Abstract
Background
There are many physiological changes occur during pregnancy that affect oxygenation of the pregnant women. It was considered that aerobic and breathing exercises are safe for the mother and the fetus especially moderate intensity exercise during pregnancy.
Objective
This study was designed to investigate the blood oxygenation response to aerobic exercise combined with breathing exercises in pregnant women.
Methodology
Forty pregnant women were selected from obstetrics and gynecology outpatient clinic at Kasr El Einy Hospital, Egypt, confidentiality was assured. They were ranged from 25 to 30 years old, with body mass index (BMI) less than 30 kg/m2 and at the beginning of 3rd trimester, this study was conducted from September 2019 to April 2020. They were assigned into two groups: group A performed aerobic exercise in a form of walking for 20 min. On the treadmill at 60–75% of the maximum heart rate (MHR) of each woman, three times per week in addition to deep breathing exercises in form of diaphragmatic and lateral costal breathing; group B who performed deep breathing exercises only in form of diaphragmatic and lateral costal breathing. The program continued for three months, three times per week. The oxygen saturation (SaO2) was measured twice time, firstly, at the beginning of 3rd trimester of pregnancy then after three months of treatment program.
Results
The results of this study revealed a statistically significant difference in the oxygen saturation in group A than in group B.
Conclusion
It could be concluded that there was significant statistical effect of aerobic exercise combined with breathing exercises on blood oxygenation in pregnant women. It improved the oxygen saturation in pregnant women.
Similar content being viewed by others
Introduction
The normal physiological alterations that occur during pregnancy are very important for fetus survival and labor preparation. During pregnancy, the lung volumes and capacities are changed as there was enlargement of the uterus, and the diaphragm was raised about 4 cm. This leads to upward displacement of the rib cage, expanding the ribs angle with the spine [1]. These progressions expanded the lower thoracic breadth by about 2 cm and the thoracic boundary by 6 cm. During pregnancy, abdominal muscles had less tone and activity, making breath more dependent on the diaphragm. Elevation of the diaphragm was coupled with decrease in the total capacity of the lung and function residual capacity, while both tidal volume and oxygen consumption were increased (Ajne et al. 2005) [2].
Pregnancy is related with significant respiratory changes, it expands O2 utilization by 15 to 20%, a huge part of this increment is related with the necessities of the feto-placental unit, and the expanded work by the maternal organs (heart, kidneys, and lungs) (Charles et al. 2008) [3]. That expanding in the ventilation because of increase of tidal volume. This ventilation expansion is superior to increase in oxygen consumption and this brought about both hyperventilation and an expanded ventilatory comparable for oxygen (the ventilation in liters needed for every 100 mL of the consumed oxygen) [4].
Knowledge of expanded ventilation is one clarification for the feeling of dyspnea in pregnant women without cardiopulmonary restriction. Functional residual capacity diminishes and alongside the expanded oxygen consumption described, prior effects in the reduced oxygen reserve (Gabbe et al., 2007) [5].
Aerobic exercise (additionally called cardio) is a physical of generally low intensity that fundamentally depends on the aerobic energy producing process. Aerobic signifies “living in air” and refers to the utilization of oxygen to adequately satisfy energy needs during exercise through the aerobic metabolism. For the most part, activities with light-to-moderate intensities that are sufficiently supported by aerobic metabolism can be performed for elongated periods of time. The intensity ought to be in the range of 60 and 85% of the maximum training heart rate [6].
Exercise should be part of a healthy pregnancy. Walking is perhaps the most ideal approaches to obtain the heart rate up and gain the regular exercise benefits during pregnancy. The treadmill considered as a very effective and safe environment for exercising during pregnancy. The brisk walking is the best treadmill exercise that can be performed during pregnancy [7].
During pregnancy, moderate aerobic exercise has all the earmarks of being safe for both fetus and the mother and may improve some pregnancy outcomes such as preeclampsia and gestational diabetes. Pregnant women while performing moderate intensity of exercise, react distinctively contrasted with non-pregnant women. The expansion in oxygen utilization for a given remaining task at hand is more noteworthy. In pregnant women weight bearing activities, for example, treadmill walking, is related with fundamentally higher oxygen utilization than cycle ergometry contrasted with the distinction between these two modes in non-pregnant [8].
During aerobic exercise the cardiac output rises as in pregnant compared with non-pregnant ladies. This distinction is essentially because of an expansion in stroke volume. The correspondingly more prominent expansion in cardiac output with exercise brings about expanding oxygen conveyance to the fetus during maternal exercise because of increment blood stream to the lung (permitting the lung to convey more oxygen into blood) (Jensen et al. 2005) [9].
Aerobic exercise like walking or running on the treadmill presents many benefits, for the pregnant ladies with routine exercises, to get out of achieving extra weight during pregnancy and can simply go back to the pre-pregnancy weight after delivery. Exercise likewise can diminish the danger of gestational diabetes and other pregnancy-related conditions. At long last, walking or running is a great method to set up the body for process of labor (Penney, 2008) [10].
Breathing is one of the substantial processes that can be either is voluntary or involuntary. Breathing can occur automatically without considering it, or subjects can change it intentionally and freely. Considering this remarkable relationship among thinking and bodily processes, breathing pattern can assume a deciding role in how much subjects are influenced by stresses [11].
Diaphragmatic breathing encourages subjects to inhale more easily and utilize less energy. Patients with lung diseases often have enlarged lungs since air gets caught in the lungs. Diaphragmatic breathing gets the stale, trapped air out of the lungs [12].
As there are numerous physiological changes happen during pregnancy that influences the oxygenation of the pregnant women, so this study was carried out to discover the impact of the aerobic exercise combined with breathing exercises on oxygenation during pregnancy.
Participants and methods
Study design
The study was designed as a randomized controlled trial. Ethical approval was obtained from the institutional review board of the faculty of physical therapy, Cairo University by number P.T.REC/012/002499) before starting of the study and the clinical trial registration in Clinicaltrial.gov with an identifier number NCT04077931. The study was followed the Guidelines of Declaration of Helsinki on the conduct of human research.
Participants
Forty volunteers’ pregnant women at the beginning of 3rd trimester participated in this study. They were selected randomly from the obstetrics and gynecology outpatient clinic Kasr El Einy Hospital, Egypt, confidentiality was assured. Inclusion criteria of the participants in the study were as follows: their ages were ranged from 25 to 30 years, and body mass index (BMI) were less than 30 kg/m2. All participants were pregnant women at the beginning of the 3rd trimester. Exclusion criteria of the study were as follows: a participant who had pulmonary diseases, cardiovascular diseases, and psychiatric disorders.
Participants were assigned randomly used sealed envelope into two groups (A&B) equally in the number. Group A consisted of 20 pregnant women at the beginning of the 3rd trimester. They performed aerobic exercise training in the form of walking on the treadmill for 20 min, three times per week for 12 weeks. Then, they performed deep breathing exercises in form of diaphragmatic and lateral costal breathing. Group B consisted of 20 pregnant women at the beginning of the 3rd trimester who performed deep breathing exercises only in form of diaphragmatic and lateral costal breathing.
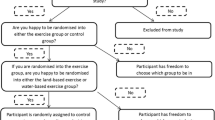
Eligibility
Forty-four women were assessed for eligibility in the present study, 4 women were excluded from our study (4 women declined to participate), and so 40 women were randomized to the study. And finally, 40 women completed the study and their data had been analyzed (Fig. 1).
Randomization
Simple randomization was done by sealed envelope as before the study started the therapist collected 40 women who met the inclusion criteria and then each one was instructed to select one of sealed envelope, there were 40 sealed envelope 20 of them contain letter (A) and 20 of them contain letter (B).
Methods
Before the start of the first session, each pregnant woman was informed about the program of exercises, and informed written consent form was signed from each woman before participation in the study. This study was conducted from September 2019 to April 2020.
Aerobic exercise for all participants in group A
Women performed aerobic exercise in a form of walking for 20 min on the treadmill three times per week for 12 weeks.
Treadmill: (power 220 V, 50/60 Hz): its speed, inclination and timer are adjustable, and it also provided with the control plane to display the exercises parameters.
Intensity of exercises
The intensity of exercises was calculated as 60–75% of her maximum heart rate (MHR) [13] as follows:
MRH (Maximum heart rate = 220 − age in years) [14].
Mode of exercises
Walking on the treadmill with fixed 0% grade inclination.
Duration of exercises
Firstly, every woman started with 5 min warming up exercises in form of stretching muscles of lower limbs and walking in places. Then, the active period started by standing on treadmill and catching the handles by her hand, so her pulse rate appears on the screen of the machine. She asked to maintain 1 min and then we pick the heart rate from the screen. She asked to start walking with the speed of the machine was adjusted at 0.8 km/h, so her resting pulse rate increases, then we increased the speed by 0.2 km/h gradually every 2 min (to give a time for adjustment of heart rate) until reaching the maximum heart rate (not less than 60% and not more than 75% of maximum heart rate). So, the intensity of exercises can be increased or decreased only by changing the speed of treadmill according to maximum heart rate [14].
Finally, each exercise session terminated with cooling down performed immediately after the active period to gradually bring HR to its pre-exercises level, in the form walking at low intensity (40% of the maximum HR) on the treadmill for 5 min.
Deep breathing exercises for all participants in group A
In the form of diaphragmatic and lateral costal breathing.
Diaphragmatic breathing exercises
-
Position of the woman: the woman assumes a relaxed comfortable position, e.g., crock lying, sitting, standing position.
-
Position of the therapist: stride standing position at the level of the waistline.
One hand of the therapist is placed on the abdomen just above the level of the waistline on horizontal position.
Technique of breathing exercises: regular aerobic exercise in a form of breathing exercises included duration of 30 min at 40–70% VO2 max, performed 2–3 times per week. Each woman practiced the deep breathing exercises for 30 min in the form of diaphragmatic breathing exercises for 15 min and lateral costal breathing exercises for 15 min, three times per week for 12 weeks. Each pregnant woman performed slow breathing six times in a minute as deep breathing exercises consisted of inspiration and expiration in a form of diaphragmatic breathing exercises and lateral costal breathing exercises in each session. Each six slow breaths per minute, as divided into (inspiration) breath in for 4 s and breath out (expiration) for 6 s. Each complete breath should last 14 s and this is repeated and performed six times. Each woman took a rest between the exercises 2 min as duration of exercises of each deep breathing exercises for 15 min [15]. The therapist asked the women to take deep inspiration from her nose, push hand upward, and then expire the air from the mouth with a sigh.
Lateral costal breathing
Position of the woman and the therapist: as before in diaphragmatic breathing, and as technique of breathing exercises. Both hands of the therapist placed laterally on the chest wall with the finger fanning to take the shape of the chest and both thumbs directly upward [15].
The therapist asked the women to take deep inspiration from the nose, open out ribs, push hand laterally, and then expire the air from the mouth with a sigh
Group B (control group)
Women in the group B performed deep breathing exercises only in the form of diaphragmatic and lateral costal breathing exercises as described for group A.
Outcome measures
The assessment of the participants in the two groups (A and B) was done before, after the end of the treatment program by the measurement of oxygen saturation (SaO2) through the pulse oxymeter.
Pulse oxymeter
It was used to measure oxygen saturation (SaO2) on the right index of everyone. Each individual sits quietly for about 5 min before the measurement and sits silently during the measurement. After placing the sensor of the oxymeter on the index finger, the pregnant woman asked to wait until a reading registered on the oxymeter display, also she was asked to wait for another 15 s until verifying a steady signal. The Pulse oxymeter begins to record SaO2 and pulse rate every 10 s. Six observations were recorded, and their mean used as the individual's SaO2 [15].
Statistical analysis
Results were expressed as mean ± standard deviation (SD). Paired t test was used to compare between the “pre” and “post” tests for blood oxygenation at each tested group. Independent t test was conducted to compare blood oxygenation between both groups in the “pre” and “post” tests with the alpha level 0.05. Prior to final analysis, data were screened for normality assumption, homogeneity of variance, and presence of extreme scores. This exploration was done as a pre-requisite for parametric calculations of the analysis of difference. Descriptive analysis using histograms with the normal distribution curve showed that the data were normally distributed and not violates the parametric assumption for each of the measured dependent variables. Additionally, testing for the homogeneity of covariance revealed that there was no significant difference with p values of > 0.05. The box and whisker plots of each of the tested variables after removal of the outliers were done. All these findings allowed the researchers to conduct parametric analysis.
Results
As shown in Table 1, the general characteristics for all subjects in studied groups A and B at the entry of the study. Group A: the means of their age, BMI, and gestational age were 26.65 ± 1.38 years, 27.42 ± 1.23 kg/m2, 28.8 ± 1.45 weeks, respectively.
Group B: the means of their age, BMI, and gestational age were 27.75 ± 1.2 years, 27.86 ± 1.37 kg/m2, 28.9 ± 1.7 weeks, respectively.
There was no statistically significant difference between the mean value of age, weight, height, BMI, and gestational age of the study group (A) and control group (B) where their t and p values were − 1.694, 0.098, − 1.124, 0.268, − .749, 0.458, 0.131, 0.869, respectively and 0.224, 0.824 (Table 1).
Table 2 demonstrated the blood oxygenation pre- and post-treatment for group (A). Paired t test showed that there was significant difference between pre- and post-treatment as pre-treatment the blood oxygenation was (96.21 ± 0.48) and post-treatment it was (99.98 ± 0.52). P value was (0.025) and the percentage of improvement was 3.91 % (increase).
Regarding group B
Table 3 demonstrated the blood oxygenation pre- and post-treatment for group B. Paired t test showed that there was significant difference between pre- and post-treatment as pretreatment the blood oxygenation was (96.16 ± 0.47) and post-treatment it was (97.49 ± 0.46), the P value was (0.05) and the percentage of improvement was 1.38 % (increase).
Table 4 the “independent t test” results for the blood oxygenation pre- and post-treatment between groups A and B. There was non-significant difference in pretreatment values where the p value was (0.872). There was significant difference in the post-treatment values, p value was (0.020).
Discussion
The results of this study showed that the percentage of improvement in blood oxygenation was 3.91% (increase) post-treatment for group A. As that there was significant difference between pre- and post-treatment where the mean value of the blood oxygenation was 96.21 ± 0.48 and 99.98 ± 0.52, pre- and post-treatment respectively. P value was 0.025.
In group B, the percentage of improvement in blood oxygenation was 1.38% (increase) in post-treatment. There was significant difference between pre- and post-treatment as the mean values were 96.316 ± 0.47 and 97.49 ± 0.46, pre- and post-treatment respectively. P value was (0.05). These results were supported with the following:
The body keeps up a steady degree of oxygen saturation, generally, by chemical procedures of aerobic metabolism related with breathing. Utilizing the respiratory system, red blood cells, categorically the hemoglobin, accumulate oxygen in the lungs and appropriate it to the remainder of the body. The necessities of the body's blood oxygen may vary, for example, during exercise when more oxygen is required or when living at higher elevations. A platelet is said to be "immersed" while conveying an ordinary measure of oxygen [16].
The study came in agree with study by Pirhonen et al. [17] who upheld the noteworthy impact of transient exercise in the pregnant ladies reacted by expanding the oxygen saturation till 29 weeks. From that point onward, the saturation level abatements yet stays at a more elevated level at a rate 95% even half year after conveyance. As the activity kept up the degree of oxygen saturation, As the investigation were 40 healthy women were enlisted to the examination before an arranged pregnancy, and were pursued multiple times during the pregnancy and for as long as half year after delivery. A submaximal bicycle exercise test with a target heart rate of 85% of the predicted age-adjusted maximum was performed. Maternal oxygen saturation was persistently recorded utilizing a pulse oximeter. Subsequently, at the extreme workload, the maternal oxygen saturation had expanded fundamentally as of now at about 2 months gestation and stayed at an essentially more elevated level until 29 weeks of gestation. From there on, the oxygen saturation kept on being higher even at half of year post-partum period during the exercise test, the most minimal saturation was found during the late recuperation time frame, and afterward stayed unaltered previously, during and after gravidity.
Larsson et al. [18] recorded in his examination, which included 40 pregnant ladies and 11 controls performing low-impact aerobic exercise were checked before work out, at a most extreme exercise level, and after exercise concerning their core temperature, their heart rate, and their oxygen saturation level. As compared with pre-exercise values, oxygen saturation among ladies was fundamentally improved at both maximum-exercise and post-exercise measurements, but no measurement was beneath 95% in the oxygen saturation.
During maximal exercise, an outrageous lactate overflow to blood permits pH decline to beneath 7.1 and as indicated by the O2 dissociation curve, this is critical for SaO2. At the point when imbuement of sodium bicarbonate keeps up a steady blood buffer capacity, acidosis is lessened and SaO2 increments from 89 to 95%. This empowers exercise ability to expand, an impact additionally observed when O2 supplementation to inspired air restores arterial oxygenation. In that circumstance, exercise capacity increases less than can be clarified by VO2 and CaO2. Besides, the adjustment in muscle oxygenation during maximal exercise is not influenced when hyperoxia and sodium bicarbonate constrict desaturation. It is recommended that different organs profit by improved O2 accessibility and particularly the cerebrum seems to build its oxygenation during maximal exercise with hyperoxia [19]. The consequence of concentration was bolstered by Stewart and Pickering [20] as the outright oxygen utilization (1/min) was expanded with propelling pregnancy very still and maximal exercise; however, the useful oxygen utilization (VO2) (ml/kg/min) was not changed during pregnancy.
The lower maternal standard PCO2 favors transplacental exchange of carbon dioxide from the baby to the maternal dissemination for expulsion. Maternal PaO2 increments somewhat due to the expanded moment ventilation and alveolar ventilation and may accomplish levels of 100 to 105 mmHg. This higher weight encourages transplacental oxygen move. Transforming from a supine to sitting position increases PaO2 by around 13 mmHg [21].
Cardiac output is higher for a given exercise level in pregnant ladies contrasted with non-pregnant ladies. This distinction is principally because of an expansion in the stroke volume. The relatively more prominent increment in cardiac output with exercise brings about a decrease in the contrast between the blood vessel and blended venous oxygen content contrasts (CaO2–CvO2) contrasted and the non-pregnant state, prompting expanded oxygen conveyance to the embryo during maternal exercise. Not many investigations have performed side effect constrained maximal cardiopulmonary exercise tests in late pregnancy. Maximal O2 utilization has been noted to be decreased in inactive pregnant ladies yet is related with lower top pulses and might be incompletely because of exertion [8].
This came in concur with study by Nepal et al. [22] as deep breathing amends the blood oxygenation (SpO2) and influences the hemodynamics during pregnancy hypoxia. They examined the hemodynamic and ventilatory impacts of slow deep breathing at high height in normal subjects. Toward the finish of slow breathing, an increase in SpO2 (study A: from 80.2 ± 7.7% to 89.5 ± 8.2%; study B: from 81.0 ± 4.2% to 88.6 ± 4.5; both p < 0.001) and noteworthy decreases in both pulmonary and systemic arterial pressure happened. This was related with expanded tidal volume and no adjustments in minute ventilation or pulmonary CO dispersion. Slow deep breathing ameliorates ventilation efficiency for oxygen as appeared by blood oxygenation increment and it decreases the pulmonary and systemic blood pressure at high height however does not change the pneumonic gas dissemination.
Maximal oxygen uptake (VO2 max) of the person expands surprisingly with controlled exercises incrementing consistently. The expanded one is VO2 max, yet in addition individual’s maximum respiratory minute volume and maximum heart minute volume show increment by influencing one another. A high aerobic capacity is changed over to an anaerobic capacity positively [23]. SpO2 is the measure of oxygen conveyed relying upon hemoglobin in the blood and this structures the primary system for the transportation of oxygen to the cells (SpO2 was utilized to demonstrate that a non-invasive measurement was utilizing the pulse oximeter). Estimation of oxygen saturation provides data about hypoxia [24].
During pregnancy, submaximal oxygen uptake alterations (V̇O2) rely upon the sort of activity performed. During maternal rest or submaximal weight-bearing activity (for example walking, treadmill exercise, stepping), absolute maternal V̇O2 is essentially expanded contrasted and the non-pregnant state. The size of progress is roughly corresponding to maternal weight gain [25].
At the point when pregnant ladies play out the submaximal weight-supported exercises on land (for example level cycling), the discoveries are conflicting. A few investigations revealed fundamentally expanded total V̇O2, while numerous others announced unaltered or just marginally expanded absolute V̇O2 contrasted and the non-pregnant state. The last discoveries might be clarified by the way that the metabolic interest of cycle practice is to a great extent free of the maternal weight, bringing about no absolute V̇O2 alteration [26]. This investigation came in help with an old examination Lotgering et al. [27] maximal VO2 was unaffected by pregnancy during bicycle (BE) and treadmill exercise (TE). O2 take-up (VO2) expanded at rest, the measure of O2 accessible for work out for exercise (exercise minus rest) would in general abatement with advancing gestation, reaching statistical consequentiality only during TE at 35 weeks gestation.
As the study by Heenan et al. [28] analyzed pregnant (n = 14, mean gestational age 34.7 ± 0.4 weeks), and non-pregnant control group (n = 14) included physically active, healthy ladies. The point of respiratory compensation, maximal oxygen uptake (V̇O2max), the ventilatory threshold, and calculated work efficiency did not vary altogether among pregnant and non-pregnant ladies. Nonetheless, during the maximal exercises, the respiratory exchange proportion, and peak post-exercises lactate, and abundance post-exercises oxygen consumption were significantly lower in the pregnant group.
During weight-bearing exercise, the work efficiency was demonstrated to be amended in athletic ladies who keep practicing and the individuals who quit practicing during pregnancy. At the point when balanced for weight gain, the expanded proficiency is kept up all through the pregnancy, with the improvement being more noteworthy in practicing ladies. Aerobic training substantially changes the respiratory response to exercises. This is accomplished by an increase in both maximal respiratory rate and maximum tidal volume [29].
In a study by McAuley et al. [30] analyzed the impacts of the aerobic conditioning during the second and third trimesters of human pregnancy on the ventilatory reactions to graded cycling. Beforehand, inactive pregnant ladies were appointed haphazardly to an exercise group (n = 14) or a non-exercising control group (n = 14). Data were gathered at 15–17 weeks, 25–27 weeks, and 34–36 weeks of pregnancy. Testing included 20 W min−1 increments in the work rate to a heart rate of 170 beats min−1 and (or) volitional fatigue. Breath-by-breath ventilatory and alveolar gas exchange estimations were compared during rest, a standard submaximal VO2 and the peak exercise. Within both groups, resting (V̇O2max) increased significantly with advancing gestation. Peak work rate, respiratory rate VO2, VCO2, and O2 pulse (VO2/HR) were expanded after physical conditioning.
The way that VO2 max, a determinant of aerobic capacity, is high enables the human body to lead practice longer in homeostatic conditions. During physical activity, 6 critical digits are known to decide how a lot of barometrical air oxygen utilized from alveoles moving to skeletal muscle mitochondria can be utilized [31]. (1) oxygen uptake into the lungs through alveolar ventilation, (2) going of oxygen through alveolar-capillary membrane by means of diffusion, (3) combining of oxygen with hemoglobin, (4) coming too oxygen to capillary in tissue levels via the artery blood, (5) dispersion of oxygen to mitochondria in capillary levels, (6) utilization of oxygen in oxidative phosphorylation and ATP creation after use. Working of any of these means at high limit without anyone else does not imply that more oxygen would be utilized by skeletal muscle tissue however a decline in limit of any of them will cause oxygen take-up decline influencing all responses [32].
The way that the degree of oxygen required for the performance in the arterial blood of the human body cannot be kept up during substantial physical activity prompts the confinement in the capacity of these people. Because of the way that oxygen substance of the blood vessel blood is straight forwardly conclusive in the aerobic sporty performance capacity, the variables affecting the body’s oxygenation has become an intriguing examination subject by practice physiologists and training scientists [33].
Maternal exercise has critical impact on pregnancy-induced alterations in ventilation and (or) alveolar gas exchange either during standard submaximal exercise or at rest [30].
As the breathing exercises in group B training-induced increment in the ventilatory threshold T (vent) and the peak oxygen pulse support the efficiency of prenatal fitness programs to improve the capacity of maternal work. As this came in help with the following:
Cardio-respiratory endurance is the capacity of the heart, veins, and lungs to carry oxygen to muscles during the aerobic activity. Aerobic training improves capacity of the lung with the goal that more oxygen can enter the body during inhalation. Carbon dioxide increments when muscles are working hard, which increases the respiratory rate [32].
Determinately, in this study, regardless of the physiological changes incited by pregnancy, which are fundamentally created to fulfill the expanded metabolic needs of mother and fetus, pregnant women benefit from performing the regular physical activity, there are improvements of cases during working in the study:
-
Increase capacity to workload without sensation of breathless as hyperventilation as inability to walk or any activities.
-
Decrease complains from inability to breathe or difficulties to breathe in and out when make activities.
-
Regulate breathing rate without shallow breathing or hyperventilation, these results were supported with the following:
Regular physical activity is related with improved physiological, psychological, and metabolic parameters, and with diminished danger of morbidity and mortality. Recent suggestions planned for improving the wellbeing and prosperity of non-pregnant ladies instruct that a gathering with respect to ≥ 30 min of moderate physical action ought to happen on most, if not all, days of the week [34].
Regular physical activity has been demonstrated to bring about stamped for mother and fetus. Maternal advantages incorporate improved cardiovascular capacity, constrained pregnancy weight increase, diminished musculoskeletal distress, decreased occurrence of muscle spasms and lower limb edema, state of mind stability, lessening of gestational diabetes mellitus and gestational hypertension [7].
Conclusion
It could be concluded that aerobic exercise combined with breathing exercises improve the oxygen saturation in pregnant women.
Availability of data and materials
The data collected and/or analyzed during the study are available from the corresponding author on reasonable request.
References
Jensen D, Wolfe L, Slatkovska L. Effects of human pregnancy on the ventilator chemo reflex response to carbon dioxide. Am J Phys Regul Integr Comp Phys. 2005;288(5):369–75.
Ajne G, Ahlborg G, Wolff K, Nisell H. Contribution of endogenous endotheline -1 to basal vascular tone during normal pregnancy and preeclamsia. Am J Obstet Gynecol. 2005;193:234.
Charles P, Wolfe R, Whitby M. SMART-COP: a tool for predicting the need for intensive respiratory or vasopressor support in community-acquired pneumonia. Clin Infect Dis. 2008;47(8):375–84.
Al-Ansari MA, Hameed AA, Al-Jawder SE. Use of noninvasive positive pressure ventilation during pregnancy: case series. Ann Thorac Med. 2007;2:23–5.
Gabbe SG, Niebyl JR, Simpson JL. Obstetrics: normal and problem pregnancies. 5th ed. Philadelphia: Churchill Livingston; 2007. p. 70.
William D, McArdle N, Frank I, Katch H, Victor L, Katch M. Essentials of exercise physiology. 3rd ed: Philadelphia, Lippincott Williams & Wilkins; 2006. p. 204. ISBN 978-0-7817-4991-6
Mottola M. Exercise prescription for overweight and obese women: pregnancy and postpartum. Obstet Gynecol Clin N Am. 2009;36:301–16.
Wolfe LA, Charlesworth SA, Glenn NM, Heenan AP, Davies GA. Effects of pregnancy on maternal work tolerance. Can J Appl Physiol. 2005;30:212–32.
Jensen D, Webb KA, Wolfe LA, O'Donnell DE. School of kinesiology and health studies, clinical exercise physiology laboratory. Kingston: Physical Education Center, Queen's University; 2007. Epub 2006 Aug 22. Respir Physiol Neurobiol
Penney DS. The effect of vigorous exercise during pregnancy. J Midwifery Women’s Health. 2008;53:155–9.
Yokogawa M, Kurebayashi T, Soma K, Miaki H, Nakagawa T. Investigation into deep breathing through measurement of ventilatory parameters and observation of breathing patterns. J Vis Exp. 2019;16(151):20–5.
Hudson AL, Walsh LD, Gandevia SC, Butler JE. Respiratory muscle activity in voluntary breathing tracking tasks: implications for the assessment of respiratory motor control. Respir Physiol Neurobiol. 2019;21:30–3.
Q'Sullivan S, Schmitz TS. Chapter 16, Coronary artery diseases. In: Physical rahapition assessment and treatment. 3rd ed. Philadelphia: Davis Company; 1999. p. 297–321.
Wilmore JH, Costill DL. Aerobic exercises and endurance. Phyision Sport Med. 2003;31:906–13.
Beall C. Oxygen saturation increases during childhood and decrease during adulthood among high altitude native Tibetans residing at 3800-4200m. High Med Biol J. 2000;1(1):25–32.
Ellison A. Bronwyn A. Normal range of blood oxygen level. Livestrong.com. Livestrong.com. Retrieved 6 June 2013.
Pirhonen JP, Lindqvist PG, Marsal K. A longitudinal study of maternal oxygen saturation during short-term submaximal exercise. Clin Physiol Funct Imaging. 2003;23(1):37-41.
Larsson L, Lindqvist PG. Low-impact exercise during pregnancy-a study of safety. Acta Obstet Gynecol Scand. 2005;84(1):34-8
Nielsen HB. Arterial desaturation during exercise in man: implication for O2 uptake and work capacity. Scand J Med Sci Sports. 2003;13(6):339-58.
Stewart IB, Pickering RL. Effect of prolonged exercise on arterial oxygen saturation in athletes susceptible to exercise-induced hypoxemia. Scand J Med Sci Sports. 2007;17(4):445–51.
Yeomans ER, Gilstrap LC. Physiologic changes in pregnancy and their impact on critical care. Crit Care Med. 2005;33(10):256–8.
Nepal O, Pokharel BR, Khanal K, Mallik SL, Kapoor BK, Koju R. Relationship between arterial oxygen saturation and hematocrit, and effect of slow deep breathing on oxygen saturation in Himalayan high altitude populations. Kathmandu Univ Med J (KUMJ). 2012;10(39):30-4.
Giuliano KK, Higgins TL. New generation pulse oximetry in the care of critically ill patients. Am J Crit Care. 2005;14:26–39.
Hakemi A, Bender JA. Understanding pulse oximetry advantages and limitations. Home Health Care Manag Pract. 2005;17:416–8.
Pivarnik JM, Chambliss HO, Clapp JF. Special communications, roundtable consensus statement: impactof physical activity during pregnancy and postpartumon chronic disease risk. Med Sci Sports Exerc. 2006;38:989–1006.
Borodulin KM, Evenson KR, Wen F, Herring AH, Benson AM. Physical activity patterns during pregnancy. Med Sci Sports Exerc. 2008;40(11):1901–8.
Lotgering FK, van Doorn MB, Struijk PC, Pool J, Wallenburg HC. Maximal aerobic exercise in pregnant women: heart rate, O2 consumption, CO2 production, and ventilation. J Appl Physiol. 1991;70:1016–23.
Heenan AP, Wolfe LA, Davies GA. Maximal exercise testing in late gestation: maternal responses. Obstet Gynecol. 2001 Jan;97(1):127-34.
Wilmore JH, Costill D, L. Aerobic exercises and endurance. Phys Sport Med. 2003;31:906–13.
McAuley SE, Jensen D, McGrath MJ, Wolfe LA. School of Physical and Health Education, Queen's University, Kingston, Ontario K7L 3N6, Canada. Can J Physiol Pharmacol. 2005;83(7):625–33.
Taylor NA, Groeller SH. Physiological bases of human performance during work and exercise. Philadelphia, Churchill Livingstone Elsevier; 2008. p. 169–76.
Kurdak SS. Does respiratory system restrict the maximal exercise capacity? Solunum. 2012;14:12–20.
Moazami MN, Bijeh S, Gholamian A. The response of plasma Leptin and some selected hormones to 24-weeks aerobic exercise in inactive obese women. Int J Sport Stud. 2013;3(1):38–44.
Kardel KR. Effects of intense training during and after pregnancy in top-level athletes. Scand J Med Sci Sports. 2005;15(2):79–86.
Acknowledgements
The authors thank all the participants in this study for their cooperation.
Funding
No funding was obtained for this study.
Author information
Authors and Affiliations
Contributions
We affirm that the submission represents an original work that has not been published previously and is not currently being considered by another journal. Also, we confirm that each author has seen and approved the contents of the submitted manuscript. This work was carried out in collaboration between all authors. Author GEE designed the study, wrote the protocol and wrote the first draft of the manuscript. Author HFEME managed the literature searches and performed the statistical analysis. Authors YMA and HOG managed the analyses of the study. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval was obtained from the institutional review board of the Faculty of physical therapy, Cairo University by number P.T.REC/012/002499) before starting of the study and the clinical trial registration in Clinicaltrial.gov with an identifier number NCT04077931. The study was followed the Guidelines of Declaration of Helsinki on the conduct of human research.
Before the start of the first session, each pregnant woman was informed about the program of exercises, informed written consent form was signed from each woman before participation in the study, and agreed to publication of the treatment results. The safety and confidentiality were assured, and all the procedures of evaluation and treatment were carried out in compliance with laws and institutional guidelines.
Consent for publication
Informed written consent form was signed from each woman before participation in the study, and agreed to publication of the treatment results.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Elsisi, H.F.E.M., Aneis, Y.M., El Refaye, G.E. et al. Blood oxygenation response to aerobic exercise combined with breathing exercises in pregnant women: a randomized controlled trial. Bull Fac Phys Ther 27, 16 (2022). https://doi.org/10.1186/s43161-022-00073-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43161-022-00073-z