Abstract
Background
Virtual reality (VR) is increasingly used in healthcare settings as recent technological advancements create possibilities for diagnosis and treatment. VR is a technology that uses a headset to simulate a reality in which the user is immersed in a virtual environment, creating the impression that the user is physically present in this virtual space. Despite the potential added value of virtual reality technology in healthcare, its uptake in clinical practice is still in its infancy and challenges arise in the implementation of VR. Effective implementation could improve the adoption, uptake, and impact of VR. However, these implementation procedures still seem to be understudied in practice. This scoping review aimed to examine the current state of affairs in the implementation of VR technology in healthcare settings and to provide an overview of factors related to the implementation of VR.
Methods
To give an overview of relevant literature, a scoping review was undertaken of articles published up until February 2022, guided by the methodological framework of Arksey and O’Malley (2005). The databases Scopus, PsycINFO, and Web of Science were systematically searched to identify records that highlighted the current state of affairs regarding the implementation of VR in healthcare settings. Information about each study was extracted using a structured data extraction form.
Results
Of the 5523 records identified, 29 were included in this study. Most studies focused on barriers and facilitators to implementation, highlighting similar factors related to the behavior of adopters of VR and the practical resources the organization should arrange for. However, few studies focus on systematic implementation and on using a theoretical framework to guide implementation. Despite the recommendation of using a structured, multi-level implementation intervention to support the needs of all involved stakeholders, there was no link between the identified barriers and facilitators, and specific implementation objectives or suitable strategies to overcome these barriers in the included articles.
Conclusion
To take the implementation of VR in healthcare to the next level, it is important to ensure that implementation is not studied in separate studies focusing on one element, e.g., healthcare provider-related barriers, as is common in current literature. Based on the results of this study, we recommend that the implementation of VR entails the entire process, from identifying barriers to developing and employing a coherent, multi-level implementation intervention with suitable strategies. This implementation process could be supported by implementation frameworks and ideally focus on behavior change of stakeholders such as healthcare providers, patients, and managers. This in turn might result in increased uptake and use of VR technologies that are of added value for healthcare practice.
Similar content being viewed by others
Background
Virtual reality (VR) is increasingly used in healthcare settings as recent technological advancements create possibilities for diagnosis and treatment. VR is a technology that uses a headset to simulate a reality in which the user is immersed in a virtual environment, creating the impression that the user is physically present in this virtual space [1, 2]. VR offers a broad range of possibilities in which the user can interact with a virtual environment or with virtual characters. Virtual characters, also known as avatars, can provide the user with a greater sense of reality and facilitate meaningful interaction [1]. VR interventions have been piloted in various healthcare settings, for example in treating chronic pain [3], improving balance in patients post-stroke [4], managing symptoms of depression [5], improving symptom burden in terminal cancer patients [6], and applied within treatment for forensic psychiatric patients [7]. These studies highlight the opportunities for VR as an innovative technology that could be of added value for healthcare. While there is a need for more research on the efficacy of VR in healthcare, experimental studies have shown that VR use is effective in improving the treatment of, among others, anxiety disorders [8], psychosis [9], or eating disorders [10]. However, the added value of VR is often not observed in practice due to the lack of usage of this technology.
Regarding uptake in clinical practice, VR is still in its infancy [11, 12]. Various barriers are identified as limiting the uptake, such as a lack of time and expertise on how to use VR in treatment, a lack of personalization of some VR applications to patient needs and treatment goals, or the gap in knowledge on the added value of VR in a specific setting [11, 13].
Not only VR uptake is challenging, but also other eHealth technologies experience similar difficulties in implementation [14]. eHealth is known as “the use of technology to improve health, well-being, and healthcare” [14]. For years, implementation has been out of scope for many eHealth research initiatives and healthcare practices, resulting in technologies that have not surpassed the level of development [15]. For these technologies to succeed and be used as effectively as intended, they must be well integrated into current healthcare practices and connected to the needs of patients and healthcare practitioners [13]. As a result, a focus on the implementation is of added value. It has the potential to improve the adoption, uptake, and impact of technology [16]. However, implementation procedures for VR technology still seem to be understudied in both research and practice [12, 17].
One of the reasons for the lacking uptake of (eHealth) technology is the complexity of the implementation process [18, 19]. The phase between the organizational decision to adopt an eHealth technology and the healthcare providers actually using the technology in their routine is complex and multifaceted [18, 19]. This highlights the importance of a systematic and structured implementation approach that fits identified barriers. The use of implementation strategies, known as the “concrete activities taken to make patients and healthcare providers start and maintain use of new evidence within the clinical setting,” can help this process by tackling the implementation barriers [20]. These strategies can be used as standalone, multifaceted, or as a combination [21]. Often, they are part of an implementation intervention, which describes what will be implemented, to whom, how, and when, with the strategies as a how-to description in the intervention [17]. In addition, according to Proctor et al. [22], it is important to conceptualize and evaluate implementation outcomes. Implementation outcomes, such as acceptability, adoption, appropriateness, feasibility, fidelity, implementation cost, penetration, and sustainability, can be used to set specific and measurable implementation objectives. Furthermore, assessing implementation outcomes will increase the understanding of the success of the implementation process and form a starting point for studies focusing on the effectiveness of VR in healthcare [22].
While implementation interventions could help the systematic implementation of VR, they are rarely used in practice. A way to stimulate systematic implementation and help develop an implementation intervention is by using an implementation model to guide this process. While a broad range of implementation models have been developed, there is still limited use of these models to structure the implementation of VR in healthcare [23]. One framework that could be used to identify important aspects of implementation is the NASSS framework, which investigates the non-adoption, abandonment, and challenges to scale up, spread, and sustainability of technology-supported change efforts in health and social healthcare [24]. The NASSS framework does not only focus on the technology itself, but includes the condition of the target group, the value proposition, the adopter system (staff, patients, and healthcare providers), the healthcare organization(s), the wider system, and the embedding and adoption of technology over time [24]. The framework is used to understand the complexity of the adoption of new technologies within organizations [25]. However, it remains unclear if and what factors of the NASSS framework, or any other implementation framework, can be found in the implementation of VR in various healthcare settings.
In summary, virtual reality interventions have the potential to improve the quality of care, but only if implemented thoroughly. As VR use becomes more prevalent, studies should expand the focus to identify factors specifically related to the implementation of this new technology [19]. It is advised to perform a needs assessment, understand potential barriers to implementation early, set implementation objectives, and identify fitting implementation strategies before testing VR interventions in practice [26]. Therefore, this scoping review aims to examine the current state of affairs in the implementation of VR technology in healthcare settings and provide an overview of factors related to the implementation of VR. Within this research, the following sub-questions are formulated: (1) Which barriers play a role in the implementation of VR in healthcare? (2) Which facilitators play a role in the implementation of VR in healthcare? (3) What implementation strategies are used to implement VR in healthcare? (4) To what extent are specific implementation objectives and outcomes being formulated and achieved? (5) What are the recommendations for the implementation of VR in healthcare?
Methods
To address the study aims, a scoping review was undertaken on the current state of affairs regarding the implementation of virtual reality in healthcare settings. Due to the broad scope of the research questions, a scoping review is most suitable to examine the breadth, depth, or comprehensiveness of evidence in a given field [23]. As a result, scoping reviews represent an appropriate methodology for reviewing literature in a field of interest that has not previously been comprehensively reviewed [24]. This scoping review is based on the methodological framework of Arksey and O’Malley [27] including the following steps: (1) identifying the research questions, (2) identifying relevant studies, (3) study selection, (4) charting the data, and (5) collating, summarizing and reporting the results. A protocol was developed and specified the research questions, study design, data collection procedures, and analysis plan. To the authors’ knowledge, no similar review had been published or was in development. This was confirmed by searching academic databases and the online platforms of organizations that register review protocols. The protocol was registered at OSF (Open Science Framework) under registration https://doi.org/10.17605/OSF.IO/5Z3MN. OSF is an online platform that enables researchers to plan, collect, analyze, and share their work to promote the integrity of research. This scoping review adheres to the Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) [26].
Searches
A comprehensive, systematic electronic literature search was undertaken using three databases: Scopus, PsycINFO, and Web of Science. In each database, the same search strategy was used. Search terms were identified and included in the search strategy for three main categories relevant to the research questions: implementation, virtual reality, and healthcare. The search terms within a category were combined using the Boolean term “OR” and the term “AND”was used between the different categories. The search strategy was piloted to check if keywords and databases were adequate and adjustments were made whenever necessary. The full electronic search strategy can be found in Appendix 1.
Study inclusion and exclusion criteria
All identified records published up until February 2022, that were peer-reviewed, and written in English, Dutch, or German, were included in the initial results. All references and citation details from different electronic databases were imported into the online review management system Covidence and duplicate records were removed automatically. A three-step screening approach, consisting of a title, abstract, and full-text screening, was used to select eligible studies.
Records were included if the titles indicated that the article focused on VR within a healthcare setting and that VR was used as a tool for prevention or treatment of patients. Because of the possibility of implementation not being mentioned in the title, broad criteria were used to prevent the unjust exclusion of relevant studies. In addition, records were included if they outline (parts of) the implementation process of VR technology (e.g., needs assessment, planning, execution, or lessons learned). Furthermore, the primary target group of the VR technology had to be patients with mental or physical disorders. If the studies focused solely on augmented reality (AR) or mixed reality (MR) and/or described a VR technology that was utilized to train healthcare professionals, they were excluded. Additionally, studies were excluded if full texts could not be obtained or if the study design resulted in no primary data collection, such as meta-analyses, viewpoint papers, or book chapters.
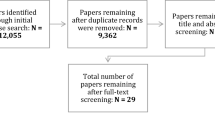
In the first step, two authors (MK & HK) screened all titles for assessment against the inclusion and exclusion criteria for the scoping review. Titles were included based on consensus between both authors. In the event of doubt or disagreement, the title was discussed by both authors. After screening the titles, both authors screened and assessed the abstracts using the inclusion and exclusion criteria. Abstracts were included or excluded based on consensus. In the final step, one author screened the full-text articles (MK). Reasons for excluding and any reservations about including were discussed with the other authors. The results of the search are reported in full and presented in a Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) flow diagram [28] (Fig. 1).
Data extraction strategy
The data extraction of this scoping review is mostly based on the guidelines of the Cochrane Handbook for Systematic Reviews of Interventions [29]. A systematic assessment of study quality was not performed because this review focused on giving a broad overview of all factors related to the implementation of VR. This resulted in a heterogeneous sample of included study topics and designs: ranging from explorative qualitative studies to reflective quantitative studies. The data extraction process started with the creation of a detailed data extraction form based on the research questions in Microsoft Excel. This form was generated to capture the most relevant information from all obtained studies and standardize the reporting of relevant information. The extracted data included the fields as presented in Table 1. One author (MK) filled out the data extraction forms; in case of uncertainties, a second author was consulted (HK). Secondly, for each category, relevant text fragments from each study were copied from the articles into the data extraction forms.
Data synthesis and presentation
To answer the first and second research questions, the fragments from the data extraction forms were coded inductively. To answer the third and fourth research questions, fragments were first coded deductively, based on the main categories of the NASSS framework: technology, adopters, organization(s), wider system or embedding, and adaptation over time [24]. Second, within these categories, the specific barriers and facilitators were coded inductively to identify recurrent themes. The implementation recommendations were coded inductively to answer the fifth and last research question. The first author executed the coding process, which included multiple iterations and constant adaptations until data saturation was reached. During this iterative process, multiple versions of the coding scheme were discussed with all authors and adapted accordingly.
Results
Search results
The search strategy, the number of included records, and the reasons for full-text exclusion are provided in Fig. 1. The main reason for excluding full-text articles was that studies focused on the usability or effectiveness of VR, rather than on the needs assessment, planning, execution, or lessons learned from the implementation process of VR.
Study and technology characteristics
An overview of the characteristics of the 29 included records and the used VR technology is provided in Appendix 2. The following study designs were identified: qualitative (n = 13), quantitative cross-sectional (n = 10), and studies that used qualitative as well as quantitative methods (n = 6).
Of the 29 included records, 11 focused on VR use in rehabilitation clinics. Additional settings in which VR was applied are general health clinics, mental health clinics, or clinics for specific disorders, e.g., eating disorder clinics or burn clinics. The goal of VR technology was often to be of added value as a treatment tool. It was used to improve movement in rehabilitation patients (n = 11) or decrease anxiety in patients with a stress-related disorder (n = 2). In addition, it was applied to offer distraction or relaxation during medical procedures (n = 4). In addition to the variety in settings and applications of VR, the type of technology that was applied differed as well: from interactive VR (n = 26), in which patients can be immersed in a virtual environment, such as a shopping street or a restaurant, via a VR headset and interact with this environment, to (360°) videos (n = 4) in which patients are immersed in a virtual environment shown on a (computer) screen, with limited to no possibility for interaction.
Implementation characteristics
An overview of the 29 included studies and the implementation characteristics, such as the use of an implementation model or the stage of implementation research are presented in Appendix 2. In this review, 8 of the 29 studies used a theoretical framework to structure implementation or data analysis. The Consolidated Framework for Implementation Research (CFIR) [30] was used in 3 studies and the Decomposed Theory of Planned Behavior (DTPB) [31] was also used in 3 studies. In addition, the Unified Theory of Acceptance and Use of Technology (UTAUT2) [32] was used in a single study, and the Innovation Diffusion Theory [33] was applied in one study as well.
Of the 29 included studies, the data collection of 12 studies took place before actual implementation and focused on factors, expected by stakeholders, that could influence future implementation. The data collection of the other 17 studies took place after actual implementation and reflected on existing factors related to implementation. Thus, most identified barriers, facilitators, and recommendations stated in this review were observed in studies that evaluated an existing implementation process.
Barriers to implementation
Barriers to the implementation of VR were identified based on relevant fragments from the articles. In 26 records, a total of 69 different barriers were identified and divided into categories of the NASSS framework. All barriers are provided in Table 2. The barriers are explained in the accompanying text below.
A broad range of barriers was relevant to the implementation of VR in healthcare. Most identified barriers were related to the organization category of the NASSS framework. These were mainly focused on the lack of practical resources for healthcare providers to use VR. For example, the organization does not schedule sufficient time for healthcare providers to learn how to use VR and how to integrate VR into practice. In addition to a lack of time, not enough technical support, treatment rooms for VR, and VR equipment to treat patients were mentioned as organizational barriers.
Frequently mentioned barriers related to the adopters were factors that negatively influence healthcare providers’ opinions of VR. First, a lack of research and evidence on the added value of VR was mentioned as a barrier. Second, a perceived lack of experience in working with VR was said to cause a lack of confidence and self-efficacy in healthcare providers to work with VR during treatment. The perceived lack of time and limited opportunities to learn how to use VR contributed to this feeling.
Furthermore, technical barriers were identified to hinder VR implementation. Functional issues, such as technical malfunctioning of VR hardware or software, or a lack of client safety while wearing a VR headset in the limited space of the treatment room that limits freedom of movement were most frequently mentioned as barriers. Related to the VR headset, a lack of physical comfort for the patient when wearing the VR headset and the feeling of isolation while wearing the headset were frequently mentioned as barriers.
Lastly, barriers related to the condition, value proposition, wider system, and embedding and adoption over time categories of the NASSS framework were less frequently identified. The conditions and physical limitations of patients that could negatively influence VR use, such as several cognitive limitations, distress, or cybersickness during VR, were mentioned as barriers. Related to the value proposition, barriers such as high costs to purchase VR equipment or the lack of time for maintaining the VR hardware were mentioned. In addition, the lack of personalization to patients’ needs and treatment goals was mentioned as a barrier. The barriers related to the wider system and adoption over time, such as organizations not being innovation-minded or the lack of insurance reimbursement to compensate for costs of VR use, were mentioned less frequently.
Facilitators to implementation
Besides barriers, a total of 53 different facilitators to the implementation of VR in healthcare were identified in 26 records. Facilitators were identified based on relevant fragments from the articles and are divided into categories of the NASSS framework. They are mentioned and explained in Table 3 and the accompanying text below.
In comparison to the barriers, facilitators to implementation were identified less frequently in the included studies. Similar to the barriers, most facilitators were related to the organization category of the NASSS framework. As an organization, providing support, time, room, and technical system support to healthcare providers to learn and use VR were mentioned most frequently as facilitators.
In multiple studies, it was mentioned that adopters of VR technology need training and education on how to use and integrate VR into treatment. Healthcare providers want to increase their knowledge, skills, and experience with VR to feel confident and increase self-efficacy in using VR in treatment with patients. Besides, as a facilitator in the adopter’s category, it is mentioned that having access to evidence on the added value of VR for treatment is a major facilitator in VR implementation because healthcare providers feel the use of VR is validated within the treatment.
Lastly, facilitators in the condition, technology, value proposition, wider system, and embedding and adoption over time category of the NASSS framework were identified less frequently. For example, when looking at the sociodemographic factors of patients, the young age of patients was identified as a facilitator since these people tend to be more open to new technology and treatments and feel more comfortable using VR. Related to technology, ensuring client safety was mentioned as a facilitator, that is creating a physically safe space in the treatment room for patients to use VR. This safe and controlled environment was also identified in the value proposition category. Meaning that healthcare providers can create a safe space for patients to practice challenging behavior. Lastly, being innovation-minded as an organization and VR becoming more and more commonplace and affordable to scale up were both mentioned as facilitators in the wider system category and the adoption over time category of the NASSS framework.
Implementation strategies, objectives, and outcomes
An overview was created of the implementation strategies, objectives, and outcomes that were extracted from the included studies (see Appendix 2). In two studies, a clear implementation objective was mentioned [13, 43]. These objectives both focused on designing an implementation intervention, the knowledge translation (KT) intervention, to translate knowledge about the use of VR to the healthcare provider. In addition, they aimed to identify factors that influenced VR adoption and healthcare providers’ support needs.
Of the 29 included records, 8 studies described actual implementation strategies [13, 34, 35, 43, 44, 48, 53, 60]. Most were mentioned in studies that collected data after implementation and reflect on existing implementation processes. In the included studies that described expected implementation factors, implementation strategies were most often not described. These studies focused on identifying potential barriers and/or facilitators in preparation for the implementation phase and did not evaluate the used strategies.
A summary of the described implementation strategies mentioned in the included records is displayed below in Table 4. Examples of strategies focused on practical resources were VR equipment to be used in treatment, treatment rooms in which the VR technology can be set up and used, and time for healthcare providers to learn about VR use. In addition, training and education on VR use were mentioned as important strategies. Hands-on interactive training, e-learning modules, mentorship for support and troubleshooting, and matching protocols and guidelines on how to use VR were mentioned. To set up VR treatment, an identified implementation strategy is to give support to healthcare providers in selecting appropriate content in VR that fits the patient’s needs and give information on how to instruct the patient about VR treatment. Lastly, implementation strategies that help to increase the motivation of healthcare providers to use VR were addressed. For example, having sufficient time to discuss the potential and added value of VR or having support from champions or mentors, experienced healthcare providers who share their experience with VR, to motivate others to integrate VR into their treatment practice were used during implementation.
The explicit conceptualization of implementation outcomes and the use of these outcomes to formulate implementation objectives or design implementation strategies was not described as such in the included records. The concepts of acceptability, adoption, uptake, or feasibility were mentioned in 12 records (see Appendix 2); however, they were not integrated as outcomes into a systematic implementation process.
Recommendations for implementation
In Table 5, an overview of the 51 different recommendations for the implementation of VR in healthcare that were mentioned in 20 records is provided. These recommendations were inductively coded and divided into seven categories: (1) Increase understanding of patient suitability, (2) Improve knowledge and skills on VR use, (3) Improve healthcare providers’ engagement with VR, (4) Have support staff available, (5) Points of attention for developing VR treatment, (6) Support functionality of VR hardware and software, and (7) Design and development of implementation.
The first recommendation was to increase the understanding of patient suitability. In other words, it should be clear for healthcare providers how they can determine for which patients VR treatment is a fitting option. One way to determine patient suitability is to take into account the functional limitations of patients, such as their level of mobility or communication skills, before referring patients to VR treatment. Next to functional limitations, one should take into account cognitive limitations and any sensitivity to cybersickness. Patient suitability can be dependent on the goal of VR treatment, as some functional or cognitive limitations are not always a barrier to VR use.
The second recommendation was to improve the knowledge and skills of healthcare providers on VR use. Training programs and other educational resources, such as training days, online meetings, or instruction videos, that should be developed and disseminated to healthcare providers were mentioned as key elements to improving knowledge and skills.
The third recommendation was to improve healthcare providers’ engagement with VR. To accomplish this, the benefits of VR use and its possible contributions to treatment should be communicated to healthcare providers and patients. The use of successful example cases and disseminating supportive evidence of the added value of VR were mentioned as options to increase the engagement of healthcare providers with VR.
The fourth recommendation was to have sufficient support staff available to support VR use during treatment and maintain VR equipment. In addition, champions or mentors, healthcare providers experienced in VR treatment, were mentioned to promote uptake and increase the self-efficacy of other healthcare providers in VR use.
The fifth recommendation was related to developing VR treatment. The included studies gave some inconsistent suggestions on the frequency of use, from daily to once a week. Important aspects of developing a VR treatment are to set clear treatment goals, let the patient become familiar and comfortable with the VR equipment and software, and increase the treatment difficulty step by step.
The sixth recommendation was to support the functionality of VR hardware and software and ensure that it fits the user. Software should be appropriate for the patient’s needs, and age, and should fit the treatment setting. For example, VR software for forensic mental healthcare patients with aggression regulation problems should be able to let patients practice self-regulation strategies in virtual environments in which their undesired behavior is triggered. This could be a bar or supermarket with strangers for one patient, or a more intimate setting with a partner at home for another. The hardware needs to be adaptable for the limited mobility of patients, for example, patients that are wheelchair-bound. In addition, the VR hardware should still give the possibility for healthcare providers and patients to interact during the use of VR. The patient needs to be able to hear the voice of the healthcare provider.
The seventh and last recommendation was related to the design and development of the implementation of VR in practice. In multiple studies, it was advised that healthcare organizations use a structured, multi-model implementation intervention to support the needs of stakeholders and address barriers to VR use. The key stakeholders should be engaged during the development process of implementation interventions. It was recommended to use a theoretical framework, such as the Consolidated Framework for Implementation Research (CFIR) [46] or the Decomposed Theory of Planned Behavior (DTPB) [47] to guide the development of relevant implementation strategies to enhance the uptake of VR in healthcare practice.
Discussion
Principal findings
This scoping review was conducted to provide insight into the current state of affairs regarding the implementation process of virtual reality in healthcare and to identify recommendations to improve implementation research and practice in this area. This review has resulted in an overview of current implementation practices. A broad range of study designs was identified: from qualitative studies that described expected factors of implementation, to quantitative methods that summarized observed factors. From the included studies, it can be concluded that the main focus of the implementation of VR is on practical barriers and facilitators, and less attention is paid to creating a systematic implementation plan, including concrete implementation objectives, developing suitable implementation strategies to overcome these barriers, and linking these barriers or facilitators to clear implementation outcomes. Only two studies described objectives for implementation and the practical strategies that were used to reach these objectives. Most implementation strategies that were described were related to practical resources and organizational support to create time and room for healthcare providers to learn about VR and use it in treatment. Despite differences in the type of VR technology, healthcare settings, and study designs, many studies identified the same type of barriers and facilitators. Most identified barriers and facilitators focused on the adopter system and organization categories of the NASSS framework [24], e.g., the needs of healthcare providers related to VR use and the organizational support during the implementation of VR. The most frequently mentioned barriers were a lack of practical resources, a lack of validated evidence on the added value of VR, and a perceived lack of experience in working with VR. This review showed that facilitators were studied less than barriers. Most of the included studies only described the implementation barriers. However, in the studies that did mention facilitators, similar themes were found between identified barriers and facilitators, mostly related to practical resources, organizational support, and providing evidence of the added value of VR were found. The content of the recommendations for the implementation of VR fits with the foregoing.
Comparison with prior work
Despite the importance of concrete strategies to successfully implement VR [20] and the conceptualization of implementation outcomes to understand the process and impact of implementation [22], there is a lack of research on this systematic implementation approach. In this review, only a few studies used a theoretical framework to structure implementation or data analysis. Frameworks that were mentioned most often were the Consolidated Framework for Implementation Research (CFIR) [30], and the Decomposed Theory of Planned Behavior (DTPB) [31]. However, none of the studies that mentioned the use of these models described an explicit link between the separate strategies, barriers, or facilitators and the integrated systematic implementation process. This illustrates the gap in research between identifying factors that influence implementation and linking them to practical strategies and implementation outcomes to form a coherent implementation intervention. The development of a coherent implementation intervention was only mentioned in two studies that were included in this review. To illustrate, one study set up an implementation intervention that promotes clinician behavior change to support implementation and improves patient care [63]. A coherent intervention could be an option to structure the implementation process and bridge the gap between knowledge of the use of VR to actual uptake in practice [63]. However, from implementation frameworks, such as the NASSS framework [24] or the CFIR [30], it is clear that the focus should lie on a coherent multilevel implementation intervention that focuses on all involved stakeholders and end-users, not only on one stakeholder.
The importance of focusing on the behavior change of all involved stakeholders, such as healthcare providers, patients, support staff, and managers, is reflected in the results of this review. Most barriers, facilitators, strategies, and recommendations are related to stakeholders within the healthcare organization that need to change their behavior in order to support implementation. For example, healthcare providers are expected to learn new skills to use VR and organizational management needs to make time and room available to support healthcare providers in their new learning needs and actual VR use during treatment. This highlights the importance of focusing on strategies that target concrete behavior of stakeholders for successful implementation. Identifying concrete behavior that is targeted in an implementation intervention can help describe who needs to do what differently, identify modifiable barriers and facilitators, develop specific strategies, and ultimately provide an indicator of what to measure to evaluate an intervention’s effect on behavior change [64]. The focus on behavior in implementation is not new, it is an important point of attention in the implementation of other eHealth technology [14]. However, based on the results of this scoping review, this focus is lacking in research on VR implementation.
To design implementation interventions that focus on the behavior change of stakeholders, existing intervention development frameworks can be used. An example is Intervention Mapping (IM). Intervention Mapping is a protocol that guides the design of multi-level health promotion interventions and implementation strategies [65, 66]. It uses a participatory development process to create an implementation intervention that fits with the implementation needs of all involved stakeholders [65]. Eldredge et al. [65] and Donaldson et al. [67] IM can provide guidance on overcoming barriers by applying implementation strategies based on behavioral determinants and suitable behavior change techniques [65]. For example, when reflecting on the implementation strategies described in this review, providing feedback as a behavior change method can be used during the education or training on VR use to support the learning needs of healthcare providers. In addition, providing opportunities for social support could be seen as the behavior change technique behind the need for support and discussion of VR use during intervision groups with other healthcare providers.
Implications for practice and future research
The results from this review provide various points of departure for future implementation research and implications for practice. An important implication for both is the need for a systematic approach to the implementation process. Most studies identified in this review focused only on barriers or facilitators to implementation, not paying attention to the systematic process of developing an implementation intervention that specifies implementation objectives, describes suitable strategies that fit with these barriers and facilitators, and conceptualizes implementation outcomes to evaluate the effectiveness of these strategies. The development of an implementation intervention should preferably be supported by theoretical implementation frameworks such as the Consolidated Framework of Implementation Research [30], or the NASSS framework [24]. In this review, all implementation factors could be coded with and analyzed within the categories of the NASSS framework. Indicating its usefulness in structuring implementation research. Future research could focus on applying and evaluating such implementation frameworks to the implementation of VR in healthcare, specifying factors related to the implementation of VR and focusing on all phases and levels of implementation.
In addition, it could be valuable to focus on existing intervention development frameworks, such as Intervention Mapping, to guide the design of a complete implementation intervention. Future research could apply these existing frameworks in an implementation context, reflect on the similarity in working mechanisms and evaluate their influence on the implementation process and the behavior change of the involved stakeholders. This way, a first step in identifying the added value of systematic implementation intervention development can be made.
Furthermore, as being aware and convinced of the added value of VR within the treatment of patients is seen as an important facilitator of implementation for healthcare providers and organizations, it would be valuable for future research to focus on the evaluation of the efficacy of VR within healthcare practice. However, this raises an interesting paradox. Healthcare organizations and healthcare providers would like to have evidence of the added value of VR before investing in the technology for its implementation, but the efficacy of VR in practice can only be determined in an ecologically valid way when it is already thoroughly implemented in healthcare practice.
Strengths and limitations
This review set out to give an overview of factors that are related to the implementation practice of VR in healthcare. A strength of this study is that it used the NASSS framework to structure the analysis and review process. The use of an implementation framework contributed to systematic data collection and analysis, which can increase the credibility of the findings [68]. However, the use of the NASSS framework also revealed some drawbacks. Although all implementation factors were categorized within the categories of the NASSS framework, this coding was limited by the description of these categories and the overlap between some categories. For example, most barriers and facilitators that were categorized under organization, adopters, or technology were relevant for sustainable embedding and thus could fit in the category “embedding and adaptation over time” as well. In addition, the description of the category “condition,” the illness of the patient, and possible comorbidities, which are often influenced by biomedical and epidemiological factors [24], is too limited to describe all factors related to patient suitability for VR. The condition of a patient within mental healthcare is often related to other aspects, such as sociodemographic factors like age, technical skills, and feeling comfortable using new technology. All these factors could influence patient suitability for VR. Besides, in most included studies, the barriers or facilitators were not described in great detail, which made the coding process within the NASSS categories more difficult.
Furthermore, when titles of screened records did not focus on the implementation process of VR, e.g., studies that only focused on usability or effectiveness, they were excluded. Since usability studies could still partly focus on implementation, this may have caused us to miss publications that could provide interesting insights on implementation but whose main focus was other than that. We tried to overcome this limitation by selecting detailed inclusion and exclusion criteria for the literature search and abstract screening. The study was excluded only when there was no indication of a link between usability and implementation.
In addition, the full-text screening and data-extraction process were executed by one researcher. This could have caused us to miss information related to the topic. However, since the researcher used inclusion criteria that were thoroughly discussed during the title and abstract screening, and used a detailed data-extraction form, the chances of missing information are considered to be low. Furthermore, the first and second authors both extracted data from a few full-text articles, and in case of doubt, full-text were discussed with both authors.
Furthermore, because this scoping review aimed to provide an overview of the current state of affairs related to the implementation of VR in healthcare, all available studies were included, regardless of their quality and type of results. This is in line with the general aim of scoping reviews, which is to present a broad overview of the evidence on a topic. Since a quality assessment was not conducted, not all results of included studies might be valid or reliable. In addition, most of the barriers, facilitators, and recommendations stated in this review are observed in studies that took place after actual implementation. However, some of these factors were mentioned as potential factors related to implementation in studies that collected data before actual implementation. These factors were described as expected factors by involved stakeholders, but not observed. Therefore, these findings should be interpreted with care.
Conclusion
This scoping review has resulted in an initial overview of the current state of affairs regarding the implementation of VR in healthcare. It can be concluded that in the included publications, a clear focus on practical barriers and facilitators to the implementation of VR has been identified. In only a few studies implementation frameworks, specified strategies, objectives, or outcomes were addressed. To take the implementation of VR in healthcare to the next level, it is important to ensure that implementation is not studied in separate studies focusing on one element, e.g., therapist-related barriers, but that it entails the entire process, from identifying barriers to developing and employing a coherent, multi-level implementation intervention with suitable strategies, clear implementation objectives and predefined outcomes. This implementation process should be supported by implementation frameworks and ideally focus on behavior change of stakeholders such as healthcare providers, patients, and managers. This in turn might result in increased uptake and use of VR technologies that are of added value for healthcare practice.
Availability of data and materials
All dataset(s) supporting the conclusions of this article are available in the included primary studies.
References
Kim M, Jeon C, Kim J. A study on immersion and presence of a portable hand haptic system for immersive virtual reality, Sensors. 2017;17(5). https://doi.org/10.3390/S17051141.
Pillai AS, Mathew PS. Impact of virtual reality in healthcare. In: Virtual and Augmented Reality in Mental Health Treatment, vol. 17. 2018.
Li A, Montaño Z, Chen VJ, Gold JI. Virtual reality and pain management: current trends and future directions. Pain Manag. 2011;1(2):147–57. https://doi.org/10.2217/pmt.10.15.
de Rooij IJM, van de Port IGL, Meijer J-WG. Effect of virtual reality training on balance and gait ability in patients with stroke: systematic review and meta-analysis. Phys Ther. 2016;96(12):1905–18. https://doi.org/10.2522/ptj.20160054.
Falconer CJ, et al. Embodying self-compassion within virtual reality and its effects on patients with depression. BJPsych Open. 2016;2(1):74–80. https://doi.org/10.1192/bjpo.bp.115.002147.
Niki K, et al. A novel palliative care approach using virtual reality for improving various symptoms of terminal cancer patients: a preliminary prospective, multicenter study. J Palliat Med. 2019;22(6):702–7. https://doi.org/10.1089/jpm.2018.0527.
Kip H, Bouman YHA. Van denken en praten naar doen en ervaren: op zoek naar de toegevoegde waarde van technologie voor de forensische psychiatrie. 2020.
Valmaggia LR, Latif L, Kempton MJ, Rus-Calafell M. Virtual reality in the psychological treatment for mental health problems: an systematic review of recent evidence. Psychiatry Res. 2016;236:189–95. https://doi.org/10.1016/j.psychres.2016.01.015.
Pot-Kolder RMCA, et al. Virtual-reality-based cognitive behavioural therapy versus waiting list control for paranoid ideation and social avoidance in patients with psychotic disorders: a single-blind randomised controlled trial. Lancet Psychiatry. 2018;5(3):217–26. https://doi.org/10.1016/S2215-0366(18)30053-1.
Clus D, Larsen ME, Lemey C, Berrouiguet S. The use of virtual reality in patients with eating disorders: systematic review, J Med Internet Res 2018;20(4). https://doi.org/10.2196/jmir.7898. JMIR Publications Inc.
Smith V et al. The effectiveness of virtual reality in managing acute pain and anxiety for medical inpatients: systematic review. J Med Internet Res 2020;22(11). https://doi.org/10.2196/17980. JMIR Publications Inc.
B Garrett, T Taverner, D Gromala, G Tao, E Cordingley, C Sun. Virtual reality clinical research: promises and challenges, JMIR Serious Games 2018;6(4). https://doi.org/10.2196/10839. JMIR Publications Inc.
Levac DE, Miller PA. Integrating virtual reality video games into practice: clinicians’ experiences. Physiother Theory Pract. 2013;29(7):504–12. https://doi.org/10.3109/09593985.2012.762078.
van Gemert-Pijnen L, Kelders S, Kip H, Sanderman R. eHealth research, theory and development. Oxford, New York: Routledge; 2018.
Pieterse M, Kip H, Cruz-Martínez RR. The complexity of eHealth Implementation: a theoretical and practical perspective. 2018.
J. E. W. C. Van Gemert-Pijnen et al. A holistic framework to improve the uptake and impact of ehealth technologies. J Med Internet Res 2011;13(4). https://doi.org/10.2196/jmir.1672. JMIR Publications Inc.
Brassel S, Power E, Campbell A, Brunner M, Togher L. Recommendations for the design and implementation of virtual reality for acquired brain injury rehabilitation: systematic review. J Med Internet Res. 2021;23(7):e26344.
Varsi C, Ekstedt M, Gammon D, Ruland CM. Using the consolidated framework for implementation research to identify barriers and facilitators for the implementation of an internet-based patient-provider communication service in five settings: a qualitative study. J Med Internet Res. 2015;17(11). https://doi.org/10.2196/jmir.5091.
Ross J, Stevenson F, Lau R, Murray E. Factors that influence the implementation of e-health: a systematic review of systematic reviews (an update). Implement Sci;11(1). 2016. https://doi.org/10.1186/s13012-016-0510-7. BioMed Central Ltd.
Waltz TJ et al. Use of concept mapping to characterize relationships among implementation strategies and assess their feasibility and importance: results from the Expert Recommendations for Implementing Change (ERIC) study. Implement Sci 2015;10(1). https://doi.org/10.1186/s13012-015-0295-0.
Powell BJ et al. Enhancing the impact of implementation strategies in healthcare: a research agenda. Front Public Health 2019;7. https://doi.org/10.3389/fpubh.2019.00003.
Proctor E, et al. Outcomes for implementation research: Conceptual distinctions, measurement challenges, and research agenda. Adm Policy Ment Health Ment Health Serv Res. 2011;38(2):65–76. https://doi.org/10.1007/s10488-010-0319-7.
Ritchie MJ, et al. Using implementation facilitation to improve care in Veterans Health Administration (version 2), Veterans Health Administration, Quality Enhancement Research Initiative (QUERI) for Team-Based Behavioral Health. 2017.
Greenhalgh T, Abimbola S. The NASSS Framework A Synthesis of Multiple Theories of Technology Implementation. Stud Health Technol Inform. 2019;263:193–204. https://doi.org/10.3233/SHTI190123.
Thach KS, Lederman R, Waycott J. "Virtual Reality in Residential Aged Care: a study of adoption and system complexity." (2020). ACIS 2020 Proceedings. 56.
Birckhead B et al. Recommendations for methodology of virtual reality clinical trials in health care by an international working group: iterative study. JMIR Ment Health 2019;6(1). https://doi.org/10.2196/11973. JMIR Publications Inc.
Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Method. 2005;8(1):19–32. https://doi.org/10.1080/1364557032000119616.
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol. 2009;62(10):1006–12. https://doi.org/10.1016/j.jclinepi.2009.06.005.
O'Connor D, Green S, Higgins JP. Defining the review question and developing criteria for including studies. Cochrane handbook for systematic reviews of interventions: Cochrane book series. 2008. p. 81–94.
Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci 2009;4(1). https://doi.org/10.1186/1748-5908-4-50.
Taylor S, Todd P. Marketing Decomposition and crossover effects in the theory of planned behavior: a study of consumer adoption intentions. 1995.
Venkatesh V, Thong JYL, Xu X. Consumer acceptance and use of information technology: extending the unified theory of acceptance and use of technology. 2012.
Rogers E. Diffusion of innovations. 1995.
Chung OS et al. Implementation of therapeutic virtual reality into psychiatric care: clinicians’ and service managers’ perspectives. Front Psychiatry 2022;12. https://doi.org/10.3389/fpsyt.2021.791123.
Demers M, et al. Exergaming for stroke rehabilitation: lessons learned for future implementation strategies. 2019.
Cavenett W et al. Deploying new technology in residential aged care: staff members’ perspectives, in ACM International Conference Proceeding Series, Association for Computing Machinery. 2018, pp. 200–204. https://doi.org/10.1145/3292147.3292214.
Nguyen AV, et al. Virtual reality exergaming as adjunctive therapy in a sub-acute stroke rehabilitation setting: facilitators and barriers. Disabil Rehabil Assist Technol. 2019;14(4):317–24. https://doi.org/10.1080/17483107.2018.1447608.
Ogourtsova T, Archambault PS, Lamontagne A. Exploring barriers and facilitators to the clinical use of virtual reality for post-stroke unilateral spatial neglect assessment. Disabil Rehabil. 2019;41(3):284–92. https://doi.org/10.1080/09638288.2017.1387292.
Stamou G, Garcia-Palacios A, Botella C. The combination of cognitive-behavioural therapy with virtual reality for the treatment of post-natal depression, in ACM International Conference Proceeding Series, Association for Computing Machinery. 2019, pp. 599–603. https://doi.org/10.1145/3369457.3369541.
Rimer E, Husby LV, Solem S. Virtual reality exposure therapy for fear of heights: clinicians’ attitudes become more positive after trying VRET. Front Psychol 2021;12. https://doi.org/10.3389/fpsyg.2021.671871.
Ma L, et al. Integrating virtual realities and psychotherapy: SWOT analysis on VR and MR based treatments of anxiety and stress-related disorders. Cogn Behav Ther. 2021;50(6):509–26. https://doi.org/10.1080/16506073.2021.1939410.
Langlet BS, Odegi D, Zandian M, Nolstam J, Södersten P, Bergh C. Virtual reality app for treating eating behavior in eating disorders: development and usability study. JMIR Serious Games 2021;9(2). https://doi.org/10.2196/24998.
Glegg SMN, et al. Evaluating change in virtual reality adoption for brain injury rehabilitation following knowledge translation. Disabil Rehabil Assist Technol. 2017;12(3):217–26. https://doi.org/10.3109/17483107.2015.1111944.
Sarkar U, Lee JE, Nguyen KH, Lisker S, Lyles CR. Barriers and facilitators to the implementation of virtual reality as a pain management modality in academic, community, and safety-net settings: qualitative analysis. J Med Internet Res 2021;23(9). https://doi.org/10.2196/26623.
Bryant L, et al. Opportunities for immersive virtual reality in rehabilitation: focus on communication disability. 2020.
Kramer TL, Pyne JM, Kimbrell TA, Savary PE, Smith JL, Jegley SM. Clinician perceptions of virtual reality to assess and treat returning veterans. Psychiatr Serv. 2010;61(11):1153–6.
Üstel P, et al. Acceptability and feasibility of peer specialist-delivered virtual reality job interview training for individuals with serious mental illness: a qualitative study. J Technol Hum Serv. 2021;39(3):219–31. https://doi.org/10.1080/15228835.2021.1915924.
Levac DE, et al. A comparison of virtual reality and active video game usage, attitudes and learning needs among therapists in Canada and the US. In: 2019 International Conference on Virtual Rehabilitation (ICVR). 2019. p. 1–7.
Algahtani M, Altameem A, Baig AR. An extended UTAUT2 model to explain the adoption of virtual reality technology in health centers_ an empirical study based in Riyadh. Int J Comput Sci Netw Secur. 2021;21(3):219–28.
Høeg ER, Scully CFR, Bruun-Pedersen JR, Serafin S. The reality of implementing virtual reality: a case study on the challenges of integrating vr-based rehabilitation, in Lecture Notes of the Institute for Computer Sciences, Social-Informatics and Telecommunications Engineering, LNICST, Springer, 2020, pp. 749–759. https://doi.org/10.1007/978-3-030-53294-9_58.
Lindner P, Miloff A, Zetterlund E, Reuterskiöld L, Andersson G, Carlbring P. Attitudes toward and familiarity with virtual reality therapy among practicing cognitive behavior therapists: a cross-sectional survey study in the era of consumer VR platforms. Front Psychol 2019;10. https://doi.org/10.3389/fpsyg.2019.00176.
Nwosu AC, Mills M, Roughneen S, Stanley S, Chapman L, Mason SR. Virtual reality in specialist palliative care: a feasibility study to enable clinical practice adoption. BMJ Support Palliat Care. 2021. https://doi.org/10.1136/bmjspcare-2020-002327.
Vincent C, Eberts M, Naik T, Gulick V, O’Hayer CV. Provider experiences of virtual reality in clinical treatment. PLoS One 2021;16(10). https://doi.org/10.1371/journal.pone.0259364.
Dahms R, Stamm O, Müller-Werden U. Developing a VR training program for geriatric patient with chronic back pain. 2019. Available: http://www.springer.com/series/7409.
Tennant M, McGillivray J, Youssef GJ, McCarthy MC, Clark TJ. Feasibility, acceptability, and clinical implementation of an immersive virtual reality intervention to address psychological well-being in children and adolescents with cancer. J Pediatr Oncol Nurs. 2020;37(4):265–77. https://doi.org/10.1177/1043454220917859.
Ford CG, Manegold EM, Randall CL, Aballay AM, Duncan CL. Assessing the feasibility of implementing low-cost virtual reality therapy during routine burn care. Burns. 2018;44(4):886–95. https://doi.org/10.1016/j.burns.2017.11.020.
Demers M, Chan Chun Kong D, Levin MF. Feasibility of incorporating functionally relevant virtual rehabilitation in sub-acute stroke care: perception of patients and clinicians. Disabil Rehabil Assist Technol. 2019;14(4):361–7. https://doi.org/10.1080/17483107.2018.1449019.
Levac D, et al. A knowledge translation intervention to enhance clinical application of a virtual reality system in stroke rehabilitation. BMC Health Serv Res. 2016;16(1):1–11. https://doi.org/10.1186/s12913-016-1807-6.
Proffitt R, Glegg S, Levac D, Lange B. End-user involvement in rehabilitation virtual reality implementation research. J Enabling Technol. 2019;13(2):92–100. https://doi.org/10.1108/JET-10-2018-0050.
Banerjee-Guénette P, Bigford S, Glegg SMN. Facilitating the implementation of virtual reality-based therapies in pediatric rehabilitation. Phys Occup Ther Pediatr. 2020;40(2):201–16. https://doi.org/10.1080/01942638.2019.1650867.
Davis K, Drey N, Gould D. What are scoping studies? A review of the nursing literature. Int J Nurs Stud. 2009;46(10):1386–400. https://doi.org/10.1016/j.ijnurstu.2009.02.010.
Easterlin MC, et al. Child and parent perspectives on the acceptability of virtual reality to mitigate medical trauma in an infusion center. Matern Child Health J. 2020;24(8):986–97. https://doi.org/10.1007/s10995-020-02955-x.
Levac D, Glegg SM, Camden C, Rivard LM, Missiuna C. Best practice recommendations for the development, implementation, and evaluation of online knowledge translation resources in rehabilitation. Phys Ther. 2015;95(4):648–62.
Presseau J, McCleary N, Lorencatto F, Patey AM, Grimshaw JM, Francis JJ. Action, actor, context, target, time (AACTT): a framework for specifying behavior. Implement Sci 2019;14(1). https://doi.org/10.1186/s13012-019-0951-x.
Eldredge LKB, Markham CM, Ruiter RA, Fernández ME, Kok G, Parcel GS. Planning health promotion programs: an intervention mapping approach. Hoboken: Wiley; 2016.
Proctor EK, Powell BJ, Mcmillen JC. Implementation strategies: recommendations for specifying and reporting, Implement Sci. 2013;8. Available: http://www.implementationscience.com/content/8/1/139.
Donaldson A, Lloyd DG, Gabbe BJ, Cook J, Finch CF. We have the Programme, what next? Planning the implementation of an injury prevention programme. Inj Prev. 2017;23(4):273–80. https://doi.org/10.1136/injuryprev-2015-041737.
Lincoln YS, Guba EG. But is it rigorous? Trustworthiness and authenticity in naturalistic evaluation. New Dir Program Eval. 1986;1986(30):73–84. https://doi.org/10.1002/ev.1427.
Acknowledgements
Not applicable.
Funding
Funding for this study was provided by Stichting Vrienden van Oldenkotte. They had no role in the study design; collection, analysis, or interpretation of the data; writing the manuscript; or decision to submit the paper for publication.
Author information
Authors and Affiliations
Contributions
MK, HK, and SK designed the study and wrote the protocol. MK conducted literature searches. MK and HK screened the titles and abstracts. MK analyzed the data and wrote the first draft of the manuscript. HK, SK, and YB contributed to the final manuscript and the authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendices
Appendix 1. Full electronic search strategy
Search terms
Set | Key concepts | Related terms |
|---|---|---|
Set 1 | Implementation | Adoption, dissemination, introduction, uptake |
Set 2 | Virtual reality (VR) | VR, Virtual technology, virtual environment |
Set 3 | Health care | Health, care, treatment |
Search string
TS = (implement* OR adopt* OR disseminat* OR introduc* OR “uptake”) AND TS = (“virtual reality” OR VR OR “virtual technolog*” OR “virtual environment”) AND TS = (health* OR “care” OR treat*)
Appendix 2. Study, technology, and implementation characteristics per study
Table 6 Study characteristics, characteristics of VR technology, and implementation characteristics per study
Authors, year, country | Study | VR technology | Implementation |
|---|---|---|---|
Study goal, design, and participants | VR technology, goal, target group, and setting | Implementation stage, strategies, target group, objectives, and outcomes | |
Algahtani, Altameem, and Baig, 2021; Saudi Arabia [49] | Goal: The study explores the current state of VR technology adoption, factors that influence such adoption, and the extent of this technology’s efficiency when it is used for vaccinating children Design: Quantitative cross sectional, experimental Participants: Workers in vaccination clinics (n = 186) survey—and pediatric patients (n = 6) experiment Data collection: Survey and experiment | VR technology and goal: VR eyewear that shows an amusing video that distracts children during vaccination Target group VR: pediatric patients Setting: Vaccination clinic | Stage: After implementation Target group implementation: Workers in health centers Objective: - Model: UTAUT2 Strategies: N/S Outcomes: Adoption, satisfaction, behavioral intention |
Banerjee-Guénette, Bigford, and Glegg, 2020; Canada [60] | Goal: Develop and evaluate the impact of a multifaceted KT intervention (KTI). An overview of (a) the theoretical determinants of occupational therapists’ and physical therapists’ intentions to use a variety of VR and other interactive technologies in practice and (b) their actual technology usage patterns Design: Quantitative Participants: Physical and occupational therapists (n = 11) Data collection: Survey | VR technology and goal: Nintendo Wii, WiiFit, Kinexct for XboX 360; in which the player is represented as an avatar. This system uses motion capture technology to allow full-body movements to control therapy-focused games developed with rehabilitation context in mind Target group VR: Rehabilitation patients Setting: Rehabilitation clinic | Stage: After implementation Target group implementation: Therapists Objective: N/S Model: Decomposed Theory of Planned Behavior + elements of Diffusion of Innovation Theory and Technology Acceptance Model (ADOPT-VR) Strategies: One-on-one mentoring sessions; Outcomes: Adoption and Acceptability |
Bryant, Bluff, Barnett, Hemsley, Nguyen, Jacobs, Power, Baily, Stubbs, and Lucas, 2020; Australia [45] | Goal: Explore the views of professionals with expertise in health, rehabilitation, and VR technology, on the populations that might benefit from VR-based rehabilitation, and potential barriers and facilitators to their use of VR Design: Qualitative Participants: Health professionals (n = 9) and VR technologist (n = 1) Data collection: Focus group and interview | VR technology and Goal: Immersive VR using a head-mounted display (not specified further—VR technology is developed based on the insights of this study) Target group VR: Rehabilitation patients Setting: Rehabilitation clinic | Stage: Before implementation Target group implementation: Health professionals in rehabilitation Objective: N/S Model: N/S Strategies: N/A Outcomes: - |
Cavenett, Baker, Waycott, Carrasco, Robertson, Vetere, and Hampson, 2018; Australia [36] | Goal: Explore factors that influence staff members when deploying new VR technology in residential aged care facilities Design: Qualitative Participants: Workers from Australian residential care facilities (n = 5) Data collection: Interviews | VR technology and goal: Commercial VR system with a headset, 2 3D cameras, 2 hand controllers. Aim is to let participants move things around in VR and stimulate physical activity Target group VR: Elderly at residential aged care facilities Setting: Residential aged care facilities | Stage: After implementation Target group implementation: Workers in residential aged care facilities Objective: N/S Model: N/S Strategies: N/S Outcomes: - |
Chung, Robinson, Johnson, Dowling, Chee, Yücel, and Segrave, 2022; Australia [34] | Goal: Explore the perspectives of staff working in the private mental health sector around the use of therapeutic VR, including potential implementation barriers and facilitators Design: Qualitative Participants: Clinicians (n = 14) and managers (n = 5) of a major private mental health hospital Data collection: Interviews | VR technology and goal: A HTC Vive system with a wireless head-mounted display and handheld controllers was utilized. VR scenarios were designed for OCD treatment Target group VR: Patients with Obsessive–compulsive disorder (OCD) Setting: Private mental health hospital | Stage: Before implementation Use of VR: VR only used as part of study, not in treatment Target group implementation: Clinicians Objective: N/S Model: Theory of Innovation Diffusion, CFIR and TDF Strategies: Treatment manuals; in-service training days; consultation opportunities with VR developers and early adopter services; Protocols to promote safe and ethical usage of VR Outcomes: - |
Dahms, Stamm, and Muller-Werdan, 2019; Germany [54] | Goal: Determine the process-identifying needs of a VR training program for geriatric patients with chronic backpain Design: Qualitative Participants: Experts (n = 4) physiotherapists and psychotherapists in an executive position of a hospital and rehabilitation center Data collection: Interviews | VR technology and goal: ViRST: Personalized and adaptive VR based on immersive interaction sequences and gamification; sensor-based presentation of content with dynamic, adaptive and personalized storytelling for therapeutic recommendations through multimodal interaction with the content (Multimodal Pain Therapy) Target group VR: Chronic back pain patients Setting: Hospital and rehabilitation center | Stage: Before implementation Target group implementation: Experts who care for and have daily contact with geriatric, chronic back pain patients Objective: N/S Model: N/S Strategies: N/A Outcomes: - |
Demers, Kong, and Levin, 2019; Canada [57] | Goal: Determine user satisfaction and safety of incorporating a low-cost virtual rehabilitation intervention as adjunctive therapeutic option for cognitive-motor upper limb rehabilitation in individuals with sub-acute stroke Design: Mixed-methods convergent parallel design: qualitative and quantitative cross-sectional Participants: Clinicians (n = 9) who are stroke program therapists and patients with a sub-acute stroke undergoing rehabilitation (n = 7) Data collection: Focus group, interviews and survey | VR technology and goal: Unity Pro software and Kineact II camera tracked arm, hand and trunk movements to interact with VR environment without a game controller. Projected on large screen. Participants played games sitting or standing with or without ambulatory aids. One smash blocks task and one shopper’s delight task (interactive grocery shopping) Target group VR: Stroke patients Setting: Rehabilitation clinic | Stage: Before implementation Target group implementation: N/S Objective: N/S Model: N/S Strategies: N/A Outcomes: Perceived usefulness, satisfaction |
Demers, Nguyen, Austin Ong, Xin Luo, Thuraisingam, Rubino, Levin, Kaizer, and Archambault, 2019; Canada [35] | Goal: Understand the perspectives of clinicians regarding an exergaming program (VR) to supplement stroke rehabilitation care Design: Qualitative Participants: Occupational and physiotherapists (n = 10) working in the stroke program at a rehabilitation hospital Data collection: Interviews | VR technology and goal: Exergaming program in VR: Jintronix and Meditouch HandTutor to supplement stroke care and address therapeutic goals (e.g., improving upper limb function, sitting balance and endurance) Target group VR: Stroke patients Setting: Rehabilitation hospital | Stage: After implementation Target group implementation: Clinicians Objective: N/S Model: N/S Strategies: Obtaining a dedicated room for VR; approval from hospital administration; establishing the referral process; purchasing equipment; hiring personal for VR Outcomes: - |
Easterlin, Berdahl, Rabizadeh, Spiegel, Agoratus, Hoover, and Dudovitz, 2020; USA [62] | Goal: Examining the acceptability of hypothetically using VR during an infusion appointment to help reduce medical trauma Design: Qualitative Participants: Patient-guardian dyads (n = 18) (pediatric IBD patients and parents) Data collection: Interviews | VR technology and goal: VR wear goggles to help reduce medical trauma (content not specified) Target group VR: Pediatric IBD patients Setting: Pediatric clinic | Stage: Before implementation Target group implementation: N/S Objective: N/S Model: N/S Strategies: N/A Outcomes: - |
Ford, Mangegold, Randall, Aballay, and Duncan, 2018; USA [56] | Goal: Evaluate key stakeholder (i.e., patients, providers) perceptions of feasibility, acceptability, and effectiveness for the use of low-cost VR technology during routine burn care with adult patients Design: Quantitative cross sectional and qualitative Participants: patients (n = 10) within burn care and providers (n = 8) who delivered the burn care Data collection: Survey and interviews | VR technology and goal: VR is used as a distraction during burn care. An iPod Touch was used to deliver the VR videos: choice of 8 VR applications (Table Mountain sunset, reindeer race, scuba diving, exploring Amsterdam, roller coaster, playing soccer, swinging through a city, or riding motocross) Target group VR: Burn patients Setting: Burn care clinic | Stage: Before implementation Target group implementation: Care providers of burn patients Objective: N/S Model: N/S Strategies: N/A Outcomes: Acceptability and Feasibility |
Glegg, Holsti, Stanton, Hanna, Velikonja, Ansley, Sartor, and Brum, 2017; Canada [43] | Goal: Evaluate the impact of knowledge translation (KT) on factors influencing virtual reality adoption and to identify support needs of therapists Design: Quantitative cross-sectional Participants: Physical, occupational, and rehabilitation therapists (n = 37) Data collection: Survey | VR technology and goal: A variety of VR and other interactive technology systems were already available to participants (not specified) Target group VR: Rehabilitation patients Setting: Brain injury rehabilitation centers | Stage: After implementation Target group implementation: Physical, occupational, and rehabilitation therapists Objective: Knowledge translation (KT) on factors influencing VR adoption and identify support needs of therapists Model: DTPB: Decomposed Theory of Planned Behavior (ADOPT-VR2 instrument) Strategies: Interactive education; clinical manual with goal setting, measuring client progress, developing client progress and evidence; Evidence synthesis; Sample goals; Overview of games and how to select goal-appropriate ones for clients; Information on isolating desired skills or grading VR activities for therapy Outcomes: Adoption and behavioral intention |
Høeg, Scully, Bruun-Pedersen, and Serafin, 2020; Denmark [50] | Goal: Determine the circumstances in which physiotherapists and occupational therapists would decide to use VR as part of the therapy. Additionally, evaluate the challenges faced with the implementation, including pain points related to the use of VR Design: Qualitative Participants: Physiotherapists (n = 4) Data collection: Interviews and observations | VR technology and goal: VR-based treatment tool for biking-based rehabilitation: Oculus Rift Consumer Version headset. Software is a set of 4 unique, digitally generated virtual landscapes; measuring the angular velocity of the foot-pedals on the training bike. Stimulating movement Target group VR: Rehabilitation patients Setting: Outpatient health center | Stage: After implementation Target group implementation: Physiotherapists in outpatients health centers Objective: N/S Model: N/S Strategies: N/S Outcomes: - |
Kramer, Jeffrey, Pyne, Timoty, Kimbrell, Savary, Jeffrey, Smith, and Jegley, 2010; USA [46] | Goal: Determine critical factors in the successful implementation of a VR intervention among veterans Design: Qualitative Participants: Clinicians (n = 18) from a Veterans Health Administration hospital Data collection: Focus groups | VR technology and goal: VR that offers an assessment method for OEF-OIF veterans by allowing for controlled immersion in a simulated combat environment while monitoring psychophysiological reactivity. The technology has also been used as an adjunct to exposure therapy and aims to improve PTSD symptoms among veterans Target group VR: Veterans Setting: Veterans Health Administration hospital (PTSD clinic, substance abuse treatment service residential program, and mental health clinic) | Stage: After implementation Target group implementation: Clinicians from a Veterans Health Administration hospital Objective: N/S Model: N/S Strategies: N/S Outcomes: - |
Langlet, Odegi, Zandian, Nolstam, Södersten, and Bergh, 2021; Sweden [42] | Goal: Evaluate the feasibility and usability of an immersive virtual reality technology administered through an app for use of patients with eating disorders Design: Quantitative cross sectional Participants: Eating disorder personnel (n = 19) and information technology personnel (n = 5) Data collection: Usability tests and survey | VR technology and goal: Participants handled virtual food and utensils on an app using immersive virtual reality technology comprising a headset and two hand controllers. The challenge consisted of a meal type (meatballs, potatoes, sauce, and lingonberries) that is typically difficult for patients with anorexia nervosa to eat in real life. Participants were instructed, via visual feedback from the app, to eat at a healthy rate, which is also a challenge for patients Target group VR: Anorexia Nervosa patients Setting: Eating disorder clinic | Stage: Before implementation Target group implementation: Eating disorder clinic personnel Objective: N/S Model: N/S Strategies: N/A Outcomes: Feasibility (and usability) |
Levac, Glegg, Pradhan, Foc, Espy, Chicklis, and Deutsch, 2019; USA [48] | Goal: Undertake a cross-country comparison of VR/AVG uptake to inform the content of educational interventions designed to promote implementation of these technologies into practice Design: Quantitative cross-sectional Participants: Physical- and occupational therapists in Canada and VS (n = 1490) Data collection: Survey | VR technology and goal: VR/AVG (active video gaming) in general healthcare (not specified) Target group VR: N/S Setting: General healthcare | Stage: After implementation Target group implementation: Physical- and occupational therapists Objective: N/S Model: Decomposed Theory of Planned Behavior (ADOPT-VR2 instrument) Strategies: N/S Outcomes: Uptake |
Levac and Miller, 2013; Canada [13] | Goal: Explore observations and insights from a sample of physical therapists working with children with acquired brain injury regarding practical implications of using the Wii as a physical therapy intervention Design: Qualitative Participants: Physical therapists (n = 6) at a children’s rehabilitation center Data collection: Interviews | VR technology and goal: Wii virtual reality (VR) interactive video gaming console: movement-based games to target motor impairments in a variety of patient populations Target group VR: Variety of patient populations (sample: children with acquired brain injury) Setting: Clinical rehabilitation practice and at home | Stage: After implementation Target group implementation: Physical therapists at children’s rehabilitation center Objective: N/S Model: N/S Strategies: Making time to reflect and understand how to use VR; Spend time considering the potential and added value of VR into practice; Time and effort to set up and maintain system, find treatment location and maintenance issues; Getting familiar with the technology to instruct patients in its use Outcomes: - |
Levac, Glegg, Sveistrup, Colquhoun, Miller, Finestone, DePaul, Harris, and Velikonja, 2016; USA [58] | Goal: (1) evaluate the impact of the intervention on therapists’ confidence related to VR knowledge and skills and perceptions of facilitators and barriers related to VR use; (2) assess the usability of the VR system; (3) obtain therapists’ perspectives about the KT intervention and VR use in practice; and finally, (4) measure the frequency of continued VR use following the KT intervention Design: Qualitative and quantitative cross-sectional Participants: Physical and occupational therapists (n = 11) Data collection: Focus groups and survey | VR technology and goal: Motion-capture technology enables players to view their mirror image in the virtual environment of the GestureTek Interactive Rehabilitation Exercise (IREX) software platform. Interaction with the virtual environment is through body movements to participate with games that address multiple upper extremity or full body movement goals, while motivating clients to participate Target group VR: Stroke rehabilitation patients Setting: Stroke rehabilitation units | Stage: After implementation Target group implementation: Physical- and occupational therapists Objective: The KT intervention designed to translate knowledge about use of the VR system to therapists in two stroke rehabilitation units Model: ADOPT-VR Strategies: E-learning modules (3 online modules provided foundational knowledge about clinical VR use); Hands-on learning (VR experience, training sessions, case scenarios); Experiential learning (use and reflect); Didactic reminders (weekly e-mails with “tips”for VR use); Mentorship (mentors to contact with questions or support needs) Outcomes: Uptake |
Lindner, Miloff, Zetterlund, Reuterskiöld, Andersson, and Carlbring, 2019; Sweden [51] | Goal: Survey attitudes toward and familiarity with VR and VRET among practicing cognitive behavior therapists attending a conference Design: Quantitative cross-sectional Participants: Psychologists, psychiatrists, social workers, nurses, and counselors (n = 185) Data collection: Survey | VR technology and goal: Virtual reality exposure therapy (VRET) for fear and anxiety on VR headset Target group VR: Therapists Setting: Used during a conference (normally used during treatment) | Stage: Before implementation Target group implementation: N/S Objective: N/S Model: N/S Strategies: N/A Outcomes: - |
Ma, Mor, Anderson, Baños, Botella, and Bouchard, 2021; Sweden [41] | Goal: Present an overview of current expert opinions on the use of virtual technologies in the treatment of anxiety and stress-related disorders Design: Quantitative cross-sectional Participants: Experts on VR and MR technology within psychotherapies (n = 14) Data collection: Survey | VR technology and goal: VR and MR technology use in treatment of anxiety and stress-related disorders (not specified) Target group VR: Patients with anxiety or stress-related disorders Setting: Clinics and within research projects | Stage: Before implementation Target group implementation: N/S Objective: N/S Model: N/S Strategies: N/A Outcomes: - |
Nguyen, Ong, Luo, Thuraisingam, Rubino, Levin, Kaizer, and Archambault, 2019; Canada [37] | Goal: Identify the facilitators and barriers perceived by clinicians to using an Exergaming Room as adjunct to conventional therapy Design: Qualitative Participants: Clinicians (n = 10); physical therapists and occupational therapists Data collection: Interviews | VR technology and goal: The Exergames Room contains two systems. The Jintronix is a VR rehabilitation software and it elicits purposeful movements that can be done in sitting or standing. The Meditouch HandTutor allows the repetition of functional movements within a game context, while providing augmented motion biofeedback Target group VR: Rehabilitation patients Setting: The Exergames Room in a hospital | Stage: After implementation Target group implementation: Rehabilitation patients Objective: N/S Model: N/S Strategies: N/S Outcomes: - |
Nwosu, Mills, Roughneen, Stanley, Chapman, and Rason, 2021; UK [52] | Goal: 1) explore the feasibility of implementing VR therapy, for patients and healthcare providers, in a hospital specialist inpatient palliative care unit and a hospice, and (2) to identify questions for organizations, to support VR adoption in palliative care Design: Quantitative cross-sectional Participants: Patients (n = 12) and healthcare providers (n = 3) Data collection: Survey | VR technology and goal: The Samsung Gear VR system was used in a hospital specialist palliative inpatient unit and a hospice. Patients and healthcare providers received VR distraction therapy Target group VR: Palliative patients Setting: Palliative inpatient unit | Stage: After implementation Target group implementation: Healthcare providers in palliative care units Objective: N/S Model: N/S Strategies: N/S Outcomes: Feasibility |
Ogourtsova, Archambault, and Lamontagne, 2019; Canada [38] | Goal: Explore the barriers and facilitators perceived by clinicians in the use of virtual reality for hemineglect assessment; and to identify features of an optimal virtual assessment Design: Qualitative and quantitative cross-sectional Participants: Clinicians (n = 11) and research experts in the field (n = 3) Data collection: Focus groups, interviews, and survey | VR technology and goal: VR for post-stroke unilateral spatial neglect assessment: VR-based USN assessment that could be implemented and used by clinicians in the management of post-stroke unilateral spatial neglect Target group VR: Post-stroke patients Setting: Healthcare clinic | Stage: After implementation Target group implementation: Clinicians Objective: N/S Model: N/S Strategies: N/S Outcomes: - |
Proffitt, Glegg, Levac, and Lange, 2019; USA [59] | Goal: Review four case examples from the authors’ collective experience of including end users in VR/AVG research to identify common benefits, challenges, and lessons learned Design: Quantitative cross-sectional and qualitative Participants: (1) therapists and clients with stroke; (2) OT students; (3) Clients and therapists; (4) Clients and therapists Data collection: Survey, interviews, observations, focus groups, and usability testing | VR technology and goal: Gesturetek IREX (interactive rehabilitation exercise system); Rapael SmartGlove; Adapted PlayStation2 controller; All VR systems related to rehabilitation Target group VR: Individuals with stroke, pro-bono clinic clients, adolescents and adults with hemiparesis, individuals with stroke/brain injury/amputations/older adults at risk for falls Setting: Inpatient stroke rehabilitation, pro-bono student-run outpatient clinic, home-based rehabilitation, outpatient clinic/hospital/home | Stage: After implementation Target group implementation: Therapists and clients Objective: N/S Model: N/S Strategies: N/S Outcomes: - |
Rimer, Husby, and Solem, 2021; Norway [40] | Goal: Testing whether modern, wireless, commercially available VR equipment with controller-free hand tracking could induce and reduce discomfort using scenarios designed for fear of heights. Also, the study tested if clinicians’ attitudes toward using VR in therapy changed after trying it themselves Design: Quantitative cross-sectional Participants: Clinicians (n = 74) and psychology students (n = 54) with clinical experience Data collection: Survey | VR technology and goal: VRET software: The program utilized the VR hardware Oculus Quest, which is a wireless head-mounted display (HMD). It included a controller-free hand-tracking feature, which enabled the use of hands as an input method to control the program. The software consisted of two different scenarios, which will be referred to as the “Lift” and the “Plank.” Target group VR: Patients with anxiety/phobia treatment Setting: Private and public health clinics | Stage: After implementation Target group implementation: Clinicians from private and public health clinics Objective: N/S Model: N/S Strategies: N/S Outcomes: - |
Sarkar, Lee, Nguyen, Lisker, and Lyles, 2021; USA [44] | Goal: Assess the readiness for VR in safety-net settings with a qualitative, theory-informed implementation science study Design: Qualitative Participants: Current VR users and non-users in safety-net health systems (n = 15) Data collection: Interviews | VR technology and goal: AppliedVR platform for pain treatment. A commercially available, previously validated VR technology platform (Not further specified) Target group VR: Chronic pain patients Setting: Safety-net sites—clinics | Stage: After implementation Target group implementation: Health care providers Objective: N/S Model: Consolidated Framework for Implementation Research (CFIR) Strategies: Specific orientation from staff in order to initiate VR use; Staff support for coaching and troubleshooting; Champions among clinicians who can share both evidence for VR and successful treatment experiences Outcomes: - |
Stamou, Gracia-Palacios, and Botella, 2019; Spain [39] | Goal: Assess the level of feasibility, acceptance, and practical parameters of the combination of VR and traditional CBT for PND Design: Pilot study – quantitative cross-sectional and qualitative Participants: Patients (n = 6) with depression, anxiety, post-natal depression or recurrent depression Data collection: Survey and interviews | VR technology and goal: VR system where they were exposed to a series of virtual stressors, while at the same time, they were asked to tidy up the virtual house. VR stressors can be manipulated by the therapist in terms of intensity (from 0 to 6), frequency, duration, and applied individually or simultaneously. They are divided into three main categories and include amongst others: loud music, telephone ringing, newborn baby crying, toddler reaching for medication, power outage, fire in the kitchen, next door neighbors arguing, and next-door party Target group VR: Depression and anxiety-related patient groups Setting: General Practice clinics | Stage: Before implementation Target group implementation: N/S Objective: N/S Model: N/S Strategies: N/A Outcomes: Feasibility and Acceptability |
Tennant, McGillivray, Youssef, McCarthy, and Clark, 2020; Australia [55] | Goal: 1. To evaluate the acceptability and feasibility of implementing an Immersive VR therapeutic intervention in an inpatient pediatric oncology setting, from the perspective of key stakeholders (i.e., oncology HCPs, patients, and parent healthcare providers); (2) to examine factors influencing VR adoption by HCPs, including barriers/facilitators to VR use with children who are seriously ill; (3) to explore user perspectives regarding the potential clinical utility of VR as an intervention to support psychological adjustment to hospitalization, including child VR content preferences Design: Quantitative Participants: Multidisciplinary oncology healthcare professionals (n = 30) and oncology inpatients (n = 90) Data collection: Survey | VR technology and goal: Immersive VR experiences were provided using a smartphone and VR headset and headphones. The intervention content involved original 360° video content. Participants viewed one of three virtual simulation experiences, including simulated travel to Australian national parks (i.e., nature experience), Australian zoos (i.e., animal experience), or global city tourist spots (i.e., travel experience). The goal is to support children’s needs during active cancer treatment, including to help regulate strong emotion, alleviate boredom, enhance mood, and provide a sense of escape from hospital, the experience of play, distraction from feared medical procedures, and physical symptom reduction Target group VR: Oncology inpatients (7–19 years) Setting: Children’s hospital and cancer center | Stage: Before implementation Target group implementation: Health care providers in children’s oncology care Objective: N/S Model: N/S Strategies: N/A Outcomes: Acceptability, adoption and feasibility |
Üstel, Smith, Blajeski, Johnson, Butler, Nicola-Adkins et al., 2021; USA [47] | Goal: Understand peer specialist beliefs about potential barriers and facilitators influencing peer-delivered VR-JIT Design: Qualitative Participants: Peer specialists (n = 34) Data collection: Focus groups | VR technology and goal: Virtual Reality Job Interview Training (VR-JIT) which is a computerized job interview simulator delivered via the Internet. VR-JIT was designed to improve interview skills. VR-JIT enables trainees to review an e-learning curriculum about job interview strategies and tips; complete an online job application for a fictional company called “Wondersmart,” and then repeatedly practice interviews with a virtual hiring manager named “Molly Porter.” Trainees choose their responses from scripted options that range from highly effective to highly ineffective and then speak them aloud to “Molly Porter” using the website’s speech recognition function Target group VR: Individuals with serious illness Setting: Peer specialist workspaces | Stage: Before implementation Target group implementation: Peer specialists Objective: N/S Model: Consolidated Framework for Implementation Research (CFIR) Strategies: N/A Outcomes: Acceptability and Feasibility |
Vincent, Eberts, Naik, Gulick, and O’Hayer, 2021, USA [53] | Goal: Explore the provider perception of the value of VR and identify barriers to Implementation among healthcare providers Design: Qualitative, cross-sectional Participants: Providers (n = 17) who have used VR as a therapeutic tool in the past year Data collection: Survey | VR technology and goal: VR as a treatment tool in psychiatry and pain management (not specified) Target group VR: Patients with psychiatric disorders or treated with pain management Setting: Community practice; medical clinic; research setting | Stage: After implementation Target group implementation: Healthcare providers Objective: N/S Model: N/S Strategies: Training about VR content in treatment and how to use VR (in person and online—about half a day); self-directed research Outcomes: - |
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Kouijzer, M.M.T.E., Kip, H., Bouman, Y.H.A. et al. Implementation of virtual reality in healthcare: a scoping review on the implementation process of virtual reality in various healthcare settings. Implement Sci Commun 4, 67 (2023). https://doi.org/10.1186/s43058-023-00442-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43058-023-00442-2