Abstract
Background
Early and accessible testing for influenza with point-of-care testing (POCT) can be a critical factor for deciding to begin antiviral treatment. More than 10,000 pharmacies across the USA offer Clinical Laboratory Improvement Amendments-waived POCT for infectious diseases, such as influenza A/B. Knowledge of barriers and facilitators to large-scale POCT implementation may be useful in scaling POCT for influenza test-and-treat services (Flu POCT). The objective of this study was to explore the experiences of pharmacists who were early adopters of Flu POCT and treatment under collaborative practice agreement in community pharmacy settings.
Methods
Qualitative research design with in-depth, semi-structured virtual video interviews of licensed US community pharmacists. Interview questions were derived from the Consolidated Framework for Implementation Research (CFIR). Interviewees were selected via a purposeful sampling of pharmacists who were enrolled in a nationwide clinical trial involving pharmacy-based influenza test-and-treat under a collaborative agreement. Interviews were recorded and transcribed. A deductive analytic approach was used via constructs from the CFIR.
Results
Six pharmacists were interviewed. Interviews ranged from 28 to 70 min, with an average length of 46 min. Four broad themes emerged from the data, and each had corresponding subthemes and supporting quotes: influence of the Flu POCT service characteristics on pharmacy implementation, influence of factors outside of the pharmacy setting in Flu POCT implementation, factors within the pharmacy setting influencing implementation, and process of implementing Flu POCT. A novel pharmacy-based Flu POCT implementation framework is presented.
Conclusions
Implementation of community pharmacy-based Flu POCT services is feasible; but, a thorough understanding of both barriers and facilitators to their implementation is needed to increase the spread and scale of these programs. Specifically, pharmacy stakeholders should focus efforts on increasing patient and provider awareness, pharmacist acceptance, leadership support, and support of health providers external to the pharmacy to improve implementation success.
Similar content being viewed by others
Background
The Centers for Disease Control and Prevention (CDC) estimate during the 2019–2020 influenza season more than 39 million people developed influenza, leading to more than 18 million healthcare provider visits. Annually, between 410,000 and 740,000 Americans are hospitalized due to influenza [1]. Additionally, complications from influenza include pneumonia and respiratory failure which can lead to worsening of chronic medical conditions. Influenza is estimated to be responsible for between 24,000 and 62,000 deaths annually [1].
Guidelines on the management of seasonal influenza from the CDC and Infectious Disease Society of America (IDSA) suggest beginning antiviral treatment within 48 h of symptom onset with suspected or documented influenza infection [2, 3]. For high-risk patients, including those who are hospitalized or may have severe consequences from influenza infection, antiviral treatment is suggested even if the preferred 48-hour window has passed [1]. Empiric treatment is also recommended for high-risk patients in situations where a community is experiencing co-circulation of influenza and SARS-CoV-2 [2].
Early and accessible testing for influenza can be a critical factor for deciding to begin antiviral treatment. Historically, viral culture laboratory testing was the standard of practice for influenza diagnosis. However, due to cost and turnaround time for results, its use is no longer recommended for initial or primary diagnosis [2]. The Clinical Laboratory Improvement Amendments of 1988 (CLIA) established quality standards for laboratory testing of specimens for diagnosis and treatment [4]. Point-of-care testing (POCT) for many infectious diseases is considered CLIA-waived, meaning they have a low risk of error and are simple to perform. POCT with rapid diagnostic tests has led to early influenza virus detection and a significant overall effect on improving patient health [5].
More than 10,000 pharmacies across the United States offer CLIA-waived POCT for infectious diseases, such as influenza A and B, and group A streptococcus [6]. In many states, pharmacists can prescribe treatment for patients after a positive test and thorough physical assessment via collaborative practice agreements or statewide protocols [7]. As defined by the CDC, a pharmacist collaborative practice agreement is a “formal agreement in which a licensed provider makes a diagnosis, supervises patient care, and refers patients to a pharmacist under a protocol that allows the pharmacist to perform specific patient care functions” [8]. Offering POCT and treatment for infectious diseases in a pharmacy setting can increase quick access to antiviral treatment, increase patient satisfaction with healthcare, improve antimicrobial stewardship, free-up physicians’ time for higher-acuity patients, and reduce unnecessary utilization of emergency departments [7]. Offering POCT in community pharmacies has demonstrated improvement in both patient health and patient-reported satisfaction [7].
According to Dulaney et al., community pharmacists reported willingness to perform POCT and recommend treatment for patients with influenza [9]. Participating pharmacists also believed they have the clinical knowledge to treat influenza and that pharmacy staff could be trained to assist with POCT services [9]. Moreover, training to perform POCT is now increasingly integrated into the Doctor of Pharmacy curricula [10].
When implementing CLIA-waived POCT in a community pharmacy setting several logistical challenges must be addressed, including establishing collaborative practice agreements, incorporating POCT into workflow, providing training for pharmacy staff, determining methods of remuneration, and following regulatory reporting requirements [11]. Barriers and facilitators to nationwide POCT implementation have yet to be explored in the published literature, but may be useful in POCT for influenza test-and-treat services. The objective of this study was to explore the experiences of pharmacists who were early adopters of Flu POCT and treatment under collaborative practice agreement in community pharmacy settings.
Methods
We used a qualitative research design with in-depth, semi-structured virtual video interviews of licensed U.S. community pharmacists. A phenomenological approach was selected to best understand the subjective experience of community pharmacists implementing the novel service of influenza POCT (Flu POCT) and treatment with antiviral therapy prior to the COVID-19 pandemic [12]. The University of Tennessee Institutional Review Board approved this study in January 2020 (20-07309-XM).
A semi-structured interview guide was developed by experts in influenza, POCT, and community pharmacy. Questions were derived from the Consolidated Framework for Implementation Research (CFIR), and the instrument was adapted based on an expert panel comprised of clinicians (e.g., PharmD, MD), researchers, and pharmacy leadership in line with guidance from the CFIR Research Team-Center for Clinical Management Research [13]. The interview guide was first drafted by a University researcher familiar with the topic using the CFIR website (https://cfirguide.org) interview guide tool. Subsequently, the document was shared with the expert panel and the instrument was further truncated. Interviews occurred in the Spring of 2020 by two trained researchers (KH and CC). Interview sessions were audio-recorded digitally and professionally transcribed by a third-party transcription service. Interviews were conducted over virtual videoconferencing technology, recorded, and subsequently transcribed. Field notes were also collected during interviews to note non-verbal expressions and interactions and incorporated into the data analysis process.
Interviewees were selected via a purposeful sampling of pharmacists who were enrolled in a nationwide clinical trial involving pharmacy-based influenza test-and-treat under a collaborative practice agreement. Flu POCT implementation champions known to the researchers were selected as part of the stratified sample of pharmacists, which included varying geographic locations, sex, organizational roles, and practice setting (i.e., chain or independent pharmacy). Recruitment occurred over email to each of the study site organizations and continued until a point of saturation whereby no new themes emerged with subsequent focus groups [14].
A deductive analytic approach was used via constructs from the CFIR [13]. Two coders trained and experienced in qualitative research methods (KH and KM) coded two transcripts together using the CFIR codebook to ensure coding consistency, and then coded the remaining transcripts independently. A reflexive approach was used by which data analysis took place alongside data collection so that the interview guide and approach could be modified. Both coders were faculty members at US colleges of pharmacy who specialized in community practice. Once researcher was trained, credentialed, and experienced in implementation science. Transcripts and field notes were uploaded into a qualitative analytic software (NVivo, Burlington, MA), which was used to assign codes and develop themes. Lincoln and Guba's criteria for quality in qualitative research and the Consolidated criteria for reporting qualitative research (COREQ) checklist were used to ensure data collection and analytical rigor [15, 16]. A third member of the research team assisted in the resolution of disputes during the thematic analysis process. Prior to finalizing themes, participant checking occurred by sharing these pre-final themes with two of the interviewees for their feedback—however, given the limited time availability of the participants, transcripts were not returned to the participants for review.
Results
Six participants were interviewed, one for each of the pharmacy organizations approached. Demographics for interviewees are listed in Table 1. Interviews ranged from 28 to 70 min, with an average length of 46 min, and were conducted at the participants’ homes or pharmacies. Four broad themes emerged from the data, and each had corresponding subthemes and supporting quotes (Table 2).
Theme 1: Influence of the Flu POCT service characteristics on pharmacy implementation
Relative advantage of Flu POCT service over other pharmacy services
This subtheme centered on participants’ perceptions of the advantage of implementing Flu POCT in relation to other pharmacy services. Participants opted to implement pharmacist-delivered Flu POCT over spending time in other pharmacy services for reasons of professional satisfaction by means of providing direct patient care, ability to serve new patients within the pharmacy, and offering services not offered at other pharmacies. Participants noted unanticipated facilitator for implementation was that the service primarily attracted new patients to the pharmacy.
Complexity of Flu POCT service over other pharmacy services
Flu POCT complexity centered on workflow integration, sample collection, and test supply procurement. Workflow integration of Flu POCT test-and-treat was customized to each pharmacy and required small changes, mostly in preparing the team how to handle the time when the pharmacist stepped away from their computer terminal and away from drug dispensing workflow. It was noted that these changes were similar to those made when first integrating vaccinations into workflow. Participants indicated initial staff pharmacist hesitance to perform sample collection via intranasal swab, but this was overcome with training and increasing experience. A major hurdle in the implementation of Flu POCT was obtaining the testing device, something not normal to pharmacy inventory, and this delayed implementation for some participants. In these instances, the gap between procurement of the Flu POCT device and pharmacist training served as an additional barrier as there became a need to refresh pharmacists on previously taught materials while awaiting Flu POCT machines and supplies.
Theme 2: Influence of factors outside of the pharmacy setting in Flu POCT implementation
Patient needs and resources
Both patient needs and barriers to meeting those needs were discussed. Specific to patient needs, participants noted that patients prioritize convenience, speed of care, and service access, but were mostly unaware of the pharmacy’s ability to meet these needs with the Flu POCT service. Participants articulated most patients using the Flu POCT service were not patients of the pharmacy, but had come to the pharmacy based on word-of-mouth recommendations or advertising. A resounding barrier among participants was the lack of patient awareness that pharmacists can perform Flu POCT. Similarly, for participants who had performed Flu POCT for one or more previous seasons, they noted how word of mouth, advertising, referrals, and social media facilitated awareness of how this service met patient demands for convenience and speed of care. It was also noted how the SARS-CoV-2 pandemic raised awareness of the expanded role of the pharmacist and how this may facilitate further expansion of the Flu POCT.
Pharmacy networks with other healthcare settings
This subtheme centered on the degree to which the pharmacy’s network of prescribers, hospitals, and medical offices impacted implementation. Participants noted in some cases there was initial resistance to participants performing Flu POCT, but that this was usually limited to a single medical practice or prescriber and overcome with proactive communication and time. Related to communication, participants emphasized the importance of communicating Flu POCT care plans to the patient’s primary care physician over telephone or fax as a key policy of their service.
Peer pressure among pharmacy competition
Broadly participants discussed the challenges of community pharmacy’s current business model and the need to expand or develop new patient care services offered. Participants at independent pharmacies noted the need to offer services not seen by the national pharmacy chains to differentiate themselves. Participants at chain pharmacies noted that they too were in competition, but with both the other chain pharmacies and independent pharmacies.
External policies and incentives
Both future third-party reimbursement potential and advancing scope of practice were facilitators for Flu POCT. Participants noted that continued national and state-specific conversations around third party payment models drove interest from pharmacy leadership as a supplement to cash-based payment models. Also, the provision of a prescription antiviral after receiving a positive flu result and corresponding patient assessment (rather than the result alone without treatment) was essential to program success; therefore, working within states allowing expanded scope of practice or broad collaborative practice agreement rules facilitated both implementation and scaling of services. Participants noted that even with the regulatory ability to both test and treat influenza, there sometimes existed a barrier in finding a collaborating physician to oversee the program and partner under a collaborative practice agreement.
Theme 3: Factors within the pharmacy setting influencing implementation
Network and communication within the pharmacy
This subtheme refers to the informal and formal communication strategies used by participants within their pharmacy. Generally, independent pharmacies used a more informal communication method (e.g., text messages, unscheduled conversations) to implement and sustain Flu POCT, whereas chains used existing formal communication methods (e.g., messaging campaigns, scheduled and routinized emails, scheduled visits). Leadership and front-line communication were noted to be critical to success. Communication across settings generally occurred over email and occasionally telephone. Face-to-face communication happened most often between front line staff members or between members of the leadership team and was due to the close physical proximity of those individuals. However, these siloed communication loops were not found to serve as a barrier for implementation.
Culture of the pharmacy
The culture of pharmacies implementing Flu POCT was described as innovative, highly efficient, and clinically focused. Participants considered their organizations as “leaders of the pack,” and expressed pride in their innovative approaches to the practice of pharmacy. Overall the pharmacies were noted to have characteristics in line with Rogers’ definition of Early Adopter and Innovator organizations [17]. Organizational priorities aligned with advanced and clinically focused services, and front-line staff reflected those priorities. Participants were noted to proactively seek out new opportunities to provide patient care as it positively affected their quality of work life (QOWL). These pharmacies also were concurrently implementing other novel patient care services concurrently with Flu POCT. Participants noted the synergetic interplay between the other clinical services offered at the pharmacy, noting that more and varying clinical services offered at the pharmacy facilitated implementation, rather than served as a distraction or competition for Flu POCT (e.g., Flu POCT services complimented vaccines and medication therapy management services).
Implementation climate of the pharmacy
The implementation climate of the pharmacy is the “shared perception among intended users of an innovation, of the extent to which an organization's implementation policies and practices encourage, cultivate, and reward innovation use” [18]. Like pharmacy cultures, organizational climates were noted to be supportive of innovation with support for new initiatives. Participants who had organizational leadership roles noted the importance of implementing new patient care services as a part of their overall organizational strategy. Participants felt their pharmacy organizations prioritized initiatives which embraced new roles in public health. Policies and procedures from past, successful patient care service implementations enabled Flu POCT implementation.
Incentives were sometimes provided by organizations to support implementation—but this was not seen across all pharmacies. Reasoning to not specifically incentivize their staff centered on relying on the intrinsic motivation of pharmacists to take on new clinical services for their own quality of work life and professional satisfaction, and this was found to be a sufficient incentive for those pharmacies using that incentive. This concept of professional satisfaction was articulated by both management and front-line pharmacists.
Participants noted that Flu POCT was overall fully compatible with existing workflow, work tasks, and physical layout of the pharmacy; although some minor workflow adaptations were required. Some specific physical aspects required included a private patient care room located in proximity or attached to the pharmacy department itself. It was also compatible with pharmacist views of their own professional responsibilities and professional capabilities.
Pharmacy readiness for implementation
Participants noted readiness for implementation revolved around a few core items: advertising and patient awareness, training and education, and testing equipment. Pharmacies with longer experience providing Flu POCT had achieved each of these items; similarly, those who had not yet begun testing (despite a high degree of willingness) lacked the majority of the three.
Engagement from top-level management teams was a key facilitator for implementation. This was especially true given the unique circumstance whereby patients were unaware of the pharmacist-delivered service. Marketing and advertising were two areas in particular where collaboration between departments was required and was largely organized by upper management and leadership. This included social media, flyers, bag stuffers, billboards, radio advertisements, and store signage. Furthermore, top-level management and leadership also organized and facilitated training & education for their pharmacy staff and procured testing supplies and equipment.
Access to both the testing equipment, supplies, and supporting training and education were also noted to be crucial elements for successful implementation. As most pharmacy suppliers do not carry POCT equipment or supplies, new supply chains or ordering procedures needed to be developed for most pharmacies—causing several pharmacies to have initial delays in implementation. Similarly, despite having foundational knowledge in therapeutics and pathophysiology (including infectious diseases, medical microbiology, and public health), most community pharmacy practices do not involve routine use of the knowledge required for Flu POCT. Therefore, participants referred to the value of “refresher” courses in infectious diseases, laboratory diagnostics, and related administrative topics (e.g., credentialing, regulatory policies, medical billing).
Theme 4: Process of implementing Flu POCT
Planning
Planning was noted to be detailed and involved the creation of new policies and procedures in line with other pharmacy-based services. Planning was mostly performed in a top-down manner, with pharmacy ownership or corporate leadership being responsible for developing and enforcing these policies and procedures.
Engaging
Generally, engaging participants and their support staff in Flu POCT implementation was straightforward and not resource-intensive. Given recent shifts within the pharmacy profession toward services that offer direct patient care, pharmacy staff enthusiastically participated in the implementation and scaling of the program. Though, several interviews noted a persistent minority of those who do not embrace change to their work tasks like Flu POCT, despite social norms supporting Flu POCT,
Executing
Participants who had already implemented POCT in years prior noted that despite the impact of COVID-19 on the flu season, patient demand grew. For those just beginning the implementation, they noted how positive patient feedback facilitated service rollout and staff enthusiasm in implementation.
Reflecting and evaluating
Goals and measures of success for Flu POCT varied depending on the maturity of the pharmacy’s Flu POCT service. Some pharmacies set a goal of a specific number of tests, while others found setting such a goal difficult because of the variability of the flu season year-to-year. When discussing financial goals, participants articulated their goals of expanding current patient care service offerings and “breaking even” on the cost of the program.
Generally, most measures of success centered around improving patient care and diversifying pharmacy service offerings.
Participants noted another goal was to set up a lean experiment model centered on the voice of the consumer (i.e., to test the service using the minimum amount of resources to see if there was enough patient demand in the community). Given the novelty of Flu POCT as a service and of a community pharmacy as an acute care access point, participants used the service to test patient demand and feasibility.
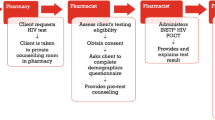
Conceptual framework of implementation facilitators to community pharmacist-delivered Flu POCT test and treat program implementation
Figure 1 represents the resulting conceptual framework developed from the semi-structured interview results. Four main facilitators were present: patient demand, pharmacy workflow integration, supportive organizational climate, and supportive network of health providers external to the pharmacy. Each of these main facilitators was mediated by at least one other variable, which included (a) patient and provider awareness, (b) pharmacist acceptance, (c) leadership support, (d) protocol-driven collaborative practice agreement solely for Flu POCT test-and-treat, (e) and sharing patient load during peak season/outside normal clinic hours. Of note, these latter two mediators (mediators “d” and “e”) related to the broader concept of built trust between the pharmacist and other healthcare providers. The first of these two mediators, protocol-driven collaborative practice agreement solely for Flu POCT test-and-treat, refers to the overseeing physician’s comfortability with delegating responsibilities to a pharmacist.
The simplicity of the Flu POCT protocols used by the participants, including patient assessment, laboratory result interpretation, and prescribing guidelines, facilitated trust where prior to this collaborative practice agreement there was none. Although it is standard practice for nurse practitioners and physician assistants to work under these collaborative agreements, the inclusion of a pharmacist in such an agreement is novel and therefore may represent additional risk or liability at first to a physician who previously had not collaborated with a pharmacist. The second mediator, sharing patient load during peak season/outside normal clinic hours, was a downstream mediator from the use of the collaborative practice agreement. Once the Flu POCT service had begun and patient experiences became known in the community, other clinicians within the community increased their trust in the service such that they saw an opportunity to refer low complexity cases to the pharmacist in a way that closely mirrors how clinicians refer routine vaccinations to community pharmacies presently to offload low complexity workload. Finally, a series of implementation targets are listed within the framework.
Discussion
Emerging evidence suggests that community pharmacies may serve as a key, underutilized care access point for acute infectious disease prevention, testing, and treatment [7, 19,20,21]. However, widespread implementation and scale of such community pharmacy-based POCT services, similar to what has been seen in pharmacy-based immunization services, will be dependent on a thorough understanding of barriers and facilitators to the service. To this end, we conducted interviews with pharmacists in a nationwide sample as part of a contextual inquiry to elucidate these barriers and facilitators. In our study, pharmacy sites ranged from local independent pharmacies to nationwide chains with differing patient populations. The results provide insights into the pharmacist’s point of view on Flu POCT in a community-based setting just prior to the COVID-19 pandemic. Such data will be of use to payers, researchers, and healthcare professionals as they seek to identify new ways to bolster public health efforts during and beyond the ongoing pandemic.
The study also provides deeper insights to existing published research and expert opinion which can be found in the literature. Pharmacist’s growing acceptance of POCT services can be represented by the over 5,000 pharmacists who have been credentialed by a nationally recognized POCT certificate program through 2020 [19]. POCT service workflow compatibility has also been researched previously and found to be in line with time spent on other clinical pharmacy activities, including pharmacy-based immunization services (ranging between 2.6 and 12.7 min) [19, 20, 22]. According to participants in this study and in the previously published literature, obtaining a collaborative practice agreement continues to be a substantial barrier due to a “unfamiliarity with statues and pharmacist capabilities; although, in general, physician-pharmacist collaborative practice under a collaborative practice agreement continues to grow across the USA [8, 23]. To this end, the study also presents a novel conceptual framework which ties salient pieces of Flu POCT implementation together. Of note, researchers and those responsible for implementing these services within community pharmacies can use the “Implementation Targets” within the framework as either a checklist for assessment or outline for planning.
The potential public health benefit of the community pharmacy is primarily that of patient accessibility [24]. Accessibility in this context refers to geographical location, hours of operation, and overall cost of the service. Based on a previous study, 92% of the US population live within 5 miles of a pharmacy [25]. Moreover, patients frequent their community pharmacist more often than their primary care physician [26]. A 2020 study also reported that 43.9% of patients sought care from a pharmacy outside of doctor’s office hours [21].
Community pharmacy-based POCT’s impact on public health has been studied to a great extent in the published literature. Several efficacy studies have shown the benefits of POCT test-and-treat in the community pharmacy setting. Results from a collaborative physician-pharmacist Flu POCT test-and-treat for patients presenting with influenza-like illness (ILI) across 55 pharmacies demonstrated the service’s feasibility and acceptability during the 2013–2014 influenza season. In total, 121 patients were screened within the program, 35% of whom did not have a primary care physician and about 40% were seeking care outside of normal clinic office hours. Of note, 37% of patients did not meet eligibility for the service according to the collaborative practice protocol and were referred to their physician or an urgent care for further evaluation. Just over 1-in-10 patients were provided oseltamivir based on physical assessment and positive Flu POCT result, and at follow-up, only 3% of those patients reported worsening symptoms and were referred for further medical care [27]. Although racial and ethnic data was not available in this study, these findings do indicate that a substantial proportion (about 2-in-5) had access to this service despite an existing barrier (e.g., lacking a primary care physician or being unable to seek care during normal business hours). In general, retail care settings have generally increased care access, at lower costs, with similar quality across select preventive and acute care conditions and have been [28, 29]. When looking specifically at retail clinics, the largest age group using these services are between 18 and 44 years old who lacked a primary care provider and that these settings are primarily located in non-medically underserved areas [30]. In comparison, community pharmacies are found almost equally across both medically underserved and non-underserved areas—possibly representing greater care access to a more diverse patient population [31, 32]. However, given the nascency of these pharmacist-provided collaborative care services (i.e., Flu POCT), the specific impact of health equity and disparities has yet to be investigated.
Similarly, another study in 2016 community pharmacy-based study resulted in 40% of patients testing positively for influenza using POCT in combination with a thorough physical assessment. Of those patients, 63% were prescribed oseltamivir under a collaborative practice agreement directly from the pharmacy and over-the-counter medications were provided to 85% of patients for symptom management [33]. Pharmacists were able to follow up with 56% of these patients, all of whom were recovering with a noted decrease in flu symptoms. In a more recent study performed across 6 states and 6 pharmacy chains, 93.8% of the flu-positive patients were able to obtain an antiviral prescription per collaborative practice agreement and 88% of negative tests received over-the-counter recommendations [19]. Of these patients, 80% had improved symptoms within 24–48 h of receiving a Flu POCT.
There were limitations to this study. Given its qualitative research methodology approach, generalization of the results to the entire population of community pharmacists is not possible. A future, follow-up study which uses the present study’s results to develop and disseminate a cross-sectional questionnaire would be best suited in establishing generalizability. Qualitative research is also highly dependent upon the data analysis team and their qualifications. In the case of the present study, this limitation was mitigated in part by both data coders (KH and KM) having been trained in and previously published on qualitative research methodology, while also being licensed community pharmacists with POCT experience.
Conclusion
Implementation of community pharmacy-based Flu POCT services, which include prescribing of antivirals under collaborative practice laws, is feasible; but a thorough understanding of both barriers and facilitators to their implementation are needed to increase the spread and scale of these programs. Specifically, pharmacies should focus efforts on increasing patient and provider awareness, pharmacist acceptance, leadership support, and support of health providers external to the pharmacy to improve implementation success.
Availability of data and materials
Given the qualitative data presented here, size and characteristics of the sample and disclosure of data and material will compromise the confidentiality of the research participants. To protect the anonymity of their responses, data and material will not be made publicly available. However, requests for data may be made to the corresponding author.
Abbreviations
- PBM:
-
Pharmacy benefits manager
- CLIA:
-
Clinical Laboratory Improvement Amendments
- POCT:
-
Point-of-care test
- CFIR:
-
Consolidated Framework for Implementation Research
- CDC:
-
Centers for Disease Control and Prevention
- IDSA:
-
Infectious Disease Society of America
- COREQ:
-
Consolidated criteria for reporting qualitative research
- QOWL:
-
Quality of work life
- ILI:
-
Influenza-like illness
References
2021-2022 U.S. flu season: Preliminary in-season burden estimates. Centers for Disease Control and Prevention. https://www.cdc.gov/flu/about/burden/preliminary-in-season-estimates.htm. Published January 13, 2022. Accessed 21 Jan 2022.
Uyeki TM, Bernstein HH, Bradley JS, et al. Clinical practice guidelines by the Infectious Diseases Society of America: 2018 update on diagnosis, treatment, chemoprophylaxis, and institutional outbreak management of seasonal influenza. Clin Infect Dis. 2019;68(6):e1–e47.
Influenza Antiviral Medications: Summary for Clinicians. Centers for Disease Control and Prevention. https://www.cdc.gov/flu/professionals/antivirals/summary-clinicians.htm. Published December 3, 2021. Accessed 21 Jan 2022.
Clinical Laboratory Improvement Amendments (CLIA). Centers for Medicare & Medicaid Services. https://www.cms.gov/Regulations-and-Guidance/Legislation/CLIA/. Published December 1, 2021. Accessed 21 Jan 2022.
Rapid diagnostic testing for influenza: Information for Clinical Laboratory Directors. Centers for Disease Control and Prevention. https://www.cdc.gov/flu/professionals/diagnosis/rapidlab.htm. Published February 4, 2021. Accessed 21 Jan 2022.
Klepser ME, Adams AJ, Srnis P, et al. US community pharmacies as CLIA-waived facilities: prevalence, dispersion, and impact on patient access to testing. Res Social Adm Pharm. 2016;12(4):614–21.
Herbin SR, Klepser DG, Klepser ME. Pharmacy-based infectious disease management programs incorporating CLIA-waived point-of-care tests. J Clin Microbiol. 2020;58(5):e00726–19.
Centers for Disease Control and Prevention. Advancing Team-Based Care Through Collaborative Practice Agreements: A Resource and Implementation Guide for Adding Pharmacists to the Care Team. Atlanta: Centers for Disease Control and Prevention, U.S. Department of Health and Human Services; 2017.
Dulaney K, Hohmeier K, Fisher C, et al. Exploring pharmacists’ perceptions regarding influenza and streptococcal testing within a chain pharmacy. J Am Pharm Assoc. 2018;58(4):438–41.
McKeirnan K, Czapinski J, Bertsch T, et al. Training student pharmacists to perform point-of-care testing. Am J Pharm Educ. 2019;83(7):Article 7031.
Anderson M. POCT regulatory compliance: What is it and how does it impact you. Crit Care Nurs Q. 2001;24(1):1–6.
Teherani A, Martimianakis T, Stenfors-Hayes T, et al. Choosing a qualitative research approach. J Grad Med Educ. 2015;7(4):669–70.
Damschroder LJ, Aron DC, Keith RE, et al. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci. 2009;4(1):1–15.
Francis JJ, Johnston M, Robertson C, et al. What is an adequate sample size? Operationalising data saturation for theory-based interview studies. Psychol Health. 2010;25(10):1229–45.
Guba EG, Lincoln YS. Competing paradigms in qualitative research. Handbook Qual Res. 1994;2(163-194):105.
Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. International J Qual Health Care. 2007;19(6):349–57.
Rogers EM, Singhal A, Quinlan MM. Diffusion of innovations. New York: Routledge; 2014. p. 432–48. https://doi.org/10.4324/9780203710753.
Weiner BJ, Belden CM, Bergmire DM, et al. The meaning and measurement of implementation climate. Implement Sci. 2011;6(1):1–12.
Klepser DG, Klepser ME, Smith JK, et al. Utilization of influenza and streptococcal pharyngitis point-of-care testing in the community pharmacy practice setting. Res Social Adm Pharm. 2018;14(4):356–9.
Klepser ME, Adams AJ. Pharmacy-based management of influenza: lessons learned from research. Int J Pharm Pract. 2018;26(6):573–8.
Kirby J, Mousa N. Evaluating the impact of influenza and streptococcus point-of-care testing and collaborative practice prescribing in a community pharmacy setting. J Am Pharm Assoc. 2020;60(3):S70–5.
Corn CE, Klepser DG, Dering-Anderson, et al. Observation of a pharmacist-conducted group A streptococcal pharyngitis point-of-care test: a time and motion study. J Pharm Pract. 2018;31(3):284–91.
Klepser DG, Klepser ME. Point-of-care testing in the pharmacy: how is the field evolving? Expert Rev Mol Diagn. 2018;18(1):5–6.
Gubbins PO, Klepser ME, Adams AJ, et al. Potential for pharmacy–public health collaborations using pharmacy-based point-of-care testing services for infectious diseases. J Public Health Manag Pract. 2017;23(6):593–600.
NACDS 2010-2011 Chain Pharmacy Industry Profile illustrates pharmacy value. Drug Topics. September 21, 2010. Available at: https://www.drugtop-ics.com/top-news/nacds-2010-2011-chain-pharmacy-industry-profile-illus-trates-pharmacy-value. Accessed 29 Dec 2021
Berenbrok LA, Gabriel N, Coley KC, et al. Evaluation of frequency of encounters with primary care physicians vs visits to community pharmacies among medicare beneficiaries. JAMA Netw Open. 2020;3(7):e209132.
Klepser ME, Klepser DG, Dering-Anderson AM, et al. Effectiveness of a pharmacist-physician collaborative program to manage influenza-like illness. J Am Pharm Assoc. 2016;56(1):14–21.
Martsolf G, Fingar KR, Coffey R, Kandrack R, Charland T, Eibner C, et al. Association between the opening of retail clinics and low-acuity emergency department visits. Ann Emerg Med. 2017;69(4):397–403.
Mehrotra A, Gidengil CA, Setodji CM, et al. Antibiotic prescribing for respiratory infections at retail clinics, physician practices, and emergency departments. Am J Manag Care. 2015;21(4):294–302.
RAND Corporation. The Evolving Role of Retail Clinics. Accessed at: https://www.rand.org/pubs/research_briefs/RB9491-2.html. Accessed on: 30 June 2022.
Murphy PA, Frazee SG, Cantlin JP, et al. Pharmacy provision of influenza vaccinations in medically underserved communities. J Am Pharm Assoc. 2012;52(1):67–70.
Burson RC, Buttenheim AM, Armstrong A, Feemster KA. Community pharmacies as sites of adult vaccination: a systematic review. Hum Vaccin Immunother. 2016;12(12):3146–59.
Papastergiou J, Folkins C, Li W, et al. Community pharmacy rapid influenza A and B screening: a novel approach to expedite patient access to care and improve clinical outcomes. Can Pharm J/Rev Des Pharm Du Can. 2016;149(2):83–9.
Acknowledgements
The research team would like to acknowledge and thank the following individuals from Genentech for their support and contributions to the project, Dr. Rita de Cassia Castro, Dr. Steven Cages, and Dr. Mitra Sadeghi.
Funding
Research was made possible by a grant from Genentech, Inc.
Author information
Authors and Affiliations
Contributions
Concept and design (KH, KM); analysis and interpretation of data (KH, KM); drafting of the manuscript (KH, KM, JA, MK, CC, DK); critical revision of the manuscript for important intellectual content (DK, SK, MK); provision of patients or study materials (SK); administrative, technical, or logistic support (SK); and supervision (MK, SK, DK). The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Research was approved by the University of Tennessee Health Science Center Institutional Review Board (Memphis, TN).
Consent for publication
Not applicable.
Competing interests
Michael Klepser receives royalties from the National Association of State Pharmacy Associations for a pharmacy-based point-of-care training program. He also has received grant funding from Janssen and conducts market consultation for Qorvo, Inc.
Donald G. Klepser receives royalties from the National Association of State Pharmacy Associations for a pharmacy-based point-of-care training program. He also conducts market consultation for Roche Diagnostics, Quidel, Diasorin, and Qorvo, Inc. He serves as a clinical advisor board member and receives honoraria from FDS/Amplicare.
Kenneth C. Hohmeier conducts market consultation for Qorvo, Inc. He serves as a clinical advisor board member and receives honoraria from FDS/Amplicare.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Semi-Structed Interview Guide.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Hohmeier, K.C., McKeirnan, K., Akers, J. et al. Implementing community pharmacy-based influenza point-of-care test-and-treat under collaborative practice agreement. Implement Sci Commun 3, 77 (2022). https://doi.org/10.1186/s43058-022-00324-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43058-022-00324-z