Abstract
Hydatid cyst is a parasitic infection most commonly localized in the liver. They may not be diagnosed early because they remain asymptomatic at small sizes and may reach large sizes at the time of diagnosis. In this situation, compression symptoms may occur and they may present with serious complications such as rupture and anaphylactic shock, which are rare. Treatment methods are determined by classification according to the imaging techniques used in the diagnosis. In the present case, echinococcal cysts originating from segments 5, 6, and 7 in the right lobe of the liver, reaching 35 cm in diameter, caused compression symptoms. The diagnosis was made by abdominal tomography showing characteristic daughter vesicles and calcified cystic wall. The patient underwent pericystectomy and had an uneventful postoperative course with no recurrence in the 5-year follow-up.
Similar content being viewed by others
Introduction
Echinococcal disease, also known as hydatid cyst, is a zoonotic infection caused by Echinococcus Granulosus and Echinococcus Multilocularis. Echinococci are most commonly found in organs such as the liver (70%), lung (20%), brain, spleen, kidney, and heart and can cause various dysfunctions. Since echinococcal cysts grow slowly, they may not show early symptoms and remain asymptomatic for 10–15 years [1].
The diagnosis of hydatid cyst can be made with radiologic imaging, serologic and immunologic laboratory studies. Ultrasonography (USG), computed tomography (CT), and magnetic resonance imaging (MRI) are highly effective in detecting hepatic hydatid cysts [2, 3].
The treatment of the echinococcal disease depends on the type, size, and location of the cyst, the presence of complications, and the experience of the team. Treatment options include percutaneous treatments, surgical procedures, anti-parasitic drugs, and follow-up without intervention [4]. Curative treatment is achieved by complete surgical removal of the cyst regardless of its location. In this article, we present a patient who underwent surgery for a giant hydatid cyst extending into the abdomen.
Case presentation
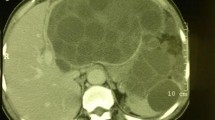
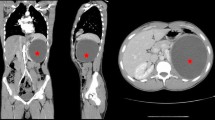
A 50-year-old male patient engaged in animal farming in southeastern Turkey was referred to our clinic with a giant hydatid liver cyst. He had a history of abdominal distension and intermittent pain for 2 years. His medical history was unremarkable. Physical examination revealed no signs of irritation except for severe abdominal distension and minimal tenderness. Laboratory tests revealed leukocyte: 7.1 × 103/UL (4.3–10.3), eosinophil: 6.5% (0.9–6), aspartate aminotransferase: 82 U/L (5–34), alanine aminotransferase: 129 U/L (0–55), gamma glutamyl transferase: 65 U/L (9–64), alkaline phosphatase: 101 U/L (40–150), total bilirubin: 0.84 mg/dL (0.2–1.2), Ca 19–9: 7.3 U/mL (0–35), HBsAg: 3406 S/CO. Contrast-enhanced upper abdominal CT scan showed a thin-walled, lobulated contoured lesion compatible with hydatid cyst, and hypodense areas of daughter vesicles. It was approximately 35 × 31 × 18 cm in size, extending from the midline to the left and inferiorly to the pelvis, located in the right lobe segments 6–7 of the liver, and causing marked distension (Fig. 1). In addition, a cystic lesion with similar characteristics measuring approximately 6 × 4 cm in size was observed in the subcapsular area of liver segments 5–8 (Fig. 2a, b). The large cyst was compressing the adjacent intestinal loops, stomach, and pancreas and pushing them to the left. There was also minimal anterior compression of the left kidney. CT scan of the lower abdomen revealed multiple multivesicular hydatid cyst compatible lesions in the pelvis, the largest of which was 10 × 8 cm (Fig. 3). Thorax CT did not reveal any lesion related to hydatid cyst. The patient's clinical and radiologic data were evaluated and surgery was planned. The patient underwent pericystectomy. Laparotomy was performed and two separate cystic lesions originating from the liver were observed. First, cystic lesions were punctured. Approximately 500 cc of 3% NaCl was injected into the cystic lesions after no bile contamination was observed in the aspirated cyst contents. After waiting for approximately 15 min, the apex of the cysts was opened and the cyst contents were aspirated (Fig. 4). The daughter vesicles inside the cyst were removed after aspiration (Fig. 5). Approximately 10 lt of cyst fluid and its elements were aspirated from the large cystic lesion (Fig. 6). Bile leakage was observed in several places in this cystic lesion. The leakage sites were closed with monofilament suture. The same procedure was applied to the second lesion in the liver. The defects were closed with omentoplasty. Later, some of the cystic lesions in the pelvis were completely excised, while some cystic lesions showing dense adhesion to the rectal wall were emptied and partially excised due to the risk of perforation (Fig. 7). After the procedure was completed, the peritoneal cavity was washed twice with 3% NaCl. No bile leakage was observed in the postoperative follow-up. Albendazole 2 × 400 mg was started on the second postoperative day. He used it regularly for 2 years. He was discharged without complications on the 10th postoperative day and there was no recurrence in the 5-year follow-up of the patient.
Discussion
Until the 1980s, surgery was the only treatment option for hydatid cysts. Although more conservative approaches came to the forefront in the following years, surgery has been recognized as the most effective treatment. Anti-parasitic drugs and percutaneous treatments can be used in selected patient groups to avoid complications of surgery.
The most commonly used classification in determining the treatment method is the Gharbi classification, which evaluates liver hydatid cysts ultrasonographically [5]. All viable cysts according to this classification, except the small ones should be treated surgically or with PAIR (puncture, aspiration, ınjection, reaspiration). Gharbi type III, compressive type IV and V cysts, cysts associated with the biliary tract, and cysts not suitable for PAIR treatment require surgery.
In surgical treatment, inactivating the cyst contents, opening the cyst, and removing the germinative membrane are commonly performed. In peripheral cysts, total pericystectomy or partial hepatectomy may be performed. Care should be taken not to spread the parasite into the abdomen during surgery.
In the literature, there were six patients whose cysts were found to be larger than 30 cm in the measurements made by imaging methods treated for hydatid cysts in liver (Table 1). Percutaneous treatment was performed in only one of these cases and surgical treatment was preferred in the others. Four of the patients were operated on under elective conditions and one was operated on under emergency conditions.
Battyany et al. [6] inserted an 8F catheter into the cyst and aspirated 6200 mL of cyst fluid, followed by PAIR treatment for 6 weeks with a cycle of 150 mL 15% hypertonic saline injection-drainage-40 mL 15% sterile saline injection, and 30 mL alcohol injection for the last 5 days. To prevent anaphylactic reactions and the spread of the disease, the patient was started on mebendazole (200 mg/day for 3 days) before the procedure. The patient’s cyst disappeared completely on CT scan and was presented as the largest hydatid cyst treated with PAIR. They recommended PAIR as an effective and safe method to avoid complications of surgery in large cysts.
Sahin et al. [7] performed pericystectomy on a 32 × 15 cm giant hydatid cyst located in the right lobe of the liver and the patient was discharged without complications.
Ettorre et al. [8] removed a 30 × 18 × 16 cm hydatid cyst compressing the inferior vena cava by right hepatectomy and the patient was discharged on the 7th postoperative day without complications.
Mohammed et al. [9] operated on a patient with 3 hydatid cysts of 10, 11, and 40 cm in the right lobe of the liver. After aspirating 4 L of cyst fluid, they excised the cyst wall, closed the two bile ducts opening into the cyst cavity with a slow-absorbing monofilament suture, and performed omentoplasty. The patient was discharged 6 days after the operation and had bile leakage from the drain, which stopped 1 month later. The patient received anti-helminthic treatment for 3 months.
Sandonato et al. [10] operated on a patient with two cysts measuring 12 × 14 × 10 cm in the right lobe of the liver and 27 × 30 cm in the right half of the abdomen, drained the cyst contents, and performed partial pericystectomy after washing with 20% hypertonic saline. The patient was discharged on the 8th postoperative day without complications and was treated with albendazole 10 mg/kg/day for 6 weeks. No recurrence was observed in the 2-year follow-up.
Gole et al. [11] performed partial cystectomy on a patient with a 45 × 35 × 20-cm hydatid cyst originating from the left lobe of the liver and presented the largest hydatid cyst in the literature. They reported that the patient had no clinical signs and symptoms in the 2-year follow-up.
Hydatid cysts that reach large sizes in the abdomen may rarely rupture. Hydatid cysts that reach large sizes in the abdomen may originate from organs other than the liver and may rarely rupture. This complication, which may result in mortality, is rare and dangerous. Belli et al. [12] took a patient with a giant hydatid cyst into emergency surgery with signs of rupture and anaphylactic shock. A 30 × 20 cm cyst with the spleen was completely excised but the patient died on the 3rd postoperative day.
Surgical procedures predominate in the treatment of hydatid cysts that reach large sizes. Although the complications of surgery are avoided in the patient treated percutaneously, the disadvantage is the long treatment period of 6 weeks. PAIR treatment is successfully applied in smaller hydatid cysts. Anti-parasitic drugs can be added to adjuvant treatment. Anaphylactic shock due to rupture of hydatid cysts is a serious and mortal complication that is more common in large hydatid cysts. Therefore, treatment should not be delayed in giant hydatid cysts.
Conclusion
Hydatid cysts can very rarely reach giant sizes without symptoms. Patients with giant cysts usually need radical surgical treatment because these type of cysts can lead to biliary tract complications, perforation, and anaphylaxis.
Availability of data and materials
Data sharing not applicable to this article as no datasets were generated or analyzed during the current study.
References
Wen H, Vuitton L, Tuxun T, Li J, Vuitton DA, Zhang W, et al. Echinococcosis: Advances in the 21st Century. Clin Microbiol Rev. 2019;32(2):e00075-18.
Liu W, Delabrousse É, Blagosklonov O, Wang J, Zeng H, Jiang Y et al (2014) Innovation in hepatic alveolar echinococcosis imaging: best use of old tools, and necessary evaluation of new ones. Parasite 21:1–14
Azizi A, Blagosklonov O, Lounis A, Berthet L, Vuitton DA, Bresson-Hadni S et al (2015) Alveolar echinococcosis: correlation between hepatic MRI findings and FDG-PET/CT metabolic activity. Abdom Imaging 40(1):56–63
Brunetti E, Kern P, Vuitton DA (2010) Expert consensus for the diagnosis and treatment of cystic and alveolar echinococcosis in humans. Acta Trop 114(1):1–16
Gharbi HA, Hassine W, Brauner MW, Dupuch K (1981) Ultrasound examination of the hydatic liver. Radiology 139(2):459–463
Battyány I, Herbert Z, Rostás T, Vincze Á, Fülöp A, Harmat Z et al (2006) Successful percutaneous drainage of a giant hydatid cyst in the liver. World J Gastroenterol 12(5):812–814
Sahin DA, Kusaslan R, Sahin O, Dilek ON (2007) Huge hydatid cysts that arise from the liver, growing exophytically. Can J Surg 50(4):301–303
Ettorre GM, Vennarecci G, Santoro R, Laurenzi A, Ceribelli C, di Cintio A et al (2012) Giant hydatid cyst of the liver with a retroperitoneal growth: a case report. J Med Case Rep 6:2–5
Mohammed AA, Arif SH (2019) Surgical excision of a giant pedunculated hydatid cyst of the liver. J Surg Case Rep 2019(7):1–4
Sandonato L, Cipolla C, Li Petri S, Ciacio O, Galia M, Cannizzaro F et al (2006) Giant hepatic hydatid cyst as a cause of small bowel obstruction. Am Surg 72(5):405–408
Gole G, Tati S, Bashetty S, Somani S (2011) Pedunculated giant hepatic hydatid cyst: Largest ever reported. Trop Parasitol 1(2):132
Belli S, Akbulut S, Erbay G, Kocȩr NE (2014) Spontaneous giant splenic hydatid cyst rupture causing fatal anaphylactic shock: a case report and brief literature review. Turkish J Gastroenterol 25(1):88–91
Acknowledgements
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
AD, ES, and YD were operated on. AD prepared the study design. ES collected the data about the patient. YD performed the literature review. AD and YD helped to prepare the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Permission to publish was obtained from the patient.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Şahin, E., Dalda, Y. & Dirican, A. Giant hydatid cyst of the liver: a case report with literature review. Egypt Liver Journal 13, 28 (2023). https://doi.org/10.1186/s43066-023-00264-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43066-023-00264-w