Abstract
Background
Controversy exists regarding the appropriate level of sympathectomy for primary palmar hyperhidrosis (PH) as different levels are associated with variable postoperative patients’ satisfaction and potential complications. The aim of this study was to investigate the safety, efficacy, and outcome of T2-T3 thoracoscopic sympathectomy (TS) versus T4 TS in this age group.
Results
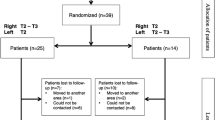
This prospective study included 32 patients (17 males and 15 females) with primary PH treated at the department of pediatric surgery, in our institution during the period from February 2019 to February 2020. Inclusion criteria included moderate and/or severe degrees of PH not responding to conservative measures. The patients were divided randomly into two groups: group I treated by T2-T3 TS and group II underwent only T4 TS. All patients were evaluated regarding operative details and postoperative outcome. Follow-up ranged from 6 to 24 months. Group I included 18 patients (14 operated on both sides and 4 operated on one side), and group II included 14 patients (11 operated on both sides and 3 operated on one side). The ages ranged between 5 and 18 years (mean 14.25 ± 3.14 years). The difference in mean age among both groups (14.5 versus 13.9 years) was not statistically significant. The mean operative time was significantly longer in group I (22.4 versus 17.2 min, p value 0.046). The hospital stay (1 day) was similar for both groups. Postoperative compensatory hyperhidrosis (CH) was more frequent in group I (n=7, 50% versus n=5, 45.5%), but the difference was not statistically significant. Postoperative over dryness occurred in 5 patients in group I (28.6%) and temporary Horner’s syndrome in one patient (7.14%). No over dryness or Horner’s syndrome occurred in any patient in group II. The QOL score has improved in both groups; the degree of improvements was better in group II.
Conclusion
Both T2-T3 TS and T4 TS are effective in treating primary palmar hyperhidrosis in children and adolescents. T4 TS is preferred than T2-3 TS due to less frequent postoperative complications and better patients’ satisfaction.
Similar content being viewed by others
Background
Hyperhidrosis is defined as excessive perspiration beyond physiological needs [1]. Primary palmar hyperhidrosis (PH) is part of a triad of excessive sweating affecting the hands, feet, and axillae. The major complaints are bouts of significant amounts of perspiration of the palms, causing severe psychological, social, and occupational inconvenience.
Primary hyperhidrosis is an underrated problem in children and adolescents. Several systemic and topical treatment modalities have been used for the treatment of hyperhidrosis. Topical treatment includes astringents, iontophoresis, and botulinum toxin. Systemic treatment consists of the administration of anticholinergic drugs and psychotherapy. Despite the availability of such modalities, their use has limitations and side effects, and they are not always effective especially in severe cases [2].
Thoracoscopic sympathectomy (TS) has been advocated in severe cases or after failure of non-surgical methods. Previously published studies have showed that TS is feasible in young children and adolescents. Controversy still exists regarding the most appropriate level of sympathectomy. The different levels are associated with different outcomes especially in terms of postoperative complications and patients’ satisfaction.
The aim of this study was to investigate the safety, efficacy, and outcome of T2-T3 versus T4 TS in this age group.
Methods
This prospective randomized comparative study was conducted at the pediatric and vascular surgery units, in our institution during the period from February 2019 to February 2020. A total of 32 patients (children and adolescents) presented with PH with a total of 57 procedures were performed.
The study design was approved by the institutional research ethical committee. Informed consent was taken from all patients/parents after detailed description of the procedure, any other available alternative treatment, or potential complications.
Inclusion criteria included children and adolescents with primary PH after failure of conservative treatment and patients with severe primary PH.
Exclusion criteria were the following: (1) patients with mild symptoms, who can benefit from conservative management; their sweating can be described and noticed as only slight wetting and dampness of the hands not grossly intervening with patients’ activities; (2) refusal of the patient or the parents of thoracoscopic approach; (3) major chest deformities; (4) previous open chest or heart surgery due to expected pleural adhesions; (5) age older than 18 years.
Patients were randomly divided by closed envelopes into 2 groups: group I, treated by T2-T3 TS; group II, treated by T4 TS.
Surgical technique
The procedure was performed under general anesthesia with single-lumen endotracheal intubation. Video-assisted thoracoscopic surgery was used for all patients. Patients were placed in a semi-Fowler’s position with abduction of both arms, the back lifted to 45° from the horizontal level, and the patient was then tilted to the opposite side with the side of procedures being up to help deflate the lung and improve the field.
Two 5-mm ports were inserted in the fifth intercostal space at mid-axillary line and fourth intercostal space at anterior axillary line for the camera and working ports respectively (Fig. 1). Sympathetic chain was interrupted by electrocautery with electrical hook; this was done on either side of the chain which was then freed and hooked from the undersurface before transection (Fig. 2). The transection range was extended about 1–2 cm laterally along the surface of the upper border of the corresponding rib in order to interrupt the potential bypass nerve fibers to decrease the possibility of recurrence. Sympathectomy was always done on one side starting with the dominant hand, and operation on the opposite side was conducted after a period of 3–5 months.
All patients remained at the hospital overnight. Discharge was allowed on the first postoperative day after exclusion of pneumothorax or other complication.
Patients were followed up at outpatient clinic once weekly for the first month and once every month after that for at least 3 months.
Assessment of the quality of life
Patients/parents were asked to fill out a questionnaire before surgery with some details added during the postoperative period. This questionnaire was adopted from the questionnaire proposed by Laje et al. [3] to evaluate objectively the results of TS in the treatment of PH. The score assesses 4 domains: functional aspects, social aspects, interaction with others, and performance under stressful circumstances (Table 1).
For each domain, a set of five questions was provided. Points for each question range from 1 to 5 for the first three domains; 1 is very poor and 5 is excellent. For the last domain, points are scored as 1 (do not know), 2 (strongly agree), 3 (agree), 4 (disagree), and 5 (strongly disagree).
The maximum score to be achieved is 100, scores below 33 signify a poor QOL, scores from 34 to 66 signify a fair QOL, and scores from 67 to 100 indicate good QOL.
Results
The current study included 32 patients (17 males and 15 females). Their ages ranged from 5 to 18 years with a mean age of 14.25 ± 3.14. The mean age of patients at time of surgery was almost equal in both groups (14.5 versus 13.9 years) The patients’ age at the onset of manifestation varied from 4 to 12 years (mean value 6.31 ± 1.97 years). Sixteen of 32 patients (50%) presented at the age of 5–6 years.
Group I included 18 patients treated by T2-T3 TS (14 operated bilaterally and 4 on one side). A total of 32 procedures were done in this group. Group II included 14 patients who underwent T4 TS (11 operated bilaterally and 3 on one side). A total of 25 procedures were done in the second group.
Seven out of the total 32 (21.89%) patients underwent unilateral sympathectomy. Five out of the 7 patients were satisfied with their primary surgery and were not enthusiastic to proceed for surgical intervention for the other side; the other 2 patients were lost to follow-up after 3 months of surgery.
Preoperative severity of symptoms
Thirteen patients (40.6%) had moderate degree, 7 in group I versus 6 in group II. The sweating was described and noticed as significant wetting, needing frequent hand wiping, and affecting the patients’ activities and manual work. Nineteen patients (59.4%), 11 in group I and 8 in group II, had severe degree of hyperhidrosis. Sweating was described and noticed to be excessive, even reaching to dripping from the hands, very frequent and routine wiping of the hands with marked affection of the patient’s daily activities.
Intraoperative and postoperative results
Patients in group I and group II were compared as regards to operative time, any intraoperative complications, and hospital stay (Table 2).
Group I
Fourteen patients had bilateral T2-T3 TS, 7 of them developed compensatory sweating (50%) ranging from mild to moderate degrees, yet all of them were satisfied. Five patients of this subgroup developed postoperative over dryness, three in one hand and 2 in both hands. Four out of those 5 patients were not bothered by such dryness, while one patient requested prescription of soothing agents. One patient sustained transient Horner’s syndrome postoperatively (7.14%) and resolved spontaneously after few weeks; four patients had unilateral T2-T3 TS. One of them developed postoperative over dryness. No compensatory sweating was noticed in any of these 4 unilateral T2-T3 TS patients (Table 3)
Group II
Eleven patients had had bilateral T4 TS, 5 of them (45.4%) developed compensatory sweating ranging from mild to severe degrees, all of them were satisfied with the exception of one case that complained of the degree of the compensatory sweating resulting in some discomfort, yet the patient did not regret having the procedure. None of the eleven patients has developed postoperative over dryness. On the contrary, four of the patients experienced slight moisture of one side (36.3%) not causing a problem for any of these patients. Three patients had unilateral T4 TS, one of them had slight moistness of hand, yet he was satisfied with the result. No compensatory sweating was noticed in any of these 3 patients (Table 3).
Change of QOL
Preoperative overall subjective assessment according to a score ranging from 1 to 5 showed that in group I, 12 patients of the 18 patients (66.6%) rated their QOL as very poor, 4 (22.2%) poor, and 1 (5.5%) good, and one patient (5.5%) rated very good. None of them rated excellent. In group II, 10 patients of the 14 patients (71.4%) rated their QOL as very poor, 3 (21.4%) poor, and 1 (7.1%) good. None of them rated very good or excellent.
An objective validation of the patients/parents assessment using the QOL questionnaire has revealed that in group I, 11 patients had scores < 33 which is poor, and 7 patients had score between 34 and 66 (fair). None of the patients scored 67 or above. In group II, 9 patients had scores below 33 (poor), and 5 patients had score between 34 and 66 which is fair; none of the patients scored 67 or above (Table 4).
The overall subjective evaluation of QOL was fairly concomitant with the objective evaluation using detailed QOL score.
Postoperatively, patients were again asked to evaluate their QOL subjectively on a score ranging from 1 to 5 during the clinic follow-up visits: In group I, 12 patients (66.6 %) rated their QOL as excellent, and 5 patients (27.7%) rated very good. One patient was lost to follow-up after 3 months of the first operation. In group II, 13 patients (%) rated their QOL as excellent (92.8%). One patient was lost to follow-up after 3 months of the first operation.
A repeated postoperative questionnaire 3 months after the last surgery showed a marked change in the patients’ QOL and functionality. In group I, 12 patients scored above 67 (good score); 5 patients scored between 34 and 66 (fair). One patient was lost to follow-up after 3 months of the first operation.
In group II, 13 patients scored above 67 (good). One patient was lost to follow-up after 3 months of the first operation (Table 4).
Discussion
Hyperhidrosis (especially PH) significantly affects the social life and functional aspects of the affected individuals. Many scoring systems have been proposed for evaluation of the condition and the response to provided treatment [3]. Some children have gross problems at their schools with many of them being bullied by their colleagues, schoolmates, and, even worse, their teachers. Hyperhidrosis has also major psychological effects over both patients and their parents. Many of them suffer from significantly lower self-esteem and self-confidence and sometimes force them to self-isolation and negative thoughts.
The appropriate time for surgical intervention has received some attention in recent years. Some studies have showed that the earlier this condition is addressed, the better is the outcome [4]. Steiner et al. included 325 patients, 116 were children (8–14 years of age, median = 13), and 209 were adolescents and adults (15–41 years of age, median =18); they concluded that the children who underwent sympathectomies benefited of the effects the procedure on their daily lives [4] and that the incidence of side effects of the procedure (e.g., compensatory sweating) was significantly lower than that occurred in older adolescents and adults who underwent the same procedure (69.8% vs. 88.5%); in addition, satisfaction rates were also higher 92.2% vs. 80.7% [4].
In the majority of published TS procedures, a biportal approach was used with the first port for the scope and the second as a working port. We have successfully used the same approach in all procedures. There was no need for introducing a third port. Some of the studies however are in favor of introducing a second working port especially in recurrent cases or when adhesions are expected [5].
T2 ganglion has been viewed traditionally as the key pathway for the hands [6,7,8]. T2 interruption has been found to cause dry hands and denervation of the face. Drott suggested that turning off head and face sweating may be the main trigger for compensatory sweating on the trunk [9]. Schmidt et al. found that avoiding T2 ganglion may limit compensatory sweating [10].
The most appropriate segment to be interrupted for the treatment of primary PH is still debatable. A previously published anatomic study showed that the preganglionic fibers to the arm originate mostly from the third to the sixth spinal segments, and the third and fourth segments were considered as main lesions [11]. Lin and Wu reported that few or none of the fibers from T2 or T3 innervate the hands, whereas fibers from T4 to the skin of the palm definitely pass through T2 and T3 [12].
The current study showed that either T2-T3 or T4 sympathectomy produces resolution of the palmar symptoms with good satisfaction of the patients. Mild moisture hands occurred commonly in T4 TS group; this was well tolerated by the patients. Slight moistness occurred in hot weather mainly, and the satisfaction rate in patients with moist hands was even higher than those with dry hands. The occurrence of slight hand moistness was also reported by Liu et al., who compared T3 versus T4 sympathectomy and it was noted in 59.4% of patients who had T4 sympathectomy vs. 25.8% of those who had T3 sympathectomy. A high satisfaction rate (94.2%) was noted in the T4 TS group in his study [13].
Despite the good results regarding resolution of PH and cessation of sweating, TS has its potential side effects. Postoperative compensatory sweating or over dryness of hands occur in some cases. The incidence and severity of these side effects vary significantly in different published series [14, 15]. These postoperative unfavorable consequences are the main focus of current research.
Compensatory sweating after TS is a common side effect. In the current study, postoperative compensatory sweating developed in both groups (50% versus 45.4%). The incidence of this complication varies widely throughout the literature. Zacherl et al. [14] reported an incidence of 69% in a series of 352 patients. In another study by Fredman et al., 90% of patients had compensatory sweating postoperatively [15]. This variability is probably due to the differences in surgical technique and classification of compensatory sweating. One of the topics that needs to be studied and researched is the mechanism of development of CH, since this is not fully understood till now. One of the interesting findings in our study is the onset of occurrence of compensatory sweating as it did not develop in any of the cases after operating on one side and only developed after operating on both sides of the patient. The group of patients who underwent unilateral sympathectomy did not develop any compensatory sweating. Despite the development of compensatory sweating in almost half of the patients, all of them were satisfied with the exception of one case, yet the patient did not regret having the procedure. The overall incidence of compensatory sweating in this study is much less than that in many other series. The impact of sequential bilateral TS rather than simultaneous bilateral TS on development of compensatory sweating was highlighted in a study conducted by Youssef et al. where sequential sympathectomy was found to be a more optimal technique for reduction of compensatory sweating [16]. Confirming this finding needs further studies and prospective controlled randomized clinical trials.
Various techniques have been attempted to reduce the occurrence rates of compensatory sweating. The level and extent of resection of the sympathetic chain are thought to be the factors behind the frequency and severity of compensatory sweating by many authors [14, 15]. The more sympathetic segments excised, especially those including T2, the greater the incidence of severe compensatory symptoms.
In Liu et al.’s study, the overall occurrence rate of compensatory sweating was 66.4% with those in the T3 group being more affected than patients in T4 group. Sweating was found to be mild, and patients did not feel any discomfort in their daily activities [13].
Hand over dryness is a potential side effect of TS surgery. In the current study, this was not documented in any of the cases in T4 group but was common (35%) in group T2-T3. A similar high rate (35%) of over dryness of limbs was also observed in of cases following T2 sympathectomy for PH by Mahdy et al. [17].
The occurrence of Horner’s syndrome is one of the serious potential side effects following the operation. Injury to the sympathetic fibers in T1 (stellate ganglion) leads to its development. Such injury may occur during the operation resulting from transmitted heat via the diathermy or may be due to traction on the ganglion [18]. This complication was reported by Wait et al. in 5% of 322 patients after sympathectomy and in only 0.9% when sympathicotomy (interruption of the sympathetic trunk by its complete transection) was used. This may point to sympathicotomy being a better option since it avoids extensive manipulation and traction on the sympathetic chain [18]. A study of 85 T2-T3 TH procedures done in 44 children reported the occurrence of transient Horner’s syndrome in 18% of cases [19]. Only one case of temporary Horner’s syndrome developed in our study among the T2-T3 group, and it resolved spontaneously within few weeks. The limited development of such side effect in our study could be owed to the limited number of cases in comparison with previous studies; also, much care was given during manipulation at T2 level during surgery. We believe that T4 TS away from stellate ganglion can obviate the occurrence of Horner’s syndrome. Also, the use of bipolar diathermy is always advocated when available rather than monopolar diathermy which is associated with more heat dispersion.
Although T4 ganglion is the main source of sympathetic innervation of the hand, some sympathetic fiber from T3 and T2 ganglions also add to hand innervation sequentially as impulses ascend along the sympathetic chain. Ablation at T2 level, therefore, blocks the impulse from T3 and T4 ganglions to the hand. Likely, ablation at T3 level blocks the impulse from T4 ganglions. T2 sympathectomy results in the most thorough sympathetic denervation of the hands; however, it induces the most common and severe side effects, which makes it a poor option.
T4 TS though theoretically means the least denervation of the hands, it produces resolution of the over-sweating of the hands, and the majority of patients would be satisfied by its results [13]. For such reason, and because it is associated with less morbidity, T4 sympathectomy is recommended to be the operation of choice since the goal of the treatment of PH is to improve the QOL of the patients, rather than the full elimination of sweating function of hands.
Limitation of the study
We acknowledge the limitations of the current study; the number is relatively small in the subgroups of patients. The impact of performing bilateral TS at the same time instead of doing it sequentially on the compensatory sweating rate needs to be investigated.
Conclusion
Based on our study, we may conclude that (1) both T2-T3 and T4 TS are safe and effective treatment options for PH in children and adolescents. (2) Postoperative CH seems to be more frequent with bilateral T2-T3 sympathectomy compared to bilateral T4 sympathectomy. (3) Postoperative CH may be less frequent when TS is done sequentially, and it appears to develop only after bilateral sympathectomy is done. (4) Hand over dryness may occur after T2-T3 TS, while mild moisture hands may be expected after T4 TS. (5) Due to the efficacy of both approaches and potential less postoperative complications and better patients satisfaction in group II, T4 is more preferred than T2-3 TS.
Availability of data and materials
The related data and material of the current study are available from the corresponding author on a reasonable request.
Abbreviations
- PH:
-
Palmar hyperhidrosis
- TS:
-
Thoracoscopic sympathectomy
- CH:
-
Compensatory hyperhidrosis
- QOL:
-
Quality of life
References
Cohen Z, Shinar D, Levi I, Mares AJ. Thoracoscopic upper thoracic sympathectomy for primary palmar hyperhidrosis in children and adolescents. J Pediatr Surg. 1995;30(3):471–3.
Krasna MJ, Demmy TL, McKenna RJ, Mack MJ. Thoracoscopic sympathectomy: the U.S. experience. Eur J Surg Suppl. 1998;164(580):19–21.
Laje P, Rhodes K, Magee L. Mary Kate Klarich Thoracoscopic bilateral T3 sympathectomy for primary focal hyperhidrosis in children. J Pediatr Surg. 2017;52:313–6.
Steiner Z. Cohen, Kleiner O, Matar I, Mogilner J. Do children tolerate thoracoscopic sympathectomy better than adults? Pediatr Surg Int. 2008;24:343–7.
Reisfeld R, Nguyen R, Pnini A. Endoscopic thoracic sympathectomy for hyperhidrosis: experience with both cauterization and clamping methods. Surg Laparo Endo Per Tech. 2002;12(4):255–67.
Lin TS, Fang HY. Transthoracic endoscopic sympathectomy in the treatment of palmar hyperhidrosis with emphasis on perioperative management (1360 case analyses). Surg Neurol. 1999;52(5):453–7.
Chiou TS, Liao KK. Orientation landmarks of endoscopic transaxillary T-2 sympathectomy for palmar hyperhidrosis. J Neurosurg. 1996;85(2):310–5.
Drott C, Gothberg G, Claes G. Endoscopic transthoracic sympathectomy: an efficient and safe method for the treatment of hyperhidrosis. J Am Acad Dermatol. 1995;33(1):78–81.
Drott C. Results of endoscopic thoracic sympathectomy (ETS) on hyperhidrosis, facial blushing, angina pectoris, vascular disorders and pain syndromes of the hand and arm. Clin Auton Res. 2003;13(1):26–30.
Schmidt J, Bechara FG, Altmeyer P, Zirngibl H. Endoscopic thoracic sympathectomy for severe hyperhidrosis: impact of restrictive denervation on compensatory sweating. Ann Thorac Surg. 2006;81(3):1048–55.
Gray H. The sympathetic nerves. In: Lewis WH Anatomy of the human body. 20th ed; 2000. p. 1292–9.
Lin CC, Wu HH. Endoscopic t4-sympathetic block by clamping (ESB4) in treatment of hyperhidrosis palmaris et axillaries, experiences of 165 cases. Ann Chir Gynaecol. 2001;90(3):167–9.
Liu Y, Yang J, Liu J, et al. Surgical treatment of primary palmar hyperhidrosis: a prospective randomized study comparing T3 and T4 sympathicotomy. Eur J Cardiothorac Surg. 2009;35(3):398–402.
Zacherl J, Imhof M, Huber ER, et al. Video assistance reduces complication rate of thoracoscopic sympathicotomy for hyperhidrosis. Ann Thorac Surg. 1999;68(4):1177–81.
Fredman B, Zohar E, Shachor D, Bendahan J, Jedeikin R. Video-assisted transthoracic sympathectomy in the treatment of primary hyperhidrosis: friend or foe? Surg Laparosc Endosc Percutan Tech. 2000;10(4):226–9.
Youssef T, Soliman M. Unilateral sequential endoscopic thoracic sympathectomy for palmar hyperhidrosis: a proposed technique to overcome compensatory hyperhidrosis and improve plantar hyperhidrosis. J Laparoendosc Adv Surg Tech A. 2015;25(5):370–4.
Mahdy T, Youssef T, Elmonem HA, Omar W, Elateef AA. T4 sympathectomy for palmar hyperhidrosis: looking for the right operation. Surgery. 2008;143(6):784–9.
Wait SD, Killory BD, Lekovic GP, et al. Thoracoscopic sympathectomy for hyperhidrosis: analysis of 642 procedures with special attention to Horner’s syndrome and compensatory hyperhidrosis. Neurosurgery. 2010;67(3):652–65718.
Sinha CK, Kiely E. Thoracoscopic sympathectomy for palmar hyperhidrosis in children: 21 years of experience at a tertiary care center. Eur J Pediatr Surg. 2013;23:486–9.
Acknowledgements
Not applicable
Funding
None
Author information
Authors and Affiliations
Contributions
All authors have read and approved the manuscript and agree with its submission to Annals of Pediatric Surgery. E. E: principle investigator, study design, participated in surgery, collection of data, data analysis, writing the draft and final version of the manuscript. MAM, AI MT, approved study design, participated in surgery and follow-up of the patients, reviewed and approved the final version of the manuscript HFA, senior supervisor, study design, review the draft and final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Research Ethics Committee and quality assurance unit of the faculty of medicine, Tanta University, on February 2019, protocol number 32967/02/19. A written informed consent for participation at this study was obtained from parents/guardians.
Consent for publication:
A written consent for publication of the results of this study was obtained from parents/guardians.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Elhalaby, I.E., Mansour, M.A., Tawfik, A.M.I. et al. Thoracoscopic T2-T3 versus T4 sympathectomy for primary palmar hyperhidrosis in children and adolescents: a randomized comparative study. Ann Pediatr Surg 17, 26 (2021). https://doi.org/10.1186/s43159-021-00092-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43159-021-00092-w