Abstract
Background
Patient navigation (PN) is an evidence-based practice that involves assessing and addressing individual barriers to care for patients. While PN has shown effectiveness in numerous studies, designing successful, sustainable PN programs has remained challenging for many healthcare organizations. The purpose of the present study was to examine implementation factors for successful PN programs to optimize the sustainability of PN services across cancer care settings in the USA.
Methods
Data were collected via semi-structured interviews with PN stakeholders (n=17) from diverse cancer care settings. Thematic content analysis was conducted by deductively coding major themes based on constructs from the Exploration-Preparation-Implementation-Sustainability framework and by inductively coding emergent themes.
Results
Facilitators in the outer context included payer guidelines, accreditation requirements, community partnerships, and demonstrated need and demand for services. Inner context factors such as alignment with organizational and leadership priorities, appropriate staff support and workloads, and relative advantage were important to program success. Innovation characteristics such as the presence of innovation champions, clear role and scope of practice, clear protocols, strong communication channels, and innovation fit were facilitators of program success. Community-Academic partnerships and funding stability also emerged as facilitators for program sustainability.
Conclusion
Our qualitative analysis from a diverse sample of PN stakeholders and programs across the USA supports intentional use of implementation theory to design PN programs to optimize implementation success.
Similar content being viewed by others
Background
Patient navigation (PN) is an evidence-based practice to reduce disparities in cancer outcomes and involves individual assessment and resolution of barriers to care [1]. Cancer PN has been effective in reducing time from screening to definitive diagnosis [2], increasing adherence to recommended treatment [3], and improving patient satisfaction [4, 5]. Research suggests that PN is most effective for patients with clear risk factors associated with delays to care, such as comorbid conditions, low socioeconomic status, and low educational attainment [6]. PN has also been shown to be cost-effective, particularly for colorectal cancer screening programs (i.e., finding and removing pre-cancerous polyps early avoids expensive treatment costs) and among geriatric patients with multiple comorbidities [7, 8]. While there has been a published business case for PN [9] with clear case examples for return on investment, sustainment of PN programs remains challenging for many institutions as it is typically a non-revenue-generating service and thus vulnerable to budget cuts when finances are constrained—such as during the recent COVID-19 pandemic when patient volumes plummeted and resources were redirected to address the virus.
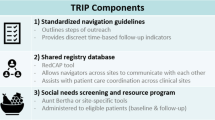
While research on PN effectiveness has grown over the last several decades, few studies have designed or evaluated PN using implementation or sustainability frameworks. Implementation science is a scientific approach to translating research evidence into practice. Two extant studies have explicitly used implementation theory to optimize PN within a particular context: Chicago’s Chinatown study [10] and Boston’s Translating Research Into Practice (TRIP) study [11]. The Chinatown study used the Consolidated Framework for Implementation Research [12] while TRIP referenced implementation principles, but did not cite a particular model. Both studies were collaboratively designed with a community-based coalition to tailor the PN intervention to the specific populations of focus. The Chinatown program emphasized internal leadership, training supports, and strong communication channels. Another study by the Penn Medicine Breast Health Initiative used a quality improvement model to optimize PN and found that securing funding for the program, training navigators and role clarity, community partnerships, culturally-tailored messaging, and evaluation were critical to optimize its program results [13].
The purpose of this study was to examine implementation factors that are related to successful implementation, maintenance, and sustainment of PN programs across diverse cancer care settings. The study focuses primarily on success factors for program implementation and potential sustainability.
Methods
Conceptual framework and epistemology
Drawing from a pragmatic epistemology, we conducted a qualitative study using semi-structured video interviews, guided by the Practical Robust Implementation and Sustainability Model (PRISM) [14]. PRISM is one of few implementation science theoretical models that includes sustainability. The model considers how intervention design, external environment, recipients, and infrastructure affect program adoption, implementation, and maintenance. After examining the data, we supplemented PRISM with the Exploration-Preparation-Implementation-Sustainability (EPIS) framework [15], which includes similar constructs, but also includes phases of implementation from preparation through sustainment.
Researcher characteristics and reflexivity
MPC and PTL are qualitative experts and RS and JT are junior researchers. MPC has a demonstrated track record of published PN workforce capacity research. None of the authors have any direct relationship with research participants.
Setting and subjects
Patient navigators, PN supervisors, and administrators from cancer centers were purposively recruited based on (1) participating in the Centers for Medicare and Medicaid Services (CMS) Oncology Care Model (OCM) or (2) published PN research. Our goal was to recruit seven institutions with three stakeholders from each institution.
Sampling strategy
An attempt was made to recruit one patient navigator, one supervisor, and one administrator from each site to provide varied perspectives on facilitators and barriers that affect program success and sustainability. Up to three recruitment phone calls or emails were sent to each potential participant by a research assistant using a standardized script approved by the PI.
Consent
Participants were sent an information sheet about the study, which was also reviewed verbally prior to each interview. Each participant was asked to verbally consent and to indicate permission to record the interview.
Ethical review
This study was deemed exempt by the George Washington University IRB (#180907).
Data collection
Semi-structured interviews of approximately 60 minutes each were conducted by a trained research assistant between March and July of 2019; digitally recorded via WebEx; and transcribed through Rev.com (San Francisco, CA). An interview guide consisting of ten questions asked about navigator role, reason for program initiation, services provided, organizational fit, engagement of key decision-makers, level of integration into organizational workflow, staffing, program infrastructure, sharing of evaluation data, and future directions. Questions were intended to mine information about the intervention, implementation and sustainability structure, and organizational characteristics based on PRISM [15].
Interviews were conducted until data saturation was reached. Identifiers were removed from transcripts prior to coding. No incentives were provided.
Data analysis
RS and JT conducted line-by-line coding using Dedoose software (dedoose.com) with oversight from PTL and MPC. Data were first deductively coded to capture examples of EPIS constructs [16], and then emergent themes were inductively coded. The study team met weekly over a 3-month period to develop consensus in coding excerpts and refine the codebook. RS and JT reviewed 10% of transcripts and agreed on codes. Subsequently, RS and JT conducted primary coding and drafted memos of key themes from half of the remaining transcripts, respectively. All authors reviewed coding for final agreement and chose exemplar quotations.
Results
Sample characteristics
Of 21 participants invited to participate, 81% (n=17) consented to interview. For one program, a supervisor had recently left, so a physician was interviewed instead. Participants included patient navigators (n=7), navigation supervisors (n=4), administrators (n=5), and physicians (n=2) from seven cancer centers of various sizes across the USA. Regionally, one institution was located in the Northeast, two in the Mid-Atlantic, two in the South, and two in the Midwest. While all centers were located in cities, four centers served larger rural areas while three served primarily urban areas. Regional representation is presented by location of individual interviewees rather than institution or state (Table 1). We successfully recruited three stakeholders each in four institutions, two stakeholders each in two institutions, and one stakeholder from one institution.
Themes
The EPIS framework includes outer and inner context factors, innovation factors, and bridging factors that influence the success of innovations. Themes relevant to EPIS constructs are described below with illustrative quotations for themes provided (Table 2).
Outer context
Outer context factors affected the role and focus of the patient navigator as well as program sustainability and growth in our study. For example, service environment and need for services as demonstrated through patient characteristics or community assessments were factors that shaped the role and focus of PN tasks. External networks and accreditation policies were drivers of growth and sustainability.
Overall, financial support of the OCM, American College of Surgeons’ Commission on Cancer (CoC) accreditation requirements, and internal funding for PN programs were facilitators for program success and sustainability. For programs that were participating in the OCM, payer requirements directly influenced the service environment and incentivized clear navigation protocols for assessment and monitoring. Overall, OCM requirements strongly influenced the stability, focus, and processes for participating programs, since payment relied on meeting quality indicators. External funding through grants, however, shifted the focus away from patient care to reporting and meeting the requirements of the funding source. For example, one program initially was funded by CMS to reduce costs among geriatric patients, but when funding ended, the program shifted to meet OCM requirements in order to sustain PN services. Internally funded navigators (programs funded through operational funds) were more likely to be engaged in ongoing quality and process improvements. In addition, internally funded programs that were centrally structured reported greater efficiency and autonomy to focus on navigation. While not a funder, the CoC PN standard for its accredited programs also drove program initiation and sustainment.
Within EPIS, external partnerships are both outer context and bridging factors. Our data indicated that PN partnerships with community organizations yielded improved adherence to care. Philanthropy was also a noted facilitator to meet patient needs by providing free screenings and transportation, and supporting patients facing significant financial toxicity due to their cancer treatment—such as mortgage payments, utility bills, and car payments.
EPIS constructs of patient advocacy and patient characteristics align with our findings for demand or demonstrated need for services. Determination of need for services varied and included internal assessment, community assessment, desire to increase diversity in clinical trials, and accreditation requirements. Reasons for program initiation varied: For example, a navigation supervisor described how their program was initiated as a result of prior research that explored the challenges of individuals whose primary language was not English. A patient navigator indicated the need for navigation to help patients understand insurance and financial impacts of their cancer treatment: In some cases, patients were declining treatment due to cost.
Some programs were initiated specifically to address the complexities of varying forms or stages of cancer. An administrator at a large center reported that their program started in order to reduce late-stage diagnoses. In each scenario, program initiation was driven by an identified barrier to cancer care adherence.
Inner context
Sustainability factors related to inner context include organizational characteristics, culture, and internal leadership; organizational staffing and processes; individual characteristics; and the ability to show relative advantage of the navigation program through evaluation.
A key facilitator for program success was the importance of aligning program goals with organizational strategic initiatives, leadership priorities, and organizational culture. Internal leadership was noted as a facilitator for program initiation and growth. For example, an administrator reported that a new CEO at the institution encouraged employees to engage in community outreach, and thus, the program aligned with the CEO’s strategic priority. Alignment with disease teams and goals was also a facilitator for success. Program alignment led to greater satisfaction within the navigation team and a sense of being valued.
Strong programs established on-the-job and online training on-boarding processes and appropriate staffing levels. Patient navigators at institutions that did not invest in their professional development suffered. Appropriate levels of staffing with reasonable workloads also surfaced as important. In contrast, staffing inadequacies led to challenges in fitting with clinic workflow. Likewise, lack of staffing slowed efficiency: One navigation supervisor noted challenges with obtaining records for complex cases due to understaffing which led to delays in care.
Data collection among participating sites was essential to show the relative advantage of PN services. Evaluation data were collected in a variety of ways, including Excel, REDCap, Electronic Health Records (EHRs), and a customized app. Data were used to show program impact internally to leadership and supported program growth in alignment with patient needs. Data were used to show productivity, resolution of patient barriers to care, and patient retention that led to indirect revenue. A program with robust evaluation was able to show value in terms of patient retention and services billed. In contrast, a program that did not prioritize data collection reported a lack of institutional support or prioritization of navigation services. This same navigator noted a lack of internal support for program sustainment.
Innovation factors
Prominent innovation factors for sustainability included innovation developers, innovation characteristics, and innovation fit. Innovation developers varied by program, but typically fell to the navigation supervisor who distinguished roles within patient services and championed navigation services. The importance of a dedicated role for program development was a common theme. Programs varied in emphasis on nurse versus non-clinical PN, but clear distinctions between these roles was a success factor. Program stakeholders reported navigation tasks including arranging transportation, facilitating screenings, resolving insurance challenges, finding and connecting patients to community resources, resolving challenges with food insecurity or utility payments, arranging for co-pay or free drug assistance, assessing eligibility for financial assistance, arranging genetic testing, arranging interpretation services, scheduling future appointments, preparing patients for visits with a provider, educating patients about what treatment involves and what services are available, assessing patient self-efficacy to take the steps needed to adhere to treatment, assessing distress, helping patients organize information regarding follow up tests and how the system works, and following up with patients by phone or in person to remind patients of appointments and services available. Additional tasks included obtaining referrals for services, identifying past medical history and services and procedures a patient has received, charting in the medical record, and contacting primary care providers to report back on procedures a patient received or is recommended to receive.
Facilitators for program success included team coordination; collaboration within an appropriate scope of practice; clear protocols; strong communication channels; and innovation fit to context. A Medical Oncologist reported that lack of clear role delineation resulted in role confusion and staff not operating at the top of their license. Clear protocols and scripts aided navigation efficiency and optimized patient care coordination to avoid expensive emergency room visits. Strong communication channels also emerged as an important characteristic for program success. Patient navigator participation in multi-disciplinary team meetings helped foster team communication. Inclusion of patient navigators in team meetings and tumor boards provided them with information to better coordinate care for patients. In contrast, barriers to communication resulted in less efficient care coordination. Thoughtful integration into existing workflows was also a factor for success.
Sustainability
Also a bridging factor, internal collaboration with researchers was noted as a strategy to optimize external funding support, and thus the sustainability of programs. Community-academic partnerships were not prevalent, but some programs voiced aspirations to integrate navigation into more community outreach and research in the future. The benefit of community-academic partnerships, when present, included robust evaluation showing the value of PN—indirectly supporting the sustainability of the intervention.
Funding stability emerged as the most important indicator for sustainability. Diverse funding streams were reported, including grants, operational budgets, and OCM financing.
Navigators with internal funding expressed perceived job security. Conversely, when PN was contingent on grant funding, sustainment was jeopardized and navigators felt devalued.
Discussion
A critical challenge to PN sustainability is lack of financing for services. Historically, PN programs have been supported by grants with a limited duration and short-term outcomes. For example, the National Institutes of Health (NIH), the Centers for Disease Control and Prevention (CDC), the Centers for Medicare and Medicaid Services (CMS), and the Health Resources and Services Administration (HRSA) have funded numerous research studies to support demonstration projects and evaluate the efficacy of PN [17]. The American Cancer Society (ACS), the Avon Safety Net Foundation, and Susan G. Komen have supported PN in practice through grant funding. However, grants from foundations have declined in recent years [18]. Thus reliance on grants is not a long-term sustainability strategy.
Integration of PN into standard of care is required for ongoing sustainment. Value-based payment models are promising options for PN sustainability. For example, the OCM requires institutions to include PN as one of several essential services required for payment [19, 20]. A $160 up-front per patient per episode payment is provided to offset the costs of these services [19]. In other disease areas, limited PN has been paid for under Medicare or Medicaid fee-for-service (FFS) codes [18]. These programs typically focus on patient education regarding diagnosis or self-management of a disease, limiting the flexibility of PN services as well as the patient populations eligible to receive services. The inflexibility of FFS payments, however, makes value-based options more attractive for oncology PN programs. Nevertheless, an FFS option for cancer screening might be quite helpful to improve adherence to guideline-driven screening.
Regardless of the financial source of support, PN programs will only be sustained if leadership within cancer care organizations value PN services. With leadership support, PN can not only be sustained, but grow. For example, Sarah Cannon, the Cancer Institute of HCA Healthcare, has demonstrated increases in patient volumes, less staff turnover, and greater patient satisfaction—leading to increasing support for an ever-growing PN program of services [9]. Their progressive leadership is an exemplar in using evaluation data to support growth.
Finally, the variability of PN programs can make it challenging to draw generalizable conclusions for best practices—in turn, making it difficult to know what exactly should be sustained. Some cancer centers employ nurse navigators and others employ patient navigators without a clinical license. The scope of practice of each of these types of navigators varies. In addition, patient needs might demand different services from navigators. Where PN may be driven by the linguistic needs of some patient populations across the continuum of care, PN may be focused on reducing late-stage diagnoses in screening settings. Some centers employ a team-based approach, triaging patients to the appropriately skilled navigator based on the type of patient need. While common tasks of PNs include providing education to patients, identifying and addressing barriers to care, assisting with scheduling, attending appointments with patients, and providing referrals for services, patient needs across settings vary widely [21].
Our study contributes to the PN literature in several ways. We fill a gap in the literature by using implementation theory to identify factors across settings that aid in implementation success and sustainability. Specifically, this research is the first study to our knowledge to use the EPIS framework to describe PN program success and sustainability. In our study, a number of clear factors to program success and sustainability emerged that align with three of four phases of the EPIS framework. For the Preparation phase of EPIS, demonstrated need for services based on individuals served by the system and leadership support were critical factors. For the Implementation phase, alignment with organizational culture and strategic priorities, provision of training and staff supports, clear role delineation among team members, dedicated program leaders, clear protocols and scripts for navigators, and strong communication channels proved helpful for PN programs. For example, innovation fit was optimized in one center by clearly delineating between PN and social work roles (see Table 2, Innovation fit). Bridging factors such as relationships with community-based organizations further supported successful implementation—for example, reliance on established faith-based networks to drive patients to cancer screening. This finding aligns with a recent review that found partnerships to be essential in the development of community health worker and PN programs [21]. Sustainment was facilitated by ability to show relative advantage through evaluation as well as external incentives such as payer or accreditation requirements. Financing streams varied, but funding stability was the clearest facilitator for program sustainment.
Our study found that noted barriers to PN program success included inconsistent funding, lack of a program champion with authority, ineffective training or lack of professional development for staff, and inadequate staffing and workloads. For example, programs that depended on grant funding were vulnerable to reduced staffing over time. Many grant-funded programs had an abundance of patients and a dearth of navigators. Navigators expressed feeling overwhelmed trying to meet funder requirements. For programs where grant funding ultimately was exhausted, some programs lost staff, ultimately reducing patient support and care coordination efficiency.
It is worth noting explicitly that a fundamental assumption of our study is that strong, successful programs will be more sustainable. In the primary care literature, a recent scoping review of PN programs identified eleven core elements of sustainable navigation programs, all of which align with our qualitative findings regarding successful programs [22]. These include attention to patient characteristics, training of navigators, role clarity, clear operational processes, adequate staffing and resources, strong inter-organizational networks, community partnerships, strong communication channels, demonstrated need for the program (i.e., program uptake and buy in by end users of the program), valuing of navigators, and evaluation (i.e., showing the value of the program). Our study provides additional support for the findings of this scoping review and suggests that these sustainability factors are transferable to PN programs across various clinical areas.
Strengths
As noted above, the use of the EPIS framework specifically, and implementation science theory generally, are strengths of our study. Another strength is the examination of constructs from multiple perspectives—not just that of navigators, but also program supervisors and administrators.
Limitations
This study was limited by a small sample of navigation programs that may have represented more robust programs than are typical due to participation in the OCM and extant publications. Our sampling approach did not allow for comparisons among a similar number of successful and unsuccessful programs. Recruitment of interviewees was also challenging given the lack of incentives.
Future research directions
Future research is warranted to identify specific and parsimonious evaluation metrics critical to PN program sustainability. Additional work to tie evaluation to payer metrics will be critical for sustainability. Additional research is also needed to identify optimal care coordination strategies for navigators in collaboration with clinicians and community-based organizations, including communication and documentation through health information exchanges. Furthermore, research on whether PN increases adherence to treatment by moderating patient financial toxicity is warranted and would be novel. While our study attempted to identify important implementation constructs, more in-depth observational research may be warranted to provide even richer data regarding important variations among PN program settings. Longitudinal observational studies will be important to confirm the preliminary insights on sustainment we found in our study.
Conclusion
PN can be a cost-effective way to address barriers in access to cancer care. We identified several major facilitators for PN sustainability: aligned external incentives, strong leadership, clear roles and protocols, and effective partnerships tailored to patient needs. Additional facilitators were demonstrating a need for the program, clear communication channels, training supports, and funding stability. Without these factors, patient navigators may feel unsupported and undervalued and programs may experience challenges to sustainment.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- CoC:
-
Commission on Cancer
- CMS:
-
Centers for Medicare and Medicaid Services
- EPIS:
-
Exploration Preparation Implementation Sustainment
- OCM:
-
Oncology Care Model
- PRISM:
-
Practical, Robust Implementation and Sustainability Model
References
Community Health Workers 2017. The Community Guide. https://www.thecommunityguide.org/content/community-health-workers. Accessed 5 Oct 2021.
Raich PC, Whitley EM, Thorland W, Valverde P, Fairclough D. Denver Patient Navigation Research Program. Patient navigation improves cancer diagnostic resolution: an individually randomized clinical trial in an underserved population. Cancer Epidemiol Biomarkers Prev. 2012;21(10):1629–38. https://doi.org/10.1158/1055-9965.EPI-12-0513.
Castaldi M, Safadjou S, Elrafei T, McNelis J. A multidisciplinary patient navigation program improves compliance with adjuvant breast cancer therapy in a public hospital. Am J Med Qual. 2017;32(4):406–13. https://doi.org/10.1177/1062860616656250.
Jean-Pierre P, Cheng Y, Wells KJ, Freund KM, Snyder FR, Fiscella K, et al. Satisfaction with cancer care among underserved racial-ethnic minorities and lower-income patients receiving patient navigation. Cancer. 2016;122(7):1060–7. https://doi.org/10.1002/cncr.29902.
Jandorf L, Braschi C, Ernstoff E, Wong CR, Thelemaque L, Winkel G, et al. Culturally targeted patient navigation for increasing african americans’ adherence to screening colonoscopy: a randomized clinical trial. Cancer Epidemiol Biomarkers Prev. 2013;22(9):1577–87. https://doi.org/10.1158/1055-9965.EPI-12-1275.
Freund KM. Implementation of evidence-based patient navigation programs. Acta Oncol. 2017;56(2):123–7. https://doi.org/10.1080/0284186X.2016.1266078.
Gerves-Pinquie C, Girault A, Phillips S, Raskin S, Pratt-Chapman M. Economic evaluation of patient navigation programs in colorectal cancer care, a systematic review. Health Econ Rev. 2018;8(1):12. https://doi.org/10.1186/s13561-018-0196-4.
Rocque GB, Pisu M, Jackson BE, Kvale EA, Demark-Wahnefried W, Martin MY, et al. Resource use and medicare costs during lay navigation for geriatric patients with cancer. JAMA Oncol. 2017;3(6):817–25. https://doi.org/10.1001/jamaoncol.2016.6307.
Kline RM, Rocque GB, Rohan EA, Blackley KA, Cantril CA, Pratt-Chapman ML, et al. Patient navigation in cancer: the business case to support clinical needs. J Oncol Pract. 2019;15(11):585–90. https://doi.org/10.1200/JOP.19.00230.
Simon MA, Tom LS, Leung I, Wong E, Knightly EE, Vicencio DP, et al. The Chinatown patient navigation program: adaptation and implementation of breast and cervical cancer patient navigation in Chicago's Chinatown. Health Serv Insights. 2019;12:1178632919841376. https://doi.org/10.1177/1178632919841376.
Battaglia TA, Freund KM, Haas JS, Casanova N, Bak S, Cabral H, et al. Translating research into practice: protocol for a community-engaged, stepped wedge randomized trial to reduce disparities in breast cancer treatment through a regional patient navigation collaborative. Contemp Clin Trials. 2020;93:106007. https://doi.org/10.1016/j.cct.2020.106007.
Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci. 2009;4:50. https://doi.org/10.1186/1748-5908-4-50.
Guerra CE, Verderame E, Nicholson A, Wan L, Brooks AD. A Plan-Do-Study-Act approach to the development, implementation and evaluation of a patient navigation program to reduce breast cancer screening disparities in un- and under-insured, racially and ethnically diverse urban women. Front Public Health. 2021;9:595786. https://doi.org/10.3389/fpubh.2021.595786.
Feldstein AC, Glasgow RE. A practical, robust implementation and sustainability model (PRISM) for integrating research findings into practice. Jt Comm J Qual Patient Saf. 2008;34(4):228–43. https://doi.org/10.1016/s1553-7250(08)34030-6.
Moullin JC, Dickson KS, Stadnick NA, Rabin B, Aarons GA. Systematic review of the Exploration, Preparation, Implementation, Sustainment (EPIS) framework. Implement Sci. 2019;14(1):1. https://doi.org/10.1186/s13012-018-0842-6.
Aarons GA, Hurlburt M, Horwitz SM. Advancing a conceptual model of evidence-based practice implementation in public service sectors. Adm Policy Ment Health. 2011;38(1):4–23. https://doi.org/10.1007/s10488-010-0327-7.
Freeman HP. The origin, evolution, and principles of patient navigation. Cancer Epidemiol Biomarkers Prev. 2012;21(10):1614–7. https://doi.org/10.1158/1055-9965.EPI-12-0982.
Osundina F, Garfield K, Downer S. National Navigation Roundtable. Patient Navigation in Cancer Care: American Cancer Society; 2019. https://www.chlpi.org/wp-content/uploads/2013/12/Patient-Navigation-in-Cancer-Care-Review-of-Payment-Models_FINAL.pdf. Accessed 5 Oct 2021.
Kline RM, Bazell C, Smith E, Schumacher H, Rajkumar R, Conway PH. Centers for medicare and medicaid services: using an episode-based payment model to improve oncology care. J Oncol Pract. 2015;11(2):114–6. https://doi.org/10.1200/JOP.2014.002337.
Kline RM, Muldoon LD, Schumacher HK, Strawbridge LM, York AW, Mortimer LK, et al. Design challenges of an episode-based payment model in oncology: the Centers for Medicare & Medicaid services oncology care model. J Oncol Pract. 2017;13(7):e632–e45. https://doi.org/10.1200/JOP.2016.015834.
Roland KB, Milliken EL, Rohan EA, DeGroff A, White S, Melillo S, et al. Use of community health workers and patient navigators to improve cancer outcomes among patients served by federally qualified health centers: a systematic literature review. Health Equity. 2017;1(1):61–76. https://doi.org/10.1089/heq.2017.0001.
Valaitis RK, Carter N, Lam A, Nicholl J, Feather J, Cleghorn L. Implementation and maintenance of patient navigation programs linking primary care with community-based health and social services: a scoping literature review. BMC Health Serv Res. 2017;17(1):116. https://doi.org/10.1186/s12913-017-2046-1.
Acknowledgements
The authors would like to thank Julianne Lee who completed data collection for the study and Ruta Brazinskaite who assisted with reference formatting.
Funding
N/A.
Author information
Authors and Affiliations
Contributions
MPC conceptualized and designed the study, defined the initial codebook, and led manuscript writing. RS and JT conducted independent coding and contributed to writing the manuscript. PTL supervised coding and contributed to manuscript writing. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was deemed exempt under DHHS regulatory category 2 by the George Washington University IRB (#180907).
Consent for publication
N/A.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Pratt-Chapman, M.L., Silber, R., Tang, J. et al. Implementation factors for patient navigation program success: a qualitative study. Implement Sci Commun 2, 141 (2021). https://doi.org/10.1186/s43058-021-00248-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43058-021-00248-0