Abstract
Background
Genetic variants in the transcription factor 7-like 2 (TCF7L2) gene are related with type 2 diabetes (T2D) and gestational diabetes mellitus (GDM) in various populations, but there are not enough statistics regarding GDM among Egyptian women. We aimed by this study to evaluate the effect of two polymorphisms of rs7903146 and rs12255372 in the TCF7L2 gene with the development of GDM among Egyptian women.
Results
We enrolled 114 pregnant women with normal glucose tolerance and 114 with GDM according to the International Association of Diabetes and Pregnancy Study Groups (IADPSG) guidelines. We gathered records on blood pressure, body mass index (BMI), blood glucose level, hemoglobin A1C (HbA1c), and lipid profile. The genotyping of rs7903146 and rs12255372 polymorphisms was carried out using polymerase chain reaction–restriction fragment length polymorphism (PCR-RFLP). The statistical significance of prepregnancy BMI, fasting blood sugar (FBS), HbA1c, low-density lipoprotein (LDL), and total cholesterol (Tch) was higher, P < 0.001, in GDM women in comparison to pregnant women without GDM. CT and TT genotypes in rs7903146 SNP were 46.5% vs. 54%, P <0.04, OR; CI = 1.9 (1.0 to 3.78); TT carriers were 37.7% vs. 9.6%, P <0.001, OR (CI) = 8.9 (3.7–21.1), respectively. For the TCFL2 gene rs12255372 SNP, GT carriers were 48.2% vs. 39.5%, P= 0.004, OR (CI) = 2.3 (1.3–4.2), while TT carriers were 24.6% vs. 7.9%, P < 0.001, OR (CI) = 6 (2.5–14.3).
Conclusion
The study showed there is a significantly higher incidence of CT/TT genotypes in rs7903146 SNP and GT/TT genotypes in rs12255372 SNP in TCF7L2 gene among GDM women in comparison to healthy pregnant women (controls).
Similar content being viewed by others
Background
Gestational diabetes mellitus (GDM) is a kind of diabetes that is acquired during the gestation period. It is important to distinguish it from overt diabetes. There is a continuous increase in the incidence of GDM [1]. In 2020, the Center of Disease Control (CDC) reported that the prevalence of GDM is around 10% [2]. However, incidence differs from one population to another. There are only 2 existing studies regarding the prevalence of GDM among Egyptians. One took place in Upper Egypt where incidence was about 17.5% and the other in the Delta region (Menoufia governorate) with an incidence of 6%. Among the American population, the occurrence of GDM is around 7% [3, 4]. In Gulf countries, the occurrence of GDM varies between 4.2 and 24.9% [5]. In 2010, many countries followed the guidelines of the International screening of Gestational Diabetes according to the Association of Diabetes and Pregnancy Study Groups (IADPSG) [6]. A couple of years later, after following IADPSG guidelines, the incidence of GDM has been assessed to be approximately 17% worldwide and in specific 10% among North Americans and 25% in Southeast Asia [7].
Due to the global widespread of obesity among young fertile women, the prevalence of GDM is in a constant rapid increase [8]. Hyperglycemic state during the gestation period is directly correlated with the increase in the number of feto-maternal co-morbidities [9]. Type 2 diabetes (T2D) is more common to evolve among pregnant women with a history of GDM as well as their offsprings are highly vulnerable to having diabetes and obesity during their grownup life [10]. Obesity and family history for diabetes both are important risk factors associated with GDM and T2D [11].
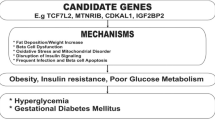
Due to the resemblance between GDM and T2D, it was documented that both might have some genetic factors in common such as single nucleotide polymorphisms (SNPs) which increase the risk for diabetes [12]. TCF7L2 is positioned at chromosome 10q25.3 and its amino acid controls hyperglycemic state in the blood [13]. The actual action of TCF7L2 in developing DM is still under debate though there are theories that DM might occur due to malfunction or decreased number in pancreatic islets [14]. It is assumed that the TCF7L2 gene controls proglucagon expression inside entero-endocrine cells [15]. TCF7L2 is important in the propagation of pancreatic B-cell as well as the production of several incretin hormones, glucose-dependent insulin-tropic peptide (GLP-1) which are released from entero-endocrine cells. GLP-1 also stimulates insulin secretion [16]. TCF7L2 regulates the metabolism of hepatic glucose mainly through inhibiting gluconeogenesis [17, 18]. TCF7L2 gene has been related to T2D in various populations [16, 19, 20]. Intronic regions of the TCF7L2 gene have variants which are well known as strong risk genetic markers for T2D [21]. TCF7L2 polymorphisms have a dual effect on blood glucose level and insulin excretion [16]. TCF7L2 polymorphism rs7903146 has been related with GDM in Danish [22], Australian [20], Greek [23], and Swedish populations [19] as well as other populations [19, 24, 25]. The aim of this study is to evaluate the association of two polymorphisms of rs7903146 and rs12255372 in the TCF7L2 gene with the risk of development of GDM among Egyptian women.
Methods
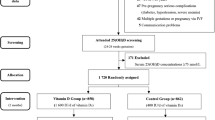
A total of 228 Egyptian women were examined. Healthy pregnant women were classified as the control group (n = 114) and pregnant women with GDM as the GDM group (n = 114). Screening for GDM using oral glucose tolerance test (OGTT) was done for the participants according to the IADPSG guidelines [26]. Participants were given 75 g of glucose. Fasting and 2-h blood glucose levels were assessed after that. The diagnosis of GDM was made after which any one of the following plasma glucose values were exceeded: if the fasting plasma glucose was 92 mg/dL or more or when the 2-h value is 153 mg/dL or more. Values (fasting ≥ 126 mg/dL or 2 h postprandial ≥ 200 mg/dL) specify overt diabetes mellitus (DM), which was excluded from this study. The study was conducted from the period of 2019–2021. Participants were referred to our prenatal diagnosis and fetal medicine department. The study was done after approval was obtained from the ethical committee (Medical research ethical Committee). With approval reference number 19266, it conforms to the provisions of the Declaration of Helsinki. Informed written consent was obtained from all participants in the study. The control group was selected from low-risk pregnant women who came for regular follow-up at our clinic unit to do a 20-week ultrasound. Women who were appropriate to be in the control group in the study were called at 28 weeks to check a normal blood glucose level then accordingly were involved in the study protocol.
Inclusion criteria
All non-diabetic pregnant women, coming for antenatal care, were assessed. Fasting and 2h postprandial, HbA1c were done at 12 weeks for high-risk pregnancies for GDM (first degree relative with diabetes, history of GDM during previous pregnancies, history of delivering overweight babies > 4 kg or prepregnancy overweight; BMI > 25kg/m2, age 20–45 years, and fetal Doppler scan within the normal reference range) [27]. Then, reassessment for the high-risk group was taken at 24–28 weeks, and whoever tested positive for hyperglycemias was included in the case group.
Exclusion criteria
Pregnant women with diabetes history before pregnancy or overt diabetes mellitus (DM) (fasting ≥ 126 mg/dL or 2 h postprandial ≥ 200mg/dL) were excluded from the study. Women known to be hypertensive were also excluded from the study. Any woman who is a smoker or having any pathology other than GDM before or during pregnancy was excluded.
Clinical and laboratory data
Clinical and anthropometric records were collected from patient files containing fasting blood glucose, postprandial, and HA1c, and fat metabolism was evaluated (total cholesterol (TCh), low-density lipoprotein (LDL), high-density lipoprotein cholesterol (HDL), serum triglycerides (TG)).
Genotyping
DNA was extracted from whole blood using the “salting out” method [28] and normalized to 20 ng/μL for the following analyses. Only samples with 280/260 absorbance ratios of 1.8 to 2.0 (NanoDrop, Thermo Scientific) were used in this study. TCF7L2 gene polymorphisms of rs12255372 and rs7903146 gene were carried out using PCR-RFLP analysis as described by Bodhini et al. [29] and Szepietowska et al. [30]. Two sets of primers were used to amplify the loci in the TCF7L2 gene containing the two polymorphisms. The primers used and the size of the PCR products and restriction enzyme used are listed in Table 1 [29]. PCR was carried out in a 50-μl total final volume containing 200 μM dNTPs (Finzyme, Finland), 10 pmole of each primer, 2U of Taq polymerase (Finzyme, Finland), and 500 ng DNA. Thermal cycling conditions were as follows: denaturation at 95°C for 10 min, followed by 30 cycles of denaturation at 95 °C for 50 s, annealing at 56 °C 50 s, and elongation at 72 °C for 50 s followed by a final elongation of 5 min. Ten microliters of a successfully amplified PCR fragment containing the rs7903146 polymorphism was digested with RsaI enzyme (Fermentas, Germany) and incubated at 37 °C for 3 h and the fragments were run on 3.5% agarose gel stained with ethidium bromide and analyzed under ultraviolet light. The RsaI enzyme cuts digested PCR product (113 bp) into two fragments (91 and 22 bp ) in the presence of the C allele as shown in Fig. 1.
A 3.5% agarose gel illustrating digestion of the PCR products with RsaI for detection of the rs7903146 polymorphism. Lanes 1–3 and 5: 4 samples with the C/C genotype (91 and 22 bp). Lanes 4, 6, 7, and 8: 4 samples with the T/C genotype (113, 91, and 22 bp). Lane 9: one sample with the T/T genotype (113 bp). Lane M: 50-bp ladder (Fermentas, Germany)
On the other hand, ten microliters of PCR fragments containing the rs12255372 was digested with Tsp509I (Fermentas, Germany) and incubated at 65 °C for 3 h and the fragments were run in 3.5% agarose gel stained with ethidium bromide and analyzed under ultraviolet light. The Tsp509I enzyme cuts PCR product (346 bp) in three fragments (143, 104, 99 bp) in the presence of the G allele while the T allele creates an additional site for the enzyme resulting in five fragments (128, 104, 104, 99, 17 bp) as shown in Fig. 2.
A 3.5% agarose gel illustrating digestion of the PCR products with Tsp509I for detection of the rs12255372 polymorphism. Lane 1: undigested PCR product (346 bp). Lanes 2 and 4–6: 4 patients with the G/G genotype (143, 104, 99 bp). Lane 3: 1 patient with the T/T genotype (128, 104, 99, 17 bp). Lanes 7–9: three patients with the G/T genotype (143, 128, 104, 99, 17 bp). Lane M: size marker (50-bp DNA ladder, Fermentas, Germany)
Statistical analysis
Statistical analysis was done using IBM© SPSS© Statistics version 22 (IBM© Corp., Armonk, NY, USA). Normality was tested using the Kolmogorov–Smirnov test. Comparisons of parameters with normal distribution were performed using the Student t-test for independent samples. Categorical variables were compared using the Fisher exact test (two-tailed) or the chi-square test, as appropriate. Allele frequencies and Hardy–Weinberg (HW) equilibrium were verified using the chi-square test. Probability lower than 5% (P < 0.05) was considered significant. The genotypic relative risk was assessed by comparing the GDM with the control group and calculating the odds ratio and 95% confidence interval.
Results
The anthropometric characteristics and laboratory data of all participants are demonstrated in Table 2.
Both groups were comparable in age, P= 0.05. GDM patients were significantly weightier with a higher body mass index, P= 0.05. Blood pressure was within the normal range, P <0.001, but still significantly higher among the GDM group in comparison to healthy pregnant women in the control group. Family history of diabetes was more prominent among the GDM group, P=0.01. Among the GDM group, fasting glucose and glycated hemoglobin were lying in the normal reference range, signifying that those patients had a past good glycemic index. Postprandial hyperglycemia was observed among the GDM group, which was more than 153 mg/dL but less than 200 mg/dL indicating the presence of GDM and the absence of preexisting overt diabetes according to IADPSG guidelines [26]. Those results display the occurrence of a hyperglycemic surge in the GDM group, which is well-matched with the studied disease as shown in Table 1. Lipid profile was normal apart from total cholesterol (Tch) and LDL which were significantly higher among the GDM group in comparison to controls, P = 0.02 and 0.001, respectively.
All genotypes in both groups were in consistency with HW equilibrium (P N 0.05). Regarding rs7903146 SNP, CT and TT genotypes were more prominent among GDM in comparison to the control group; CT carriers among the GDM group were 46.5% vs. 54% and TT carriers were 37.7% vs. 9.6%, respectively. Consequently, dominant and recessive models were highly significant among the GDM group in comparison to the control group. As for the rs12255372 SNP, GT and TT genotypes were also more prominent among the GDM group in comparison to the control group; GT carriers among GDM were 48.2% vs. 39.5%. TT carriers were 24.6% vs. 7.9%. Consequently, dominant and recessive models were highly significant among the GDM group in comparison to the control group. The T allele in rs7903146 is 61% among the GDM group vs. 36.8% among the control group, having a P value of < 0.001, OR 2.6, and CI 1.8–3.9. The T allele in rs12255372 SNP among the GDM group was 51.3% vs. 75.5% among the control group having a P value of < 0.001, OR 2.9, and CI 1.9–4.4 as shown in Table 3.
Discussion
GDM is broadly studied, yet its pathophysiology is not clearly understood. In the meantime, it is important to consider women either with a positive family history of T2D or had a previous history of GDM are at a high risk for developing GDM in upcoming future pregnancies. It is hypothesized that GDM might have similar risk factors and genetic liabilities with T2D [31]. The approximate incidence of acquiring diabetes is nearly 60% in the upcoming future among females with GDM. Associated factors predicting the development of T2D afterwards stay comparable between several cohorts [32]. We aimed by this study to evaluate the effect of two polymorphisms of rs7903146 and rs12255372 in the TCF7L2 gene with the development of GDM among Egyptian women.
Among different populations, TCF7L2 is known to be the most common risk gene for T2D. It is the most frequently examined gene among women with GDM [33, 34]. The TCF7L2 gene polymorphisms were documented to be correlated with GDM in many populations [24, 35, 36]. Conferring to the literature, there is not a highlight on the specific geographical area for TCF7L2 SNP allele frequency [37]. In our study, clinical parameters including BMI and hypertension measurements among the GDM group were comparable with other published studies that stated that pregnant women with GDM have a higher BMI and more frequency of hypertension in comparison to healthy controls [38, 39]. Throughout the normal gestation period, Tch and TG levels in the maternal blood are more prone to a sustained increase [40]. Those fluctuations in lipid profile are intensified with the existence of GDM [41]. This explains the difference found in the lipid profiles among the studied groups as shown in Table 1. Percentages of the other laboratory parameters were as predicted, and the results were comparable to other reported studies representing GDM patients with acceptable glycemic index as shown in Table 1 [42].
Women enrolled in this study were entirely Egyptians. CT and TT genotypes in rs7903146 SNP were more prominent among the GDM group in comparison to the control group. Women carrying the T allele have a nearly 2-fold increase risk for GDM. Regarding rs12255372 SNP, GT and TT genotypes were more prominent among the GDM group in comparison to the control group. Women carrying the T allele have a nearly 3-fold increase risk for GDM.
Reyes-López et al. reported that poor β-cell activity, maternal prepregnancy overweight, and rs12255372 risk allele are all independent risk factors related with the evolving of gestational diabetes [43]. Dan Ye and his colleagues studied 18 SNPs within TCF7L2 and found out that rs290487, rs6585194, and rs7094463 polymorphisms are significantly related with the existence of GDM [31]. A meta-analysis study done by Chang and his colleagues reported a direct relationship between TCF7L2 alleles and the presence of chronic pregnancy hyperglycemia [44]. The study reported that six polymorphisms in the TCF7L2 gene had a highly significant correlation with the increased risk of GDM among the entire population. Chang and his colleagues also highlighted the high significance found between diverse ethnic populations [44]. Reyes-Lopez and his colleagues reported that rs12255372 is more prominent among women increasing the liability for insulin glucose tolerance (IGT) status as well as increasing the frequency for developing T2D [42]. Potasso and his colleagues reported that T mutant allele in TCF7L2 rs7903146 is related to the loss of initial postprandial glycemic control and stressed on the necessity of insulin treatment among pregnant women with chronic hyperglycemia, even if other risk interfering factors like BMI had been regulated [41]. There is an increased possibility of having T2D in different cohorts especially among CT/TT genotype carriers of SNP rs7903146 [15]. In a long time study of around 22 years of follow-up, mutant T allele carriers had a poor insulin feedback mechanism to random OGTT as well as greater chance for developing T2D in comparison to CC genotype carriers [13]. Lin and his colleagues conducted a meta-analysis and they reported a significant correlation between mutant allele of rs7903146 with the high chances of acquiring GDM among all genomic models in the entire population of white and Hispanic/Latino as well as Asian subcategories. Lin and his colleagues also stated that homozygous TT allele carriers for the SNP rs7903146 among Asians were highly correlated with the risk of GDM (OR = 2.08) followed by Hispanics/Latinos (OR = 1.80) and whites (OR = 1.51) [45]. It is reported that TCF7L2 has a strong impact on the breakdown and absorption of glucose and lipids; therefore, it is hypothesized that TT carriers might have a greater chance for developing cardiovascular diseases [40]. Francaite et al. reported that CT/TT genotypes in rs7903146 SNP and GT/TT genotypes in rs12255372 SNP in TCF7L2 gene were more prominent among GDM Lithuanian women in comparison to women from the general population [46]. In contrast to our results, de Melo et al. reported that rs12255372 and rs7903146 were not associated with GDM in the Euro-Brazilian population [47]. Siudak et al. also found no relationship between rs7903146 polymorphism of the TCF7L2 gene and GDM in the Polish population [48]. A study was conducted in North India on 115 women with GDM, and TCF7L2 variants rs 7903146 and rs 12255372 showed no association with GDM among the Indian population [49]. Rizk et al. reported that from 114 Arab pregnant women and 45 non-Arab pregnant women with GDM, TCF7L2 rs 7903146 polymorphism showed no association with GDM but the T allele of rs 12255372 showed a significant association with GDM in comparison to healthy controls [50].
Conclusion
In conclusion, we detected a significantly high prevalence of CT/TT genotypes in rs7903146 and GT/TT genotypes in rs12255372 of TCF7L2 gene in women with GDM compared to healthy pregnant women. A good overview of genetic influences might assist in finding a clear path for early detection and efficient management plans regarding GDM. The results from this study will probably help to highlight the possible roles of those variants in our population in developing GDM; yet, wider base studies are needed to find other possible risk factors that increase the prevalence of GDM in the Egyptian population.
Availability of data and materials
The datasets generated and/or analyzed during the current study are not publicly available due to patient’s privacy but are available from the corresponding author on reasonable request.
Abbreviations
- BMI:
-
Body mass index
- GDM:
-
Gestational diabetes mellitus
- GLP-1:
-
Glucagon-like peptide-1
- HbA1c:
-
Glycated hemoglobin
- HDL:
-
High-density lipoprotein
- HW:
-
Hardy–Weinberg
- IADPSG:
-
International Association of Diabetes and Pregnancy Study Groups
- LDL:
-
Low-density lipoprotein
- OGTT:
-
Oral glucose tolerance test
- SNPs:
-
Single nucleotide polymorphisms
- TCh:
-
Total cholesterol
- TCF7L2:
-
Transcription factor 7-like 2
- TG:
-
Triglycerides
- T2D:
-
Type 2 diabetes
References
ADA (2013) Diagnosis and classification of diabetes mellitus. American Diabetes Association. Diabetes Care
Lende M, Rijhsinghani A (2020) Gestational diabetes: overview with emphasis on medical management. Int J Environ Res Public Health 17. https://doi.org/10.3390/ijerph17249573
Hartling L, Dryden DM, Guthrie A, Muise M, Vandermeer B, Aktary WM et al (2012) Screening and diagnosing gestational diabetes mellitus. Evid Rep Technol Assess(210):1–327 (Full Rep)
Moyer VA (2014) Screening for gestational diabetes mellitus: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. https://doi.org/10.7326/m13-2905
Barakat MN, Youssef RM, Al-Lawati JA (2010) Pregnancy outcomes of diabetic women: charting Oman’s progress towards the goals of the Saint Vincent Declaration. Ann Saudi Med. https://doi.org/10.4103/0256-4947.65253
Khalil NA (2017) Screening for gestational diabetes among pregnant women attending a rural family health center- Menoufia Governorate- Egypt. J Fam Med Heal Care. https://doi.org/10.11648/j.jfmhc.20170301.12
Guariguata L, Whiting DR, Hambleton I, Beagley J, Linnenkamp U, Shaw JE (2014) Global estimates of diabetes prevalence for 2013 and projections for 2035. Diabetes Res Clin Pract. https://doi.org/10.1016/j.diabres.2013.11.002
Lende M, Rijhsinghani A. Gestational Diabetes: Overview with Emphasis on Medical Management. Int J Environ Res Public Health. 2020;17(24):9573. https://doi.org/10.3390/ijerph17249573.
Metzger BE, Gabbe SG, Persson B, Lowe LP, Dyer AR, Oats JJN et al (2010) International Association of Diabetes and Pregnancy Study Groups recommendations on the diagnosis and classification of hyperglycemia in pregnancy: response to Weinert. Diabetes Care. https://doi.org/10.2337/dc09-1848
Association AD, ADA (2013) American Diabetes Association: Diagnosis and classification of diabetes mellitus. Diabetes Care
Buchanan TA, Xiang A, Kjos SL, Watanabe R (2007) What is gestational diabetes? Diabetes Care. https://doi.org/10.2337/dc07-s201
Castorino K, Jovanovič L (2011) Pregnancy and diabetes management: advances and controversies. Clin Chem. https://doi.org/10.1373/clinchem.2010.155382
Lyssenko V, Lupi R, Marchetti P, Del Guerra S, Orho-Melander M, Almgren P et al (2007) Mechanisms by which common variants in the TCF7L2 gene increase risk of type 2 diabetes. J Clin Invest. https://doi.org/10.1172/JCI30706
Hansson O, Zhou Y, Renström E, Osmark P (2010) Molecular function of TCF7L2: consequences of TCF7L2 splicing for molecular function and risk for type 2 diabetes. Curr Diab Rep. https://doi.org/10.1007/s11892-010-0149-8
Grant SFA, Thorleifsson G, Reynisdottir I, Benediktsson R, Manolescu A, Sainz J et al (2006) Variant of transcription factor 7-like 2 (TCF7L2) gene confers risk of type 2 diabetes. Nat Genet. https://doi.org/10.1038/ng1732
Stuebe AM, Wise A, Nguyen T, Herring A, North KE, Siega-Riz AM (2014) Maternal genotype and gestational diabetes. Am J Perinatol. https://doi.org/10.1055/s-0033-1334451
Boj SF, Van Es JH, Huch M, Li VSW, José A, Hatzis P et al (2012) Diabetes risk gene and Wnt effector Tcf7l2/TCF4 controls hepatic response to perinatal and adult metabolic demand. Cell. https://doi.org/10.1016/j.cell.2012.10.053
Ip W, Shao W, Song Z, Chen Z, Wheeler MB, Jin T (2015) Liver-specific expression of dominant-negative transcription factor 7-like 2 causes progressive impairment in glucose homeostasis. Diabetes. https://doi.org/10.2337/db14-1329
Shaat N, Lernmark Å, Karlsson E, Ivarsson S, Parikh H, Berntorp K et al (2007) A variant in the transcription factor 7-like 2 (TCF7L2) gene is associated with an increased risk of gestational diabetes mellitus. Diabetologia. https://doi.org/10.1007/s00125-007-0623-2
Freathy RM, Hayes MG, Urbanek M, Lowe LP, Lee H, Ackerman C et al (2010) Hyperglycemia and Adverse Pregnancy Outcome (HAPO) study: common genetic variants in GCK and TCF7L2 are associated with fasting and postchallenge glucose levels in pregnancy and with the new consensus definition of gestational diabetes mellitus from the I. Diabetes. https://doi.org/10.2337/db10-0177
Cauchi S, El Achhab Y, Choquet H, Dina C, Krempler F, Weitgasser R et al (2007) TCF7L2 is reproducibly associated with type 2 diabetes in various ethnic groups: a global meta-analysis. J Mol Med. https://doi.org/10.1007/s00109-007-0203-4
Lauenborg J, Grarup N, Damm P, Borch-Johnsen K, Jørgensen T, Pedersen O et al (2009) Common type 2 diabetes risk gene variants associate with gestational diabetes. J Clin Endocrinol Metab. https://doi.org/10.1210/jc.2008-1336
Pappa KI, Gazouli M, Economou K, Daskalakis G, Anastasiou E, Anagnou NP et al (2011) Gestational diabetes mellitus shares polymorphisms of genes associated with insulin resistance and type 2 diabetes in the Greek population. Gynecol Endocrinol. https://doi.org/10.3109/09513590.2010.490609
Cho YM, Kim TH, Lim S, Choi SH, Shin HD, Lee HK et al (2009) Type 2 diabetes-associated genetic variants discovered in the recent genome-wide association studies are related to gestational diabetes mellitus in the Korean population. Diabetologia. https://doi.org/10.1007/s00125-008-1196-4
Watanabe RM, Allayee H, Xiang AH, Trigo E, Hartiala J, Lawrence JM et al (2007) Transcription factor 7-like 2 (TCF7L2) is associated with gestational diabetes mellitus and interacts with adiposity to alter insulin secretion in Mexican Americans. Diabetes. https://doi.org/10.2337/db06-1682
Metzger BE (2010) International Association of Diabetes and Pregnancy Study Groups recommendations on the diagnosis and classification of hyperglycemia in pregnancy. Diabetes Care. https://doi.org/10.2337/dc09-1848
Parra-Cordero M, Lees C, Missfelder-Lobos H, Seed P, Harris C (2007) Fetal arterial and venous Doppler pulsatility index and time averaged velocity ranges. Prenat Diagn. https://doi.org/10.1002/pd.1868
Lahiri DK, Numberger JI (1991) A rapid non-enzymatic method for the preparation of HMW DNA from blood for RFLP studies. Nucleic Acids Res. https://doi.org/10.1093/nar/19.19.5444
Bodhini D, Radha V, Dhar M, Narayani N, Mohan V (2007) The rs12255372(G/T) and rs7903146(C/T) polymorphisms of the TCF7L2 gene are associated with type 2 diabetes mellitus in Asian Indians. Metabolism. https://doi.org/10.1016/j.metabol.2007.04.012
Szepietowska B, Moczulski D, Wawrusiewicz-Kurylonek N, Grzeszczak W, Gorska M, Szelachowska M (2010) Transcription factor 7-like 2-gene polymorphism is related to fasting C peptide in latent autoimmune diabetes in adults (LADA). Acta Diabetol. https://doi.org/10.1007/s00592-009-0133-4
Ye D, Fei Y, Ling Q, Xu W, Zhang Z, Shu J et al (2016) Polymorphisms in TCF7L2 gene are associated with gestational diabetes mellitus in Chinese Han population. Sci Rep. https://doi.org/10.1038/srep30686
Noctor E (2015) Type 2 diabetes after gestational diabetes: the influence of changing diagnostic criteria. World J Diabetes. https://doi.org/10.4239/wjd.v6.i2.234
Wung SF, Lin PC (2011) Shared genomics of type 2 and gestational diabetes mellitus. Annu Rev Nurs Res. https://doi.org/10.1891/0739-6686.29.227
Reyes-López R, Pérez-Luque E, Malacara JM. Metabolic, hormonal characteristics and genetic variants of TCF7L2 associated with development of gestational diabetes mellitus in Mexican women. Diabetes Metab Res Rev. 2014;30(8):701-6. https://doi.org/10.1002/dmrr.2538.
Huerta-Chagoya A, Vázquez-Cárdenas P, Moreno-Macías H, Tapia-Maruri L, Rodríguez-Guillén R, López-Vite E et al (2015) Genetic determinants for gestational diabetes mellitus and related metabolic traits in Mexican women. PLoS One. https://doi.org/10.1371/journal.pone.0126408
Wang B, Xue X (2020) Investigations of associations between seven gene polymorphisms and gestational diabetes mellitus: evidence from a meta-analysis. Gynecol Obstet Investig. https://doi.org/10.1159/000505453
Guinan KJ (2012) Worldwide distribution of type II diabetes-associated TCF7L2 SNPs: evidence for stratification in Europe. Biochem Genet. https://doi.org/10.1007/s10528-011-9456-2
Bryson CL, Ioannou GN, Rulyak SJ, Critchlow C (2003) Association between gestational diabetes and pregnancy-induced hypertension. Am J Epidemiol. https://doi.org/10.1093/aje/kwg273
Vysočanová M, Floriánová A, Špinar J (2018) Hypertension in pregnancy. Kardiol Rev. https://doi.org/10.7175/cmi.v1i1.615
Rezaei M, Palizban A, Zamani-Doabi S, Shojaee M (2016) Transcription factor 7-like 2 (TCF7L2) gene polymorphism rs7903146 is associated with lipid profile and risk of cardiovascular disease in metabolic syndrome subjects. J Biol Todays World. https://doi.org/10.15412/J.JBTW.01050703
Potasso L, Perakakis N, Lamprinou A, Polyzou E, Kassanos D, Peter A et al (2020) Clinical impact of the TCF7L2 gene rs7903146 type 2 diabetes mellitus risk polymorphism in women with gestational diabetes mellitus: impaired glycemic control and increased need of insulin therapy. Exp Clin Endocrinol Diabetes. https://doi.org/10.1055/a-1008-9223
Reyes-López R, Perez-Luque E, Malacara JM (2019) Relationship of lactation, BMI, and rs12255372 TCF7L2 polymorphism on the conversion to type 2 diabetes mellitus in women with previous gestational diabetes. Gynecol Endocrinol. https://doi.org/10.1080/09513590.2018.1531984
Reyes-López R, Pérez-Luque E, Malacara JM (2014) Metabolic, hormonal characteristics and genetic variants of TCF7L2 associated with development of gestational diabetes mellitus in Mexican women. Diabetes Metab Res Rev. https://doi.org/10.1002/dmrr.2538
Chang S, Wang Z, Wu L, Lu X, Shangguan S, Xin Y et al (2017) Association between TCF7L2 polymorphisms and gestational diabetes mellitus: a meta-analysis. J Diabetes Investig. https://doi.org/10.1111/jdi.12612
Lin PC, Lin WT, Yeh YH, Wung SF (2016) Transcription factor 7-like 2 (TCF7L2) rs7903146 polymorphism as a risk factor for gestational diabetes mellitus: a meta-analysis. PLoS One. https://doi.org/10.1371/journal.pone.0153044
Francaite-Daugeliene M, Lesauskaite V, Tamosiunas A, Jasukaitiene A, Velickienė D (2021) Genetic variants of TCF7L2 gene and its coherence with metabolic parameters in Lithuanian (Kaunas district) women population with previously diagnosed gestational diabetes mellitus compared to general population. Diabetes Res Clin Pract 172. https://doi.org/10.1016/j.diabres.2020.108636
de Melo SF, Frigeri HR, dos Santos-Weiss ICR, Réa RR, de Souza EM, Alberton D et al (2015) Polymorphisms in FTO and TCF7L2 genes of Euro-Brazilian women with gestational diabetes. Clin Biochem. https://doi.org/10.1016/j.clinbiochem.2015.06.013
Gorczyca-Siudak D, Michalak-Wojnowska M, Gorczyca T, Mosiewicz B, Kwaśniewska A, Filip A et al (2016) Association between rs7901695 and rs7903146 polymorphisms of the TCF7L2 gene and gestational diabetes in the population of Southern Poland. Ginekol Pol. https://doi.org/10.5603/GP.2016.0081
Thomas N, Mahesh DM, Chapla A, Paul J, Shwetha N, Christina F et al (2014) Does TCF7L2 polymorphisms increase the risk of gestational diabetes mellitus in South Indian population? Endocr Abstr. https://doi.org/10.1530/endoabs.34.p270
Rizk N (2011) The Associations of Transcription Factor 7-like 2 [TCF7L2] Gene with gestational diabetes mellitus in State of Qatar. Qatar Found Annu Res Forum Proc. https://doi.org/10.5339/qfarf.2011.bmp8
Acknowledgements
Not applicable
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
All authors read and approved the final manuscript. MS: study design, performed the study, and wrote the manuscript. TS: study design and recruitment of cases and controls. KA: analysis and interpretation of data and revised the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All measures followed were in accordance with the ethical standards of the responsible ethical committee (Medical research ethical Committee) of the National Research Centre (NRC), Cairo, Egypt. It conforms to the Helsinki Declaration of 1975, as revised in 2008, with approval reference number 19266. Informed written consent was obtained from all participants in the study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Shalabi, T.A., Amr, K.S. & Shaker, M.M. Are single nucleotide polymorphisms rs7903146 and rs12255372 in transcription factor 7-like 2 gene associated with an increased risk for gestational diabetes mellitus in Egyptian women?. J Genet Eng Biotechnol 19, 169 (2021). https://doi.org/10.1186/s43141-021-00272-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43141-021-00272-6