Abstract
Background
Increased attention has been focused on the continuous development and improvement of mesalamine colonic specific delivery systems, for the effective treatment of inflammatory bowel diseases; thus enhancing therapeutic efficacy and reducing potential side effects. Mesalamine is a class IV drug, according to the Biopharmaceutics Classification System, used usually to treat inflammation associated with colon related diseases such as Crohn’s disease and ulcerative colitis.
Main text
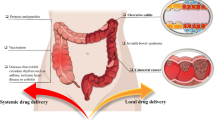
An ideal colon targeting system aims to deliver a therapeutic agent, selectively and effectively, to the colon. This system should ideally retain the drug release in the upper GI tract (stomach and small intestine); while trigger the drug release in the colon. Several approaches have been used to fabricate formulations to achieve a colon specific delivery of mesalamine such as; time dependent, pH responsive, enzymatic/microbial responsive and ultrasound mediated approaches. This overview outlines the recent advances in mesalamine-colon delivery approaches for the potential treatment of ulcerative colitis and Crohn’ disease.
Conclusion
A combined pH-time dependent delivery system can improve mesalamine colonic drug delivery via employing carriers capable of retarding mesalamine release in the stomach and delivering it at predetermined time points after entering the intestine. The existence of specific enzymes, produced by various anaerobic bacteria present in the colon advocates the advantage of designing enzyme sensitive systems and combining it with pH-time dependent system to improve mesalamine colonic delivery. The use of ultrasound has shown promises to effectively treat inflammatory bowel diseases.
Similar content being viewed by others
Background
Inflammatory bowel diseases represent inflammatory conditions that affect the gastrointestinal tract and cause over 50,000 deaths per year [1]. The most common inflammatory bowel diseases are ulcerative colitis and Crohn's diseases. The main difference between these two diseases is that Crohn's disease can affect any part of the gastrointestinal tract, while ulcerative colitis is specific to the colon. The currently available curing choices are not always effective and can cause serious side effects. Additionally, there is no permanent treatment available for inflammatory bowel diseases up to date, and patients need to stick to a lifelong drug treatment [2]. The recommended treatment depends on the disease location and its severity. Topical mesalamine, hydrocortisone or budesonide is recommended for patients with inflammation limited to the left colon. Oral mesalamine or sulfasalazine is recommended to be used in addition to the topical treatment with cases extended beyond the left colon. Oral prednisone or infliximab induction therapy is recommended for resistant patients. Intravenous steroids, infliximab or cyclosporine is recommended in severe cases. Topical mesalamine is suggested as a remission maintenance therapy for patients with ulcerative proctitis, while oral mesalamine is suggested for more extensive cases. Azathioprine, 6-mercaptopurine or infliximab agents are recommended in cases fail to maintain remission using mesalamine [3].
Mesalamine is a derivative of salicylic acid (5-amino salicylic acid [5-ASA]) and also known as mesalazine. It is usually used as a first line anti-inflammatory agent to act locally on colonic mucosa and reduce inflammation for the treatment colon related diseases, such as Crohn’s disease and ulcerative colitis [4, 5]. Mesalamine was discovered as the active moiety of sulfasalazine, where it is bound to sulfapyridine (inactive moiety), via an azo bond (cleaved by azoreductase enzyme present in the GIT). Sulfapyridine is believed to be responsible for the adverse and unwanted effects associated with sulfasalazine [6, 7]. The mechanism of action of mesalazine is not fully clear in inflammatory bowel diseases, but it is believed to be a topical effect at the inflammation site via the direct interaction with the damaged epithelial cells. It is then metabolized to the inactive form (N-acetyl-5-ASA) by N-acetyltransferase 1 and excreted in the urine [8]. This justify the failure of oral administration of pure 5-ASA in inflammatory bowel diseases and necessitates the development of an efficient delivery system capable of retarding its release in the upper GI tract (stomach and small intestine); while triggering its release at the inflammation site [9]. Mesalamine is categorized as a BCS class IV drug (low solubility, low permeability) according to the Biopharmaceutics Classification System. It is slightly soluble in water and poorly absorbed following its oral administration (approximately 25%) [10]. This fact necessitates the enhancement of its dissolution and absorption rates in order to increase its bioavailability. The development of colon specific drug delivery systems of mesalamine has gained increased attention for the effective treatment of inflammatory bowel diseases whereby high local concentration can be achieved; thus reducing side effects and enhancing therapeutic efficacy [11]. An ideal delivery system should protect the drug and retard its release in the upper GI tract (stomach and small intestine); while permitting its release in the colon [12]. Various approaches have been used to develop colonic delivery systems of mesalamine such as; time dependent, pH responsive, prodrug and enzymatic/microbial responsive approaches. Most of the oral marketed mesalamine products utilizes a pH dependent coat, which is capable to retard 5-ASA release in the stomach and permit its release at the higher intestinal pH. Examples of such systems include; the employment of Eudragit® S resin coat (such as in Asacol® and Lialda®) that disintegrates at high intestinal pH (more than 7), to trigger mesalamine release at the terminal ileum or cecum. Another example is the use of Eudragit® L resin coat (such as in Apriso® and Claversal®) that disintegrates at pH more than 6, to trigger 5-ASA release at the jejunum, terminal ileum and colon. Some of these systems also use additional polymeric matrices (such as in Lialda® and Apriso®) designed to further control the drug release rate and deliver mesalamine at predetermined time points after entering the intestines. Pentasa® is an example of pH independent oral marketed mesalamine, which is usually taken up to 4 grams/day and mesalamine is released slowly from the ethylcellulose coated tablets [13,14,15,16,17,18]. This review summarizes the recent advances in mesalamine-colon drug delivery based on time dependent, pH responsive, enzyme sensitive and ultrasound approaches.
Main Text
Time Dependent and pH Responsive Approaches
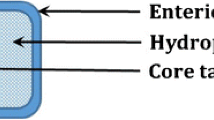
The large variation of gastric retention time is the main obstacle of sustained or delayed oral delivery as it is difficult to accurately predict the drug delivery time to the colon. The pH approach usually employs polymers that retard drug release in the stomach and permit its release at the higher intestinal pH, where the polymer can dissolve or swell. A pH-responsive carrier can enhance the oral controlled delivery of mesalamine in two ways; 1) the pH-triggered swelling of a carrier may result in fast drug release and high drug concentration gradient. 2) The pH-responsive swelling may enhance the carrier’s mucoadhesion ability; thus improving the drug absorption [19]. However, a colon specific delivery is difficult to be achieved using the pH strategy alone due to inter/intra pH variations and pH similarity between small intestine and colon [20]. The small variability of the small intestine transit time (3 ± 1 hours) advocates the advantage of developing a combined pH-time dependent delivery system to improve the site specificity. This system employs carriers capable of preventing the drug release in the stomach and delivering it at predetermined time points after entering the intestines [21]. Mirabbasi et al. [22] synthesized mesalamine loaded nanoparticles, based on polyurethane-chitosan graft copolymer, as a time-delayed colon drug delivery system. The in vitro release studies had proven that the nanocarrier based formulation was able to control mesalamine release over 72 hours with 92.19% cumulative release is being achieved. However, around 55% of the loaded drug were released within 8 hours. The release kinetics studies had shown that the release data were best fitted to first order kinetics. It was concluded that the prepared carrier was successful to sustain the drug release with no burst effect. Rehman et al. [23] prepared a carrier functionalized with long hydrophobic chains, composed of mesoporous silica SBA-15 and glycidyl methacrylate organo bridges, as a controlled release system of mesalamine. The surface area studies had indicated the successful immobilization of glycidyl methacrylate organo bridges onto the mesoporous surface; as the surface area has dropped in the functionalized carrier from 1311.8 to 494.20 m2g− 1. Although of the decreased surface area, the modified carrier had shown a higher drug loading (29% compared to 19% in the unmodified silica). This was explained by the increased hydrophobicity due to the inserted glycidyl methacrylate organo bridges. In vitro release studies were performed at different pH values (1.2, 6.8 and 7.2) for 75.5 hours. The release studies had demonstrated the ability of the modified carrier to release 5-ASA preferentially at high pH value. 6% of loaded 5-ASA was released at pH 1.2 after 2 hours compared to 8% and 11% at pH 6.8 and pH 7.2 respectively. Around 19% and 14% drug release were obtained at pH 7.2 after 6 and 8 hours respectively compared to less than 10% at pH 1.2 and pH 6.8 at the same time points. Pawar et al. [24] prepared and evaluated matrix tablets of mesalamine for colon triggered delivery, composed of Eudragit RSPO and/or RLPO as rate-controlling matrices, and coated with different concentration of anionic pH dependent copolymers (Eudragit S100). 9 formulations were prepared using different concentrations of Eudragit RSPO, Eudragit RLPO and Eudragit S100. In vitro release studies were performed sequentially in pH 1.2 buffer for 2 hours, pH 6.8 for 3 hours and pH 7.4-with/without cecal content for 19 hours. The In vitro release studies were also conducted for an oral marketed product of mesalamine (Octasa ® MR) and compared with the optimized formulation, which consist of Eudragit RLPO and coated with 1% w/v Eudragit S100. The optimized formulation exhibited a more sustainable and lower drug cumulative release (90.9% within 24 hours compared to 98.4% from the marketed product within 18 hours). It was concluded that the optimized formulation, was able to retard the drug release at the low pH and control it at intestinal pH, which makes it a promising colon-specific delivery system. Zhang et al. [25] investigated the development a colon delivery system, using melt-extruded granules of mesalamine and Eudragit® FS. The developed product exhibited higher physical strength, smaller pore size and lower porosity compared with the conventionally prepared granules. In vitro release studies were carried out sequentially at pH 1.2 for 2 hours, pH 6.8 for 4 hours and pH 7.4 for 6 hours. The prepared granules remained intact and the release mechanism of 5-ASA was controlled by diffusion within the first six hours due to the fact that Eudragit® FS is insoluble at pH 1.2 and pH 6.8. The granules size diminished gradually, when the Eudragit® FS started to dissolve at pH 7.4 forming a gel-like layer around the granule the drug release became controlled by diffusion and erosion. The drug release was found to decrease with granule size due to the decrease surface area. The drug release profile was found to be stable after one month storage at 40°C/75% relative humidity and 60°C/without humidity; as no change was observed at both conditions compared to the initial profile. The drug release was found to be increased with the drug loading (10, 20 and 30% respectively) within the first 6 hours (at pH 1.2 and pH 6.8), while decreased at pH 7.4 and this was attributed to the more micro pH environment induced by 5-ASA dissolved within the granules. The release studies had also showed that the melt-extruded granules exhibited a delayed and pH-dependent 5-ASA release compared to the conventionally compressed granules. This was explained by the higher porosity of the conventional granules, which was confirmed using scanning electron microscopy. Kumar et al. [10] investigated the development of a multiparticulate oral formulation of mesalamine, coated with Eudragit S100, as a potential colon targeted delivery system. The drug was encapsulated in gellan gum-locust bean gum-sodium alginate beads by inotropic gelation method. A lower In vitro release was observed for The Eudragit S100 coated formulations compared to the uncoated ones within the first five hours (at pH 1.2 and pH 6.5). Gamma scintigraphic studies were performed for the optimized formulation in rabbits. the scintigraphic images revealed that the delivery systems remained intact in the stomach, little drug release had occurred in the small intestine and considerable spreading of radioactivity had occurred once the system entered the colon. This considerable change was attributed to the degradation of gellan gum via the colonic bacteria. The In vivo studies also showed that the formulation residence time was more than 12 hours in the colon. Patole et al. [26] investigated the development of a combined pH-microbial sensitive delivery system based on enteric coated hydroxypropyl methylcellulose capsules filled with mesalamine-loaded alginate microspheres, which was prepared using an emulsion crosslinking method. The optimized microspheres (on the basis of maximum entrapment efficiency) were selected for encapsulation and further studies. Different weights (10, 20 and 30 mg) had been used an enteric coat. The 30 mg coat formulation was able to retard mesalamine release in simulated intestinal fluid for 6 hours, therefore it was selected for testing in simulated colonic fluid in the presence of rat colonic content. The drug release was enhanced considerably in the presence of the colonic content (around 92% released within 10 hours compared to 65% in the absence of the colonic content at the same time point). This had been explained by the microbial degradation of alginate. In another similar study, Patil et al. [27] investigated the preparation mesalamine-loaded microspheres and concluded that the appropriate inclusion of pH dependent and independent polymers (Eudragit S-100 and sodium alginate respectively) was successful to control the drug release and achieve a colon triggered delivery. Kar et al. [9] also employed an emulsification solvent diffusion method to prepare mesalamine microspheres, coated with methacrylic acid copolymers, as a controlled delivery system for the potential treatment of inflammatory bowel diseases. In vivo biodistribution of the optimized microsphere formulation was investigated in the GIT of mice and compared with pure 5-ASA solution. The optimized formulation exhibited a higher AUC0–t (around 2.6 times) in colon compared to the pure drug solution. The highest mesalamine concentration was observed in the colon for the microsphere preparation after 8 hours and negligible amount observed in the other parts of the GIT. In contrast, the highest drug concentration was observed in the small intestine for the pure drug solution after 8 hours. Pawar et al. [28] developed a pulsatile controlled release system, employing a pH-time dependent approach, to achieve a colon-specific controlled delivery of mesalamine. In this work, they developed an enteric coated capsule, composed of a water soluble cap and an insoluble body, where the drug formulation (mesalamine coated with Eudragit L-100 and S-100 copolymers) filled within the body and separated from the cap by a hydrogel plug. In this system, the capsule enteric coat dissolves upon reaching small intestine and the hydrogel plug starts to swell in a time controlled manner accounts the small intestinal transit time. Finally, the plug ejects and permits the formulation delivery to the colon, where the drug release is further controlled up to 24 hours by the pH-responsive coat. Parmar et al. [29] formulated an enteric coated bilayer (immediate and sustained release layers) tablets of mesalamine using HPMC K4M and HPMC K15M polymers for the sustained release layer. The optimized formulation was coated for different times (20, 40 and 60 min) using Eudragit S-100. The In vitro release studies revealed that the 60 minutes coated formulation was the only one successful in preventing 5-ASA release in the upper GI tract (stomach and small intestine). This was contributed to the sufficient coat thickness achieved for this formulation. The In vivo release studies in rabbits had also confirmed this finding; as the plasma drug concentration was just detectable after 6 hours of administration for the bilayer tablets and 0.5 hour for the conventional immediate release tablet. The half life of the developed bilayer tablets was found to be 20 hours compared to 1 hour in the immediate release tablet, which indicated the sustained 5-ASA release from the bilayer tablets. The roentogenographic images had also confirmed that the developed bilayer tablet remained intact in the upper GI tract and required more than 4 hours to reach the colon.
Microbial/Enzyme Sensitive Approach
Enzymes are biological catalysts that are highly specific and selective for their substrates. They play a crucial role in chemical and biological processes within the human cells. The ability to catalyze reactions at low temperatures, in aqueous environments and at different pH values, makes them suitable to be involved in drug delivery and biomedical application systems [30]. The existence of specific enzymes, produced by various anaerobic bacteria present in the colon, such as azoreductase, galactosidase, nitroreductase, glucoronidase and xylosidase, advocates the advantage of designing enzyme sensitive systems for colon specific drug delivery [11]. Jin et al. [31] investigated the development of pH–enzyme sensitive microparticles, based on mesalamine-loaded chitosan microparticles coated with methacrylic acid copolymers, as a specific delivery system for the treatment of ulcerative colitis. In vitro release experiments were carried out sequentially in buffers of pH 1.2 (for 2 hours), pH 7.4 (for 3 hours) and pH 6.8-with cecal content (for 20 hours). The release studies demonstrated the ability of the prepared particles to effectively retard the drug release in the simulated gastric and intestinal buffers (the first 5 hours), and control the drug release at pH 6.8 in the presence of 4% rat cecal content. Around 3% of the loaded mesalamine was released from the developed microparticles compared to complete mesalamine release from the conventional suspension at the same time point. Around 70% of the loaded mesalamine was released over 20 hours in the presence of the colonic contents. The pharmacokinetics studies found that a higher AUC0–t (around 72 μg·h/mL) and longer half-life (16 hours) was obtained for the developed particles compared to the drug suspension (41 μg·h/mL and 3 hours respectively). Those findings were confirmed in the biodistribution studies; as a higher AUC0–t was observed for the developed particles in the colon compared to the drug suspension. As well as, the highest drug concentration was observed in the colon for the developed particles while observed in the small intestine for the suspension after 8 hours of drug administration. Jaiswal et al. [32] employed an ionotropic gelation method to prepare dual crosslinked mesalamine microparticles, using different ratios of chitosan and pectin, as a potential enzyme-sensitive delivery system. Swelling and In vitro release studies were performed in simulated gastric (pH 1.2), intestinal (pH 6.8) and colonic (pH 7.2) fluids. All formulations revealed low swelling at pH 1.2, higher swelling at pH 6.8 and further intense swelling increase observed at pH 7.2. The microparticles exhibited a negligible drug release during 2 hours at pH 1.2 compared to the higher pH values. A higher release was observed within 3 hours at pH 6.8 and a further increase observed at pH 7.2 during 18 hours. Further release studies were performed in the presence of rat cecal content, where the complete degradation of the polymeric carrier by colonic enzymes was observed. The presence of high concentrations of polysaccharidase enzymes in the colon, suggests the use of polysaccharides as drug carriersfor colon targeted drug delivery. However, mesalamine has previously reported to affect the balance of the colonic microflora [33], which acts as a release trigger for polysaccharide based systems. Under these conditions, there is a possibility for the failure of the polysaccharide-based oral delivery system after giving the first dose. Such failure has been previously reported as a result of the disturbed microflora level [34]. To overcome this problem, Kaur et al. [35] developed a microbially triggered mesalamine microshperes using natural polysaccharides (guar gum and xanthan gum) and combined with probiotics in a single dosage form, where guar gum and xanthan gum act as prebiotics. It was concluded that this developed combined system is clearly superior compared with systems based on delayed drug release and using synthetic polymers as a pH sensitive coat. Thakur et al. [36] also employed the use of probiotics to produce spray dried microparticles, consist of mesalamine loaded eudragit S-100 embedded in probiotic biomass, as a combined targeted anti-inflammatory approach for the potential effective treatment of ulcerative colitis. The prepared formulation exhibited a controlled delivery of mesalamine and demonstrated the ability to reduce to reduce inflammation and side effects associated with conventional treatment of ulcerative colitis. In another study, Mohanta et al. [37] investigated the co-administration of probiotics, with mesalamine (coated with guar gum and Eudragit S100) and spray dried modified apple polysaccharide minitablets, for the potential treatment of ulcerative colitis induced in rats. The experimental studies showed that the maximum therapeutic efficacy was attained with the co-administration of the two prepared minitablets and probiotics compared to that with the single administration of mesalamine minitablets, modified apple polysaccharide minitablets or probiotics alone. Kandula et al. [38] synthesized CLX-103 as a novel prodrug conjugate of mesalamine, eicosapentaenoic acid and caprylic acid, to achieve a colon targeted mesalamine delivery with enhanced safety and therapeutic efficacy. In vitro and In vivo studies showed that CLX-103 was biochemically stable in simulated gastric fluid and underwent enzymatic hydrolysis in the intestinal environment to releases mesalamine, which stayed a longer period of time in the large intestine compared to sulfasalazine. Cesar et al. [39] synthesized a polymeric prodrug of mesalamine, composed of chondroitin sulfate linked with mesalamine, as a potential colon targeted drug delivery system for the treatment of inflammatory bowel diseases. The synthesized polymeric prodrug exhibited a colon mucoadhesion effect as desired, which makes it promising for targeting mesalamine at the colon. Walz et al. [40] studied the enzymatic degradability of acetylated inulin, which was prepared as a potential encapsulation material to achieve a colonic targeted delivery of mesalamine. Anindya et al. [41] synthesized xylan-mesalamine conjugate as a promising colon triggered delivery system. Xylan was isolated from pineapple stem waste. The In vitro studies showed that prepared conjugate was successful to retain mesalamine delivery in simulated upper GI fluid, while release it quickly in simulated colonic fluid-with rat cecal content. The In vivo studies concluded that the prepared formulation exhibited a delayed mesalamine delivery and lower bioavailability compared to free mesalamine, which makes it a good candidate as a potential colon-specific delivery system. In another study Souza et al. [42] reported the successful development of mesalamine loaded microshperes, based on xylan, using water-in-water emulsion technique.
Ultrasound Mediated Approach
An increased attention has been raised recently toward the use of ultrasound at low frequency (≤100 kHz), for the effective treatment of inflammatory bowel diseases, as a physical enhancer to facilitate and accelerate the drug delivery process as well as increase patient compliance and acceptance; as a result of the decreased enema dosing frequency and required mucosal exposure time [43, 44]. Ultrasound Mediated GI delivery approach was firstly reported in the mid-1980s by Kost and Langer in their patent application concerned with transbuccal drug delivery [45]. This approach employs a low frequency ultrasound to trigger drug delivery at lower GIT via causing transient cavitation, which produce microjets to enhance drug permeation through gastrointestinal mucosa [46]. Schoellhammer et al. [47] reported the development a hand-held device, which use a low frequency ultrasound, as a reversible and painless method to enhance mesalamine delivery in the treatment of ulcerative colitis and Crohn’ disease. This device was co-administered superficially into the rectum of Yorkshire pigs with a mesalamine enema. It was found that a one minute exposure was able to enhance mesalamine delivery 22 times compared to that with conventional enema treatment. In another study, they investigated the colonic delivery of RNA molecules in living mice and it was concluded that ultrasound mediated approach has successfully enhanced intracellular delivery of mRNAs and siRNAs to the mice colon [48].
Conclusion
Mesalamine is a BCS class IV drug usually used as a first line anti-inflammatory agent to treat ulcerative colitis and Crohn’s diseases. The currently available treatments are not always effective and can cause serious side effects. The development of mesalamine colonic targeted delivery has gained increased attention to enhance the therapeutic efficacy and reduce potential side effects. Several strategies have been designed to develop controlled delivery systems of mesalamine such as; time dependent, pH responsive, enzymatic/microbial responsive and ultrasound mediated approaches. A combined delayed-pH dependent and enzyme sensitive drug delivery system based on nanocarriers can be designed as a promising oral delivery system to further increase the colon-selective delivery of mesalamine in treating ulcerative colitis and Crohn’ disease. Such controlled drug delivery system can demonstrate the ability to retard the drug release at the upper GI tract (stomach and small intestine) and deliver 5-ASA, effectively and selectively, to the inflammation site; thus reducing side effects and dosing frequency, enhancing the therapeutic efficacy and avoiding drug degradation. The system stability, methodology simplicity and safety of materials used in fabricating this system need to be addressed exclusively; for the successful translation of such approach into industrial scale production and clinical practice. The employment of ultrasound mediated approach in the rectally administered mesalamine can be promising to greatly enhance the drug delivery process and decrease problems associated with conventional enemas delivery such as; patient acceptance, dosing frequency and required mucosal exposure time. However, further and more research works need to be done in this field.
Availability of data and materials
Data and material are available upon request.
Abbreviations
- 5-amino salicylic acid:
-
5-ASA
- Biopharmaceutics Classification System:
-
BCS
- Gastrointestinal:
-
GI
- Hydroxypropyl Methylcellulose:
-
HPMC
- Gastrointestinal Tract:
-
GIT
- Ribonucleic Acid:
-
RNA
- Messenger Ribonucleic Acids:
-
mRNAs
- Small Interfering Ribonucleic Acids:
-
siRNAs
References
Garrett W, Howitt M (2019) Methods of treating inflammatory bowel disease and parasite infection. U.S. Patent Application No. 16/074,934.
Zeeshan M, Ali H, Khan S, Khan SA, Weigmann B (2019) Advances in orally-delivered pH-sensitive nanocarrier systems; an optimistic approach for the treatment of inflammatory bowel disease. Int J Pharm 558:201–214
Ham M, Moss AC (2012) Mesalamine in the treatment and maintenance of remission of ulcerative colitis. Expert Rev Clin Pharmacol 5(2):113–123
Desai SA, Kale R (2019) Method development and validation of mesalamine in pharmaceutical dosage form: a review. Int J Pharma Biol Sci Arch 7(3)
Badhana S, Garud N, Garud A (2013) Colon specific drug delivery of mesalamine using eudragit S100-coated chitosan microspheres for the treatment of ulcerative colitis. Int Current Pharma J 2(3):42–48
Sonu I, Lin MV, Blonski W, Lichtenstein GR (2010) Clinical pharmacology of 5-ASA compounds in inflammatory bowel disease. Gastroenterology Clinics 39(3):559–599
Peppercorn MA (1984) Sulfasalazine: pharmacology, clinical use, toxicity, and related new drug development. Ann Intern Med 101(3):377–386
Dahl J, Gray MJ, Bazopoulou D, Beaufay F, Lempart J, Koenigsknecht MJ et al (2017) The anti-inflammatory drug mesalamine targets bacterial polyphosphate accumulation. Nature Microbiol 2(4):1–5
Kar N (2019) Formulation Design and Characterization of Colon-targeted Mesalamine Microspheres and their Biodistribution Potential Study in Mice. Asian Journal of Pharmaceutics (AJP): Free full text articles from Asian J Pharm 12(04).
Kumar M, Kaushik S, Saini V, Kumar C, Bhatt S, Malik A et al (2018) Formulation development and evaluation of colon targeted beads of mesalamine. J Drug Des Res 5(2):1067
Amidon S, Brown JE, Dave VS (2015) Colon-targeted oral drug delivery systems: design trends and approaches. Aaps Pharmscitech 16(4):731–741
Mehta R, Chawla A, Sharma P, Pawar P (2013) Formulation and in vitro evaluation of Eudragit S-100 coated naproxen matrix tablets for colon-targeted drug delivery system. J Adv Pharm Technol Res 4(1):31–41
Brunner M, Greinwald R, Kletter K, Kvaternik H, Corrado M, Eichler H et al (2003) Gastrointestinal transit and release of 5-aminosalicylic acid from 153Sm-labelled mesalazine pellets vs. tablets in male healthy volunteers. Aliment Pharmacol Ther 17(9):1163–1169
Layer PH, Goebell H, Keller J, Dignass A, Klotz U (1995) Delivery and fate of oral mesalamine microgranules within the human small intestine. Gastroenterology 108(5):1427–1433
Lichtenstein G, Kamm M (2008) 5-aminosalicylate formulations for the treatment of ulcerative colitis–methods of comparing release rates and delivery of 5-aminosalicylate to the colonic mucosa. Aliment Pharmacol Ther 28(6):663–673
Yang LP, McCormack PL (2011) MMX® Mesalazine. Drugs 71(2):221–235
Lawlor G, Ahmed A, Moss AC (2010) Once-daily mesalamine granules for ulcerative colitis. Expert review of clinical immunology 6(4):521–526
Rasmussen S, Bondesen S, Hvidberg E, Hansen SH, Binder V, Halskov S et al (1982) 5-aminosalicylic acid in a slow-release preparation: bioavailability, plasma level, and excretion in humans. Gastroenterology 83(5):1062–1070
Wang X, Zhang Q (2012) pH-sensitive polymeric nanoparticles to improve oral bioavailability of peptide/protein drugs and poorly water-soluble drugs. Eur J Pharm Biopharm 82(2):219–229
Dangi AA, Divya J (2013) Formulation and evaluation of colon targeted drug delivery system of Levetiracetam using pectin as polymeric carrier. J App Pharma Sci 3(1):78
Singh A, Sharma A (2014) Novel approaches for colon targeted drug delivery system. Int J Res Dev Pharmacy Life Sci 3(2):877–886
Mirabbasi F, Dorkoosh FA, Moghimi A, Shahsavari S, Babanejad N, Seifirad S (2017) Preparation of Mesalamine Nanoparticles Using a Novel Polyurethane-Chitosan Graft Copolymer. Pharma Nanotechnol\ 5(3):230–239
Rehman F, Rahim A, Airoldi C, Volpe PL (2016) Preparation and characterization of glycidyl methacrylate organo bridges grafted mesoporous silica SBA-15 as ibuprofen and mesalamine carrier for controlled release. Mater Sci Eng C Mater Biol Appl 59:970–979
Pawar PK, Gautam C (2016) Design, optimization and evaluation of mesalamine matrix tablet for colon drug delivery system. J Pharma Invest 46(1):67–78
Zhang F (2016) Melt-extruded Eudragit® FS-based granules for colonic drug delivery. AAPS PharmSciTech 17(1):56–67
Patole VC, Pandit AP (2018) Mesalamine-loaded alginate microspheres filled in enteric coated HPMC capsules for local treatment of ulcerative colitis: in vitro and in vivo characterization. Journal of Pharmaceutical Investigation 48(3):257–267
Patil A, Pawar P, Gharge V, Doltade U, Doijad R (2018) Mesalamine-loaded mucoadhesive microsphere for colon drug delivery system: Effect of process variables and in vitro characterization. Int J Pharma Invest 8(2):74–82
Pawar P, Varsha G (2018) Formulation and Evaluation of Mesalamine Loaded pH Dependent Colon Specific Pulsatile Drug Delivery System. Curr Res Pharma Sci:244–253
Parmar C, Parikh K, Mundada P, Bhavsar D, Sawant K (2018) Formulation and optimization of enteric coated bilayer tablets of mesalamine by RSM: In vitro–In vivo investigations and roentogenographic study. J Drug Delivery Sci Technol 44:388–398
Chandrawati R (2016) Enzyme-responsive polymer hydrogels for therapeutic delivery. Exp Biol Med 241(9):972–979
Jin L, Ding YC, Zhang Y, Xu XQ, Cao Q (2016) A novel pH-enzyme-dependent mesalamine colon-specific delivery system. Drug Des Devel Ther 10:2021–2028
Jaiswal M, Lanjhiyana S (2018) Fabrication and Evaluations of Dual Crosslinked Mesalamine containing Pectin-Chitosan gel micro beads for controlled and targeted colon delivery. Res J Pharm Technol 11(11):4797–4804
Kaufman J, Griffiths TA, Surette MG, Ness S, Rioux KP (2009) Effects of Mesalamine (5-5-Aminosalicylic Acid) on Bacterial Gene Expression. Inflamm Bowel Dis 15(7):985–996
Krishnaiah Y, Seetha Devi A, Nageswara Rao L, Bhaskar Reddy P, Karthikeyan R, Satyanarayana V (2001) Guar gum as a carrier for colon specific delivery; influence of metronidazole and tinidazole on in vitro release of albendazole from guar gum matrix tablets. J Pharm Pharm Sci 4(3):235–243
Kaur R, Gulati M, Singh SK (2017) Role of synbiotics in polysaccharide assisted colon targeted microspheres of mesalamine for the treatment of ulcerative colitis. Int J Biol Macromol 95:438–450
Thakur V, Singh A, Joshi N, Mishra N (2019) Spray Dried Formulation of Mesalamine Embedded with Probiotic Biomass for the Treatment of Ulcerative Colitis: In-Vitro and In-Vivo studies. Drug Dev Ind Pharm 45(11):1807–1820
Mohanta S, Singh SK, Kumar B, Gulati M, Kumar R, Yadav AK et al (2019) Efficacy of co-administration of modified apple polysaccharide and probiotics in guar gum-Eudragit S100 based mesalamine mini tablets: A novel approach in treating ulcerative colitis. Int J Biol Macromol 126:427–435
Kandula M, Kumar KS, Palanichamy S, Rampal A (2016) Discovery and preclinical development of a novel prodrug conjugate of mesalamine with eicosapentaenoic acid and caprylic acid for the treatment of inflammatory bowel diseases. Int Immunopharmacol 40:443–451
Cesar AL, Abrantes FA, Farah L, Castilho RO, Cardoso V, Fernandes SO et al (2018) New mesalamine polymeric conjugate for controlled release: Preparation, characterization and biodistribution study. Eur J Pharm Sci 111:57–64
Walz M, Hagemann D, Trentzsch M, Weber A, Henle T (2018) Degradation studies of modified inulin as potential encapsulation material for colon targeting and release of mesalamine. Carbohydr Polym 199:102–108
Anindya AL, Oktaviani RD, Praevina BR, Damayanti S, Kurniati NF, Riani C et al (2019) Xylan from Pineapple Stem Waste: a Potential Biopolymer for Colonic Targeting of Anti-inflammatory Agent Mesalamine. AAPS PharmSciTech 20(3):112
Souza BS, Marcelino HR, Alexandrino F, Urtiga SC, Silva KC, Soares DC et al (2019) Water-in-Water Emulsion as a New Approach to Produce Mesalamine-Loaded Xylan-Based Microparticles. App Sci 9(17):3519
Schoellhammer CM, Traverso G (2016) Low-frequency ultrasound for drug delivery in the gastrointestinal tract:1045-1048.
Maloney E, Hwang JH (2017) Intra-luminal focused ultrasound for augmentation of gastrointestinal drug delivery. Ann Transl Med 5(7):178
Kost J, Langer RS (1990) Ultrasound enhancement of transbuccal drug delivery. U.S. Patent No 4,948,587.
Sonis S (2017) Ultrasound-mediated drug delivery. Oral Dis 23(2):135–138
Schoellhammer CM, Schroeder A, Maa R, Lauwers GY, Swiston A, Zervas M et al (2016) Low-frequency ultrasound for the delivery of therapeutics to the gastrointestinal tract. J Acoust Soc Am 139(4):2091–2092
Schoellhammer CM, Lauwers GY, Goettel JA, Oberli MA, Cleveland C, Park JY et al (2017) Ultrasound-mediated delivery of RNA to colonic mucosa of live mice. Gastroenterology 152(5):1151–1160
Acknowledgements
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
MB organized the project and the article writing. RB is a student under MB supervision who prepared the manuscript. MB and RB contributed to the writing style and proof reading. Both authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare they have no competing interest regarding this work.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Bayan, M.F., Bayan, R.F. Recent advances in mesalamine colonic delivery systems. Futur J Pharm Sci 6, 43 (2020). https://doi.org/10.1186/s43094-020-00057-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43094-020-00057-7