificity of 66.7%. This agrees with a previous study which reported that BMI was a predictive factor for the occurrence of MetS in OSA patients [13].
We found that waist circumference with a cut-off value = 134 (which is higher than IDF diagnostic criteria of MetS) can be used for the detection of MetS in OSA with a significant p value, a sensitivity of 56.6%, and a specificity of 85.2%, which is agreed with a previous study which revealed that age and waist circumference are predictors of MetS and OSA [14].
One study found that neck circumference with a cut-off value of 38 cm had a sensitivity of 54% and a specificity of 70% in predicting the presence of metabolic syndrome, they concluded that neck circumference should be considered in the definition of MetS but it should be validated with larger studies [15]. This was matched with our findings; however, we found a higher cut-off value of neck circumference (46 cm) with a higher specificity of 81.5% in detecting MetS in our study group.
In the current study, we found that hip circumference with cut-off value of 142 cm and a specificity of 88% can be used for the detection of MetS in OSA, and from the polysomnographic data the only variable that can be used for the prediction of MetS was the SPO2 < 90% with cut-off value of 23%, sensitivity of 54.7%, and specificity of 74.1%.
It was noticed that LDL, total cholesterol, triglycerides, and HB A1c values were significantly elevated, while HDL level was significantly decreased in OSA patients with MetS than in OSA without MetS. We found that OSA patients with MetS had a significant increase in co-morbid conditions such as diabetes, hypertension, and ischemic heart disease (p value 0.004, 0.001, and 0.006 respectively). Oxygen indices in polysomnography revealed that OSA patients with MetS had significantly lower average O2 saturation % and spent more time with SPO2 time < 90% (as % from total sleep time).
There is clear evidence that repeated upper airway obstructive events can lead to repeated arousal, sympathetic activation, and intermittent hypoxia which results in tissue ischemia, release of oxygen free radicals, oxidative stress, cytokine production, and finally low-grade systemic inflammation. These pathologic mechanisms are responsible for the development of atherosclerosis, cardiovascular accidents, glucose intolerance, systemic hypertension, dyslipidemia, and MetS [16,17,18].
In the current study, there was no significant difference between both groups as regards AHI, RDI, or OSA severity, this was not matched with a previous study which found that MetS was positively correlated with AHI. This difference could be related to gender differences in the OSA with MetS group between both studies, as 59% of their patients were males while most of our patients were females 67.9%. It is well known that female patients presented with less severe OSA in terms of AHI than males [19, 20].
We then further classify OSA with MetS group into two subdivisions based on sex. It was noticed that females had significantly higher BMI and HBA1C than males, while males had significantly higher AHI. Regarding OSA severity it was found that most males had moderate and severe disease (47% and 35% respectively), while 52.8% of females had mild disease with a significant p value.
Previous studies found that females with OSA were more obese and had less severe disease as indexed by AHI [7, 20,21,22,23].
This discrepancy between high BMI and less severe OSA in females could be explained by different pathophysiological mechanisms underlying this situation. For example, one study confirmed that males had longer upper airways and larger soft palate than females, they concluded that airway collapsibility is more prominent in males than females [24].
Another study stated that the fat distribution was more important than BMI, it proved that males had a higher proportion of visceral and upper body fat rather than peripheral fat as in females [25].
In the current study, it was noticed that 100% of males were current smokers while all females were non-smokers. This was in line with previous research which found that smoking was a risk factor for MetS in OSA patients [26], and another research which suggested that MetS was strongly linked to smoking [11].
Smoking is known to cause inflammation and edema of the upper airway, weaken the pharyngeal muscles, and increase fat accumulation in the pharynx. So, it can increase the severity of OSA [27].
Limitations of the study
-
1)
Small number of the study group.
-
2)
Single-center study.
-
3)
We did not study the effect of weight reduction on MetS components or OSA.
-
4)
We did not study the effect of CPAP treatment on MetS components.
Conclusion
In our study, we confirmed the association of MetS and OSA and it was found that obesity was the only predictor of MetS among OSA patients. Both conditions directly increase or contribute to the development of cardiac and metabolic complications, so special attention should be given to patients with concomitant OSA and MetS for early detection and management of possible complications.
Availability of data and materials
Data from the current study is available from the corresponding author upon reasonable request.
Abbreviations
- OSA:
-
Obstructive sleep apnea
- MetS:
-
Metabolic syndrome
- HBA1C:
-
Glycosylated hemoglobin
- BMI:
-
Body mass index
- LDL:
-
Low-density lipoprotein
- HDL:
-
High-density lipoprotein
- O2:
-
Oxygen
- SpO2:
-
O2 saturation in the peripheral blood
- AHI:
-
Apnea hypopnea index
- ESS:
-
Epworth sleepiness scale
- RDI:
-
Respiratory disturbance index
- RERAs:
-
Respiratory effort-related arousals
- IDF:
-
International Diabetes Federation
- DM:
-
Diabetes mellitus
References
Slowik JM, Sankari A, Collen JF. Obstructive Sleep Apnea. 2022 Dec 11. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023. PMID: 29083619.
Yeghiazarians Y, Jneid H, Tietjens JR et al (2021) Obstructive sleep apnea and cardiovascular disease: a scientific statement from the American Heart Association. Circulation 144(3):e56–e67
Young T et al (2002) Predictors of sleep-disordered breathing in community-dwelling adults: The Sleep Heart Health Study. Arch Intern Med 162:893–900. https://doi.org/10.1001/archinte.162.8.893
American Academy of Sleep Medicine (AASM) (2014) International classification of sleep disorders, 3rd edn. American Academy of Sleep Medicine, Darien, IL
Alberti KGMM, Zimmet P, Shaw J (2006) Metabolic syndrome—a new world-wide definition. A Consensus Statement from the International Diabetes Federation. Diabet Med 23:469–480
Chaudhary P, Goyal A, Pakhare A, Goel SK, Kumar A, Reddy MA, Anoohya V (2022) Metabolic syndrome in non-obese patients with OSA: learning points of a cross-sectional study from a tertiary care hospital in Central India. Sleep Breath 26(2):681–688. https://doi.org/10.1007/s11325-021-02401-4
Negm MF, Kamel MH, Ebrahim WM et al (2022) Evaluation of obstructive sleep apnea in metabolic syndrome. Egyp J Hospital Med 88(1):3417–3422
Suryakumari V, Vulli V, Rao G et al (2018) Study of prevalence of obstructive sleep apnea in patients with metabolic syndrome. IOSR J Dent Med Sci 17:51–55
Kim D, Kim B, Han K et al (2021) The relationship between metabolic syndrome and obstructive sleep apnea syndrome: a nationwide population based study. Sci Rep 11:8751
Coughlin SR, Mawdsley L, Mugarza JA et al (2004) Obstructive sleep apnoea is independently associated with an increased prevalence of metabolic syndrome. Eur Heart J 25:735–741
Mohebbi I, Saadat S, Aghassi M et al (2012) Prevalence of metabolic syndrome in Iranian professional drivers: results from a population based study of 12,138 men. PLoS One 7(2):e31790
Shayestefar M, SadeghniiatHaghighi K et al (2019) Assessment of the relationship between metabolic syndrome and obstructive sleep apnea in male drivers of Shahroud city in 2018: a cross sectional study. BMC pub health 19(1):1–8
Lam JC, Mak JC, Ip MS (2012) Obesity, obstructive sleep apnoea and metabolic syndrome. Respirol 17:223–236. https://doi.org/10.1111/j.1440-1843.2011.02081.x
Quintas RD, Novoa MT, Pérez MT, Montero MG, Martínez ML, Velázquez PM (2011) Predictors of obstructive sleep apnea syndrome and metabolic syndrome. Europ Resp J 38:p3050
Cizza G, de Jonge L, Piaggi P, Mattingly M, Zhao X, Lucassen E, Rother KI, Sumner AE, Csako G, NIDDK Sleep Extension Study (2014) Neck circumference is a predictor of metabolic syndrome and obstructive sleep apnea in short-sleeping obese men and women. Metab Syndr Relat Disord 12(4):231–241. https://doi.org/10.1089/met.2013.0093
Song SO et al (2019) Metabolic consequences of obstructive sleep apnea especially pertaining to diabetes mellitus and insulin sensitivity. Diabetes Metab J 43:144–155. https://doi.org/10.4093/dmj.2018.0256
Lavie L, Polotsky V (2009) Cardiovascular aspects in obstructive sleep apnea syndrome–molecular issues, hypoxia and cytokine profiles. Respiration 78:361–370. https://doi.org/10.1159/000243552
Pialoux V et al (2009) Effects of exposure to intermittent hypoxia on oxidative stress and acute hypoxic ventilatory response in humans. Am J Respir Crit Care Med 180:1002–1009
Young T, Hutton R, Finn L, Badr S, Palta M (1996) The gender bias in sleep apnea diagnosis. Are women missed because they have different symptoms? Arch Intern Med 156(21):2445–2451
Assal HH, Kamal E Gender differences in polysomnographic findings in Egyptian patients with obstructive sleep apnea syndrome. Egyp J Chest Diseases Tubercul 65(32016):649–654. https://doi.org/10.1016/j.ejcdt.2016.03.009
O'Connor C, Thornley KS, Hanly PJ (2000) Gender differences in the polysomnographic features of obstructive sleep apnea. Am J Respir Crit Care Med 161(5):1465–1472. https://doi.org/10.1164/ajrccm.161.5.9904121
Alotair H, Bahammam A (2008) Gender differences in Saudi patients with obstructive sleep apnea. Sleep Breath 12(4):323–329. https://doi.org/10.1007/s11325-008-0184-8
Gabbay IE, Lavie P (2012) Age- and gender-related characteristics of obstructive sleep apnea. Sleep Breath 16(2):453–460. https://doi.org/10.1007/s11325-011-0523-z
Malhotra A, Huang Y, Fogel RB, Pillar G, Edwards JK, Kikinis R, Loring SH, White DP (2002) The male predisposition to pharyngeal collapse: importance of airway length. Am J Respir Crit Care Med 166(10):1388–1395. https://doi.org/10.1164/rccm.2112072
Harada Y, Oga T, Chihara Y, Azuma M, Murase K, Toyama Y, Aihara K, Tanizawa K, Yoshimura C, Hitomi T, Handa T, Tsuboi T, Mishima M, Chin K (2014) Differences in associations between visceral fat accumulation and obstructive sleep apnea by sex. Ann Am Thorac Soc 11(3):383–391. https://doi.org/10.1513/AnnalsATS.201306-182OC
Huang HY, Wang W, Zhou JP, Li QL, Feng WT, Wu ZZ. [Metabolic syndrome and its influencing factors in professional automobile drivers in a company] Zhonghua Lao Dong Wei Sheng Zhi Ye Bing Za Zhi. 2016;34(4):258-61. Chinese https://doi.org/10.3760/cma.j.issn.1001-9391.2016.04.005
Oțelea MR et al (2022) Smoking obstructive sleep apnea: Arguments for a distinctive phenotype and a personalized intervention. J Pers Med. https://doi.org/10.3390/jpm12020293
Acknowledgements
Not applicable.
Funding
No
Author information
Authors and Affiliations
Contributions
Safy Zahid Kaddah was responsible for the acquisition of data, analysis, drafting of the article, and final approval. Merna Hamada Korany was responsible for the acquisition of data, analysis, drafting of the article, and final approval. Eman Kamal Ibrahim was responsible for the conception and design, revising, writing, and final approval of the article.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All methods were carried in accordance with relevant regulations and guidelines, informed consent was obtained from all participants and /or their legal guardians, and the study was approved by the research ethical committee, Cairo University with IRB (code: MS-258-2022).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kaddah, S.Z., Korany, M.H. & Ibrahim, E.K. Clinical features and predictors of metabolic syndrome among obstructive sleep apnea patients. Egypt J Bronchol 18, 6 (2024). https://doi.org/10.1186/s43168-024-00259-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43168-024-00259-0