Abstract
Background
Extended spectrum beta-lactamase (ESBL) pathogens are associated with morbidity and mortality. There is a paucity of data describing the treatments and outcomes of ESBL infections in Malaysia. This study evaluated the treatments, mortality and associated factors among patients hospitalized with infections due to ESBL positive enterobacteriaceae. This is a retrospective study conducted in a tertiary hospital from January 2018 to June 2020. Hospitalized patients with ESBL-positive enterobacteriaceae infections were included. A clinical pharmacist collected data by reviewing the patients’ electronic medical records. The data were analysed using both descriptive and inferential analyses.
Results
This analysis included 110 patients with a mean age of 62.1 ± 14.4 years. Klebsiella pneumoniae (53.6%) and Escherichia coli (40.9%) were the most prevalent pathogens among the 110 infections. Bacteremia (42.7%) was the most frequent diagnosis. The isolates were resistant to majority of penicillins and cephalosporins. However, over a third (39.3%) were susceptible to piperacillin–tazobactam, while carbapenem susceptibility was extremely high (≥ 99%). The most frequently used empiric and definitive antibiotics was piperacillin–tazobactam and meropenem, respectively. Less than a third (28.2%) of patients received active empiric antibiotics, and the mean duration before active antibiotics was 3.9 ± 2.7. Overall, hospital mortality rate was 13.6%, and mortality was significantly associated with ICU admission (AOR 8.75; 95% CI 1.05–72.75; P = 0.045) and diabetes mellitus (AOR 9.85; 95% CI 1.04–93.09; P = 0.046).
Conclusions
Carbapenems are the major antibiotics used to treat ESBL-positive enterobacteriaceae infections. Hospital mortality rate is relatively high and is significantly associated with in patients admitted to ICU and those with diabetes mellitus. Antibiotic stewardship interventions are necessary to promote early administration of active antibiotics and to reduce overuse of carbapenem antibiotics.
Similar content being viewed by others
Background
Gram negative pathogens that produce extended spectrum beta-lactamases (ESBLs) have emerged as a global public health problem. The organisms cause a variety of infections, including those acquired in the community, hospitals, and healthcare settings [1]. Infections caused by these organisms include pneumonia, bloodstream infection, urinary tract infection, peritonitis, biliary tract infection, central nervous system infection, skin and soft tissue infections, bone and joint infections [2]. Infections caused by ESBL producing pathogens are associated with higher mortality than corresponding infections due to non-ESBL pathogens [3]. The mortality rate for ESBL infections ranges between 3.7 and 22.1% [2, 4, 5] which may be explained by a delay in initiating active antibiotic therapy [1, 3]. Due to their higher susceptibility profile compared to other classes of antibiotics such as beta-lactam and beta-lactamase inhibitor combinations, cephalosporins, and fluoroquinolones, carbapenems are considered the drug of choice for both empiric and definitive therapy of infections caused by ESBL pathogens [1, 6]. The increased use of carbapenems, on the other hand, has resulted in the emergence and spread of carbapenem-resistant microorganisms [7].
Enterobacteriaceae is a family of Gram negative bacteria that includes Citrobacter, Klebsiella, Escherichia, and Proteus species. These organism cause a range of community and hospital-acquired infections. In Malaysia, approximately one-third of Escherichia coli and Klebsiella pneumoniae and two-third of Acinetobacter baumanii are resistant to third generation cephalosporin, respectively [8]. The National Antimicrobial Guideline recommends using carbapenems for empiric treatment of infections caused by ESBL producing gram-negative bacteria [9]. According to available data, the mortality rate associated with infection caused by an ESBL pathogen is quite high, ranging between 3.7 and 22.1% [2, 4, 5]. In addition, the mortality rate is higher in patients with severe infections, severe sepsis or shock, advanced age, hospital-acquired infections, and rapidly fatal underlying disease; in patients with K. pneumoniae infection; in patients who received inappropriate empirical therapy; and those admitted to the intensive care unit [2, 10,11,12,13]. There is a paucity of data in Malaysia on the rate and risk factors associated with mortality in patients infected with ESBL pathogens. Identification of risk factors for mortality is critical for designing effective interventions aimed at improving treatment outcomes and reducing antibiotic overuse and resistance. This study aims to determine the microbiological characteristics, treatment outcomes, and risk factors for mortality in patients with enterobacteriaceae infection caused by ESBLs.
Method
Study design and study setting
This is a retrospective observational cohort study involving patients who had ESBL positive enterobacteriaceae infections at a tertiary hospital located on the Eastern Coast of Malaysia. The hospital provides a range of services including medicine, surgery, orthopaedic, critical care, nursing, pharmacy, microbiological and laboratory services.
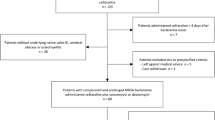
Study population
The study population includes all adults with ESBL positive enterobacteriaceae infections hospitalized at the hospital from January 2018 to June 2020. All infections including central nervous, respiratory tract, urinary tract, gastrointestinal tract, intra-abdominal and bloodstream infections, as well as both community and hospital-acquired infections were included. Those with mono- and polymicrobial infections were included. Those colonized (culture positive but without signs and symptoms of infection) with ESBL positive enterobacteriaceae and those with an infection without hospitalization were excluded.
Data collection
All adult patients hospitalized with an infection due to ESBL positive enterobacteriaceae infections from 01st January 2018 to 30th June 2020 in the selected hospital who fulfil the inclusion criteria were included in the study. A list of patients with infections due to ESBL positive enterobacteriaceae with their hospital numbers was obtained by the investigators from the medical microbiology unit of the hospital. The electronic medical records of the identified patients was reviewed by a clinical pharmacist, who has expertise in infectious diseases and antimicrobial stewardship, for data collection. The electronic medical record was accessed and reviewed after approval from the hospital management. Data was collected retrospectively through the review of patient’s medical records and medication chart. The following information was collected: demographic information such as age, gender, race, ward location, date of admission and discharge; and clinical information such as (i) information related to diagnosis and type of infection (community- and hospital-acquired) [14], presentation with sepsis or shock [15], immune status (severe- versus non-severe immunosuppression), comorbidity, recent surgery (any surgical procedure within 3 months before diagnosis) and recent hospitalization (hospitalization within 3 months before diagnosis), (ii) information related to clinical monitoring: laboratory results, vital signs such as highest daily temperature, highest heart rate, highest respiratory rate and lowest daily blood pressure, and (iii) information regarding empiric and definitive antibiotics used for treatment. Other data collected include microbiological information such as date culture was taken, pathogen isolated and complete antibiotic susceptibility of the isolates, date of subsequent culture(s), organism(s) and resistance profile. In-hospital mortality among the patients was also documented.
Definition of terms and outcomes
Community-acquired infections refer to any infection that starts outside hospital setting or manifests within 48 h after admission into the hospital [16]. Hospital-acquired infection is defined as an infection in which the signs and symptoms begin 48 h or more after hospital admission or infection present at the time of admission or manifests within 48 h after re-admission in patients who were recently discharged from the hospital [16]. Empirical therapy is defined as an antimicrobial therapy initiated before identification of the causative pathogen while definitive therapy is the treatment given after the isolate is known. Severe immunosuppression is defined as any of the following: neutropenia, (< 500/mL), leukaemia, lymphoma, HIV infection with < 200 CD4/mL, solid organ or hematopoietic stem cell transplantation, cytotoxic chemotherapy, steroids (> 15 mg of prednisone daily for > 2 weeks) [3]. Antimicrobial susceptibility was performed by automated system (Vitek 2) and interpreted using Clinical and Laboratory Standards Institute (CLSI) recommendations.
Data analysis
The data would be analysed using Statistical Package for the Social Sciences (SPSS) version 22. The data would be de-identified before analysis. Categorical data would be reported as frequency with percentage while continuous data would be presented as mean (with standard deviation) or median. Bivariate and multivariate regression analyses would be used to determine the risk factors associated with mortality. Only variables that demonstrated statistical significance (P < 0.05) in the bivariate analysis would be included in the multivariate model. P value less than 0.05 would be considered as statistical significance.
Results
Demographic and clinical characteristics of the patients
A total of 110 patients were included in this analysis with a mean age of 62.1 ± 14.4 years. There were more males (58.2%) and Malays (86.4%) included in the analysis. About 22% had intensive care unit admission while 48.5% had sepsis/septic shock. Bacteremia (42.7%) and urinary tract infection (34.5%) were the most common infections. Most of the infections (54.5%) were community-acquired infections. Table 1 summarises the characteristics of the patients included in the study.
Patients’ laboratory data on the first day of infection
Of the 110 patients, 37.3%, 68.2%, and 17.3% had fever, elevated total white blood cell count, and thrombocytopenia, respectively. About 50% had elevated serum creatinine and urea levels while 51.8% had hypoalbuminemia. Tachycardia and anemia was observed in 47.3% and 74.5% of the infections, respectively. Table 2 describes the laboratory parameters and the mortality rates among the patients.
Microbiology of extended spectrum beta-lactamase producing enterobacteriaceae
Of the 110 infections, K. pneumonia (53.6%) and E. coli (40.9%) were the most common pathogens. Other organisms include Proteus mirabilis and Citrobacter spp. About 18% of the infections were polymicrobial infections. Overall, there was high resistant rate to penicillins such as ampicillin and amoxicillin, and cephalosporins among the isolates. However, more than one-third (39.3%) were susceptible to piperacillin–tazobactam. Susceptibility to carbapenems including meropenem and imipenem was very high (≥ 99%). Table 3 shows the antibiotics susceptibilities of the ESBL enterobacteriaceae isolates.
Empiric and definitive antibiotic therapy for ESBL positive enterobacteriaceae infections
Several antibiotics were used for empiric antibiotics therapy among the patients including piperacillin–tazobactam (23.6%), ceftriaxone (12.2%), cefuroxime (10.6%) and meropenem (9.8%). Combination empiric antibiotics was administered in 13.6% of the infections. Less than one-third of the patients (28.2%) received an effective empiric antibiotics. Carbapenems including meropenem (80.4%) and imipenem (9.8%) were the most commonly used definitive antibiotics, followed by ciprofloxacin (4.3). The use of combination definitive antibiotics was lower (5.5%) compared to the empiric therapy. The mean duration before active antibiotic therapy was 3.9 days. Table 4 summarises the antibiotics used for empirical and definitive therapy among patients with carbapenem-resistant infections.
Treatment outcomes and univariate regression analysis for factors associated with in-hospital mortality
Overall, in-hospital rate among the patients was 13.6%. Secondary infections were reported in 12 (10.9%) patients including candida infection (n = 7), trichosporon asahii (n = 2) and carbapenem-resistant gram negative bacilli infection (n = 4). Univariate logistic regression analysis showed that ICU admission (odds ratio [OR] 11.57; 95% confidence interval [CI] 3.43–38.96; P < 0.001), sepsis/septic shock (OR 17.87; 95% CI 2.24–142.27; P = 0.006), diabetes mellitus (OR 3.40; 95% CI 1.01–11.46; P = 0.048), empiric piperacillin–tazobactam (OR 5.62; 95% CI 1.79–17.67; P = 0.003) and elevated serum creatinine (OR 7.86; 95% CI 1.68–36.75; P = 0.009). Other variables associated with mortality were thrombocytopenia (OR 4.20; 95% CI 1.28–13.78; P = 0.018) and transaminitis (OR 4.69; 95% CI 1.51–14.60; P = 0.008). Table 5 describes the univariate logistic regression analysis for factors associated with mortality.
Multivariate regression analysis for the predictors of mortality
Multivariate logistic regression analysis revealed ICU admission (AOR 8.75; 95% CI 1.05–72.75; P = 0.045) and diabetes mellitus (AOR 9.85; 95% CI 1.04–93.09; P = 0.046) were independently associated with in-hospital mortality among the patients. Table 6 summarises the multivariate logistic regression analysis for factors associated with in-hospital mortality.
Discussion
The current study investigated the treatment of ESBL-positive enterobacteriaceae infections, as well as the factors associated with mortality, in hospitalised patients in a tertiary hospital in Malaysia. The most frequently used empiric antibiotics were piperacillin–tazobactam, third, and second generation cephalosporins. However, resistance to these antibiotics was greater than 95% among ESBL positive enterobacteriaceae isolates, with the exception of piperacillin–tazobactam. The current study found that less than a third of patients received active empiric antibiotics, implying a high rate of inactive empiric antibiotic use in enterobacteriaceae infections caused by ESBLs. It has been demonstrated that inactive empiric antibiotic therapy increases the risk of 30-day mortality in patients diagnosed with ESBL enterobacteriaceae bacteremia [2]. In addition, the duration before active antibiotic therapy was approximately 4 days, highlighting the length of time patients used inactive antibiotics. As a result, antimicrobial stewardship strategies that promote early and appropriate antibiotic administration to patients are recommended. Hospital pharmacists have an important role in promoting early and appropriate use of antibiotics for ESBL-positive enterobacteriaceae infections. Previous studies have demonstrated that hospital pharmacists contribute in promoting effective use of antibiotics and improving clinical outcomes [17, 18]. However, lack of training and support limit hospital pharmacists’ participation in antimicrobial stewardship services [19]. Therefore, training of hospital pharmacists and their involvement in antimicrobial stewardship programme is recommended [20, 21].
Although, more than a third of the isolates had in-vitro susceptibility to piperacillin–tazobactam, carbapenems accounted for more than 90% of the definitive antibiotics used in patients. Evidence from observational studies and meta-analysis have demonstrated that combination of beta-lactam beta-lactamase inhibitor are not inferior to carbapenems for the treatment of ESBL positive infections [1, 2, 22]. The widespread use of carbapenem for definitive therapy in patients with urinary tract infection and community-acquired infections poses a threat to the emergence and spread of carbapenem resistant infections. Beta-lactam beta-lactamase inhibitor combinations have been shown to be effective as carbapenem alternatives, particularly in patients with community-acquired infections [1] or urinary tract infections [23]. This finding highlights the importance of antimicrobial stewardship interventions aimed at reducing patients’ excessive carbapenem and preventing the emergence of carbapenem-resistant gram negative bacilli.
The study found a 13.6% in-hospital rate among patients hospitalised with infections caused by ESBL positive enterobacteriaceae. The mortality rate in this study is higher than that in a previous study conducted in the United States (US) [10], but lower than that in Singapore [22]. Admission to an intensive care unit was found to be significantly associated with an increased risk of mortality in patients, which was consistent with the findings of a previous study [10]. This is because patients admitted to the ICU typically have severe underlying infections often with septic shock and may be exposed to additional invasive procedures and devices. Previous research has established that advanced age, infections caused by K. pneumoniae, sepsis or septic shock, hospital-acquired infections, treatment with piperacillin–tazobactam and inactive empiric antibiotic therapy are all associated with increased mortality in patients diagnosed with ESBL producing enterobacteriaceae infections [2, 10]. However, these factors were not associated with mortality in the currents study, although, some factors, such as sepsis or septic shock and empiric therapy with piperacillin–tazobactam were associated with mortality in the univariate regression analysis. This could be explained by the small sample size. Therefore, a large multicentre study is being planned to examine the association between these factors and mortality in patients diagnosed with ESBL positive enterobacteriaceae infections. The current study revealed that presence of diabetes mellitus among patients diagnosed with ESBL positive enterobacteriaceae infections was independently associated with mortality. This may be due to immune impairment in patients with diabetes mellitus as a result of the hyperglycemic environment [24]. Therefore, adequate glycemic control is important to improve treatment outcomes among diabetes mellitus patients infected with ESBL-positive infection.
Due to some limitations, the findings should be interpreted with caution. This is a retrospective single-centre study with a relatively small sample size, which may affect the validity and generalizability of the results. However, the study sheds light on the treatments, mortality rate, and risk factors associated with mortality among patients diagnosed with ESBL-positive enterobacteriaceae infections in Malaysia. A large multicentre study is recommended to investigate treatment approaches used and to identify potential antimicrobial stewardship service opportunities.
Conclusions
There is a high rate of inactive empiric antibiotic use and excessive use of carbapenems for definitive therapy in ESBL-positive enterobacteriaceae infections including those with urinary tract infections and community-acquired infections. The mortality rate is relatively high among patients diagnosed with ESBL-positive enterobacteriaceae infections and is associated with intensive care unit admission and diabetes mellitus. Antibiotic stewardship is recommended to promote early active empiric antibiotic administration and to decrease carbapenem use in patients with ESBL positive enterobacteriaceae infections.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
Abbreviations
- CLSI:
-
Clinical and Laboratory Standards Institute.
- SPSS:
-
Statistical Package for the Social Sciences.
- ESBL:
-
Extended Spectrum Beta-Lactamase.
- ICU:
-
Intensive care unit
- OR:
-
Odds ratio
- AOR:
-
Adjusted odds ratio
- CI:
-
Confidence interval
References
Vardakas KZ, Tansarli GS, Rafailidis PI, Falagas ME (2012) Carbapenems versus alternative antibiotics for the treatment of bacteraemia due to Enterobacteriaceae producing extended-spectrum β-lactamases: a systematic review and meta-analysis. J Antimicrob Chemother 67(12):2793–2803
Gutiérrez-Gutiérrez B, Pérez-Galera S, Salamanca E, De Cueto M, Calbo E, Almirante B, Viale P, Oliver A, Pintado V, Gasch O, Martínez-Martínez L (2016) A multinational, preregistered cohort study of β-lactam/β-lactamase inhibitor combinations for treatment of bloodstream infections due to extended-spectrum-β-lactamase-producing Enterobacteriaceae. Antimicrob Agents Chemother 60(7):4159–4169
Gutierrez-Gutiérrez B, Rodríguez-Baño J (2019) Current options for the treatment of infections due to extended-spectrum beta-lactamase-producing Enterobacteriaceae in different groups of patients. Clin Microbiol Infect 25(8):932–942
Harris PN, Tambyah PA, Lye DC, Mo Y, Lee TH, Yilmaz M, Alenazi TH, Arabi Y, Falcone M, Bassetti M, Righi E (2018) Effect of piperacillin–tazobactam vs meropenem on 30-day mortality for patients with E. coli or Klebsiella pneumoniae bloodstream infection and ceftriaxone resistance: a randomized clinical trial. JAMA 320(10):984–994
Muhammed M, Flokas ME, Detsis M, Alevizakos M, Mylonakis E (2017) Comparison between carbapenems and β-lactam/β-lactamase inhibitors in the treatment for bloodstream infections caused by extended-spectrum β-lactamase-producing Enterobacteriaceae: a systematic review and meta-analysis. In: Open Forum Infectious Diseases, vol 4, no 2. Oxford University Press
Harris PN, Yin M, Jureen R, Chew J, Ali J, Paynter S, Paterson DL, Tambyah PA (2015) Comparable outcomes for β-lactam/β-lactamase inhibitor combinations and carbapenems in definitive treatment of bloodstream infections caused by cefotaxime-resistant Escherichia coli or Klebsiella pneumoniae. Antimicrob Resist Infect Control 4(1):14
Chang HJ, Hsu PC, Yang CC, Kuo AJ, Chia JH, Wu TL, Lee MH (2011) Risk factors and outcomes of carbapenem-nonsusceptible Escherichia coli bacteremia: a matched case–control study. J Microbiol Immunol Infect 44(2):125–130
Institute for Medical Research. National Antibiotic Resistance Surveillance Report 2017. Institute for Medical Research, Kuala Lumpur
Ministry of Health Malaysia. National antimicrobial guideline 2019. Ministry of Health Malaysia, Kuala Lumpur
Tamma PD, Han JH, Rock C, Harris AD, Lautenbach E, Hsu AJ, Avdic E, Cosgrove SE (2015) Carbapenem therapy is associated with improved survival compared with piperacillin–tazobactam for patients with extended-spectrum β-lactamase bacteremia. Clin Infect Dis 60(9):1319–1325
Chopra T, Marchaim D, Veltman J, Johnson P, Zhao JJ, Tansek R, Hatahet D, Chaudhry K, Pogue JM, Rahbar H, Chen TY (2012) Impact of cefepime therapy on mortality among patients with bloodstream infections caused by extended-spectrum-β-lactamase-producing Klebsiella pneumoniae and Escherichia coli. Antimicrob Agents Chemother 56(7):3936–3942
Wang R, Cosgrove SE, Tschudin-Sutter S, Han JH, Turnbull AE, Hsu AJ, Avdic E, Carroll KC, Tamma PD (2016) Cefepime therapy for cefepime-susceptible extended-spectrum β-lactamase-producing Enterobacteriaceae bacteremia. In: Open forum infectious diseases. May 1, vol 3, no 3, p ofw132. Oxford University Press
Groupa IH (2012) b-Lactam/b-Lactam inhibitor combinations for the treatment of bacteremia due to extended-spectrum b-lactamase–producing Escherichia coli: a post hoc analysis of prospective cohorts. Clin Infect Dis 54(2):167–174
Garner JS, Jarvis WR, Emori TG, Horan TC, Hughes JM (1998) CDC definitions for nosocomial infections, 1988. Am J Infect Control 16(3):128–140
Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, Bellomo R, Bernard GR, Chiche JD, Coopersmith CM, Hotchkiss RS (2016) The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA 315(8):801–810
Suetens C, Latour K, Kärki T, Ricchizzi E, Kinross P, Moro ML, Jans B, Hopkins S, Hansen S, Lyytikäinen O, Reilly J (2018) Prevalence of healthcare-associated infections, estimated incidence and composite antimicrobial resistance index in acute care hospitals and long-term care facilities: results from two European point prevalence surveys, 2016 to 2017. Eurosurveillance 23(46):1800516
Monmaturapoj T, Scott J, Smith P, Abutheraa N, Watson MC (2021) A systematic review and narrative synthesis of pharmacist-led education-based antimicrobial stewardship interventions and their effect on antimicrobial use in hospital inpatients. J Hosp Infect 115:93–116
Abubakar U, Syed Sulaiman SA, Adesiyun AG (2019) Impact of pharmacist-led antibiotic stewardship interventions on compliance with surgical antibiotic prophylaxis in obstetric and gynecologic surgeries in Nigeria. PLoS ONE 14(3):e0213395
Abubakar U, Tangiisuran B (2020) Nationwide survey of pharmacists’ involvement in antimicrobial stewardship programs in Nigerian tertiary hospitals. J Global Antimicrob Resist 21:148–153
Abubakar U, Muhammad HT, Sulaiman SA, Ramatillah DL, Amir O (2020) Knowledge and self-confidence of antibiotic resistance, appropriate antibiotic therapy, and antibiotic stewardship among pharmacy undergraduate students in three Asian countries. Curr Pharm Teach Learn 12(3):265–273
Abubakar U, Sha’aban A, Mohammed M, Muhammad HT, Sulaiman SA, Amir O (2021) Knowledge and self-reported confidence in antimicrobial stewardship programme among final year pharmacy undergraduate students in Malaysia and Nigeria. Pharm Educ 21:298–305
Ng TM, Khong WX, Harris PN, De PP, Chow A, Tambyah PA, Lye DC (2016) Empiric piperacillin–tazobactam versus carbapenems in the treatment of bacteraemia due to extended-spectrum beta-lactamase-producing Enterobacteriaceae. PLoS ONE 11(4):e0153696
Seo YB, Lee J, Kim YK, Lee SS, Lee JA, Kim HY, Uh Y, Kim HS, Song W (2017) Randomized controlled trial of piperacillin–tazobactam, cefepime and ertapenem for the treatment of urinary tract infection caused by extended-spectrum beta-lactamase-producing Escherichia coli. BMC Infect Dis 17(1):404
Casqueiro J, Casqueiro J, Alves C (2012) Infections in patients with diabetes mellitus: a review of pathogenesis. Indian J Endocrinol Metab 16(Suppl1):S27
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
AU and BT conceived the idea and designed the study. AU collected the data. AU and BT analyzed and interpreted the data. AU and FUK drafted the manuscript. BT, MHE, and SASS reviewed the manuscript draft. The author read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study protocol was approved by the IIUM Research Ethics Committee with the following reference number: IIUM/504/14/11/2/IREC 2020-092. Consent was waived due to the retrospective nature of the study.
Consent for publication
Not applicable.
Competing interests
The author declare that there is no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Abubakar, U., Tangiisuran, B., Elnaem, M.H. et al. Mortality and its predictors among hospitalized patients with infections due to extended spectrum beta-lactamase (ESBL) Enterobacteriaceae in Malaysia: a retrospective observational study. Futur J Pharm Sci 8, 17 (2022). https://doi.org/10.1186/s43094-022-00406-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43094-022-00406-8