Abstract
Background
This work was conducted to assess the diagnostic efficiency of isotropic three-dimensional VISTA-fast spin echo versus standard two-dimensional fast spin echo at 1.5 T MRI, in the assessment of internal knee derangement in symptomatic patients, aiming to obtain similar diagnostic accuracy in a shorter time span, with reduction of partial volume artifacts by thin continuous sections.
Results
This was a non-randomized control study including 39 patients (32 male and 7 females, mean age 37 years old). A correlative study was done utilizing MRI standard 2D FSE (protocol A) versus 3D-VISTA-FSE (protocol B) for medial meniscus (MM) and lateral meniscus (LM), as well as anterior cruciate ligament ACL lesions, comparing the MRI results with the findings of arthroscopy as the gold standard. Both protocols depicted medial meniscus lesions with accuracy, specificity, and sensitivity (97.44%, 96.30%, and 100% respectively), lateral meniscus lesions with accuracy, specificity, and sensitivity (97.44%, 100%, and 50% respectively), and ACL lesions with accuracy, specificity, and sensitivity (100%, 100%, and 100% respectively), while there were no PCL lesions depicted through the study population. Comparing the time factor between both protocols revealed protocol A to consume 13.7 min, while protocol B consumed 6.6 min.
Conclusion
Three-dimensional isotropic VISTA-FSE sequence, although having similar accuracy in diagnosing cruciate and meniscal lesions as the standard sequences, facilitates thin-section data acquisition and multi-planar image reformation in standard and non-standard planes, without intersection gaps that are crucial for the detection and dissection of compound structures; also, it allows a shorter time span, which is more advantageous for patients, particularly the traumatized and emergency patients.
Similar content being viewed by others
SD Standard deviation
MPR Multi-planar reformation
IW Intermediate weighted
SPSS Statistical Package for the Social Science
Lt Left
Rt Right
PHMM Posterior horn medial meniscus
PHLM Posterior horn lateral meniscus
Background
Magnetic resonance imaging (MRI) is a specific, detailed, and noninvasive method that is used to assess internal derangements of the knee [1].
The regular MRI technique for evaluation of internal derangements of the knee utilizes two-dimensional (2D) fast spin echo (FSE) sequence, because of its higher contrast and signal-to-noise ratio. This sequence is satisfactory in evaluating joint abnormalities such as ligamentous injuries, fibro-cartilage damage, and meniscal tears [2].
Current standard 2D MR imaging has several limitations, such as (a) rather thick image sections, associated with gaps in-between, which can obscure fine anatomical details due to partial volume artifacts; (b) non-isotropic voxels; and (c) they are almost repeated in multiple planes when used to evaluate the knee joint, as reconstructions are not possible, thus extending examination time [3].
Isotropic 3D MR images can be performed with a size of 0.5 × 0.5 × 0.5 mm voxels. This can minimize the partial volume artifacts seen with conventional 2D MR images [4]. Multi-planar reformatting can be applied in all necessary planes, including the standard orthogonal planes, within only a few seconds. Hence, it can be helpful for the detection and diagnosis of complex or abnormally positioned internal structures of the knee. This imaging sequence have better diagnostic performance in detecting small radial and root tears of the menisci than conventional 2D images [5]. This was presumably due to a smaller interslice gap and the ability to reconstruct images along the structures of concern [2].
MRI of the knee is known to have high sensitivity and specificity for the detection of ACL ligament and meniscal tears. The 3D VISTA sequence can afford high-resolution volumetric images. Acquisition time and inter-echo spacing are optimized by applying reduced flip angles in conjunction with non-selective refocusing pulses. Combining parallel acquisitions utilizing robust factors in both directions of the encoding phase establishes faster acquisition times [2].
The purpose of this study was to demonstrate the added value, diagnostic accuracy, and superiority of isotropic three-dimensional (3D) fast spin echo over standard two-dimensional (2D) fast spin echo at 1.5 T MR sequences in the interpretation of meniscal and cruciate ligament lesions in symptomatic patients.
Methods
Patients
We designed a non-randomized control study for patients clinically presenting with persistent chronic knee pain or post traumatic status, who were referred from the orthopedic outpatient clinic to the Radiology Department, during the time period February 2017 to February 2018. The study included 39 patients (32 male and 7 females), which age ranged from 15–60 years (mean age 37 years). All patients included in the study had MRI examination, including both protocols (A and B), followed by arthroscopy as the gold standard reference. A correlative study was conducted between the MRI results and arthroscopic findings. Patients who were excluded from the study include those who had previous surgery on the same knee, when the interval between MRI study and arthroscopy exceeded 21 days, patients with poor image quality due to any type of artifact, those with acute knee fracture, and patients with isolated degenerative meniscal or cruciate ligament lesions, as they were not candidate for arthroscopy (gold standard). Written informed consents were collected from all patients.
MR protocol
MRI examinations were done on “ACHIEVA 1.5 T equipment (from PHILIPS Medical Systems, Best, the Netherlands)” utilizing a phased array knee coil. The candidate lied supine with joint space in the middle of the coil, while the knee joint was maintained in extension with slight flexion.
The standard knee protocol (coronal T1, axial T2, and sagittal proton density) was designated protocol A, while the 3D PD-FS (FSE) imaging was designated protocol B (Table 1).
Imaging analysis and interpretation
The produced MR images were transferred to a workstation using the Digital Imaging and Communications in Medicine (DICOM) format. Two musculoskeletal radiologists, each with an experience in interpretation of knee MR images more than 10 years, individually studied the two sets of MR protocols, each one blinded from the other, and from the arthroscopic findings, the 3D images were generated concurrently during image revision by the use of PACS software, and then they correlated their results with each other and with the results of arthroscopy. For each examined joint, the following were assessed and reported in both protocols (A and B).
The anterior ligament
ACL was assessed either by the presence or absence of tears (partial or complete). The diagnostic findings of cruciate ligament tear were an abnormal course, increased signal intensity or discontinuity, and indistinct margins with or without abnormal signal [6].
The menisci
The medial and lateral menisci were assessed (body, anterior and posterior horns). The criteria for meniscal tear were increased signal intensity within the meniscus reaching the meniscal articular surfaces or abnormal meniscus morphology [6].
Reformation of the isotropic 3D MR images and image analysis were performed simultaneously with picture archiving and communication system software. Reformatted images with 0.05 cm section thickness in axial and coronal planes were formed semi-automatically.
Arthroscopic interpretation
Arthroscopies were done by specialized orthopedic surgeons, with experience in knee joint intervention more than 10 years. Arthroscopies were done within average time interval of 14 ± 7 days to the MR studies. At arthroscopy, each cruciate ligament was classified as being normal or having partial or full thickness tear. Signs of existing tear include decreased tension on probing, grossly or focally disrupted bundle. Each meniscus was classified as either intact or torn, a visible fissure extending through the meniscal substance, or just surface fraying, which were all signs of meniscal pathology.
Statistical studies
Obtained data were statistically analyzed in the form of range, mean, standard deviation (± SD), frequencies (number of cases), and percentages.
Categorical data comparison was done by using chi-square test. Exact test was used instead when the expected frequency is less than 5. Agreement between 2D and 3D findings was obtained using kappa statistic.
Accuracy was represented by the terms of sensitivity, specificity, positive (+ve) predictive value, negative (−ve) predictive value, and overall accuracy. All calculations were performed by computer programs Microsoft Excel 2003 (Microsoft Corporation, USA) and SPSS (Statistical Package for the Social Science; SPSS Inc., Chicago, USA) version 15 for Microsoft Windows.
Screening test done using MedCalc version 18.9. Fisher exact correction was done for comparison of qualitative variables.
The standard of reference
Knee arthroscopy was considered the gold standard technique.
Results
Diagnostic performance of both protocols
Comparative study was performed between MRI protocol A versus protocol B for different meniscal and cruciate ligament lesions, and then compared with arthroscopic findings (Table 2).
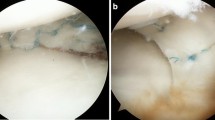
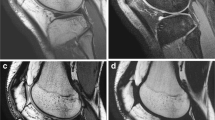
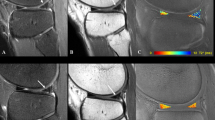
Meniscal lesions (Figs. 1, 2, 3, 4, and 5) (Tables 3, 4, 5, and 6)
Both MRI protocols detected medial meniscus injury in 13 knee joints while arthroscopy detected it in 12 knee joints; both modalities agreed in 12 patients, establishing a sensitivity = 100%, specificity = 96.30%, positive predictive value = 92.31%, negative predictive value = 100%, and accuracy = 97.44%.
A 32-year-old male patient presented with acute LT knee joint pain after trauma. a, b Sagittal standard 2D PDWI and 3D MPR VISTA images show horizontally oriented tear of the medial meniscus posterior horn (PHMM) (white arrows) with small related parameniscal cyst, with the tear clearly outlined in the VISTA images. c, d Coronal standard 2D PD and 3D MPR VISTA images again show the horizontal tear of the PHMM (white arrows)
A 29-year-old male patient presented by acute RT knee joint pain after trauma. a, b Sagittal Standard 2D PDWI and 3D MPR VISTA images show complex branching tear in PHLM (white arrows). c, d Coronal standard 2D PD and 3D MPR VISTA images again show complex branching tear in PHLM (long white arrows), clearly outlined in the VISTA images
A 35-year-old male patient presented by acute left knee pain after trauma. a, b Sagittal standard 2D PD WI and c coronal standard 2D PD WI, showing bucket handle tear at the PHMM, arrowed at a and c, with flipped meniscal fragment anteriorly posterior to the anterior horn, arrowed at b. d–g 3D MPR VISTA images (sagittal, coronal, and axial), showing the flipped triangular meniscal fragment, arrowed at d and f and the bucket handle tear arrowed at e and g
A 30-year-old female patient presented by right knee pain with history of trauma. a, b Coronal standard 2D PD WI and sagittal T2 standard 2D images, showing medial meniscus posterior root full thickness radial tear, white straight arrows. c–e 3D MPR VISTA images (coronal, sagittal, and axial), clearly outlining the posterior root full thickness radial tear, white straight arrows
Both protocols detected LM injury in 1 knee joint while arthroscopy detected it in 2 knee joints; both modalities agreed in 1 patient only and one lesion missed by MRI, reaching a sensitivity = 50%, specificity = 100%, positive predictive value = 100%, negative predictive value = 97.37%, and accuracy = 97.44%.
Cruciate lesions (Fig. 6) (Tables 7 and 8)
Both protocols detected ACL injury in 21 knee joints which agreed with arthroscopy, having a sensitivity = 100%, specificity = 100%, positive predictive value = 100%, negative predictive value = 100%, and accuracy = 100%.
There were no patients with PCL lesions either by MRI or arthroscopy.
Comparative statistical analysis
Comparing 2D MRI versus 3D MRI was done to reach accurate diagnosis by correlating the findings of each modality with the findings of arthroscopy (Figs. 7, 8 and 9).
Discussion
The main idea of Isotropic 3D MRI study is that its images can be obtained with size of 0.5 × 0.5 × 0.5 mm voxels. This range of acquisition reduces the partial volume artifacts seen at conventional 2D MR images. Multi-planar reformation (MPR) may be performed in all the essential planes, including standard orthogonal planes only in a few seconds. Therefore, this technique can be helpful for the diagnosis of complex and non-orthogonally oriented internal structures of the knee [2].
Lim et al. stated that 3D isotropic MR images accompanied by reconstructed MPR images achieve diagnostic accuracy in detection of small meniscal complex, radial, and root tears better than conventional 2D images [5]. This was likely due to small inter-slice gap as well as the capacity to reconstruct images along the important structures.
Knee MRI images have been reported as having high sensitivity and specificity for cruciate ligament lesions and meniscal tears diagnosis. Currently, most of the studies have revealed that isotropic 3D imaging technique has a diagnostic accuracy that is almost identical to the conventional 2D images [2, 5]. The 3D VISTA sequence produces high-resolution volumetric intermediate-weighted (IW) images. Inter-echo spacing and acquisition time are enhanced by utilizing reduced flip angles in combination with non-selective refocusing pulses [7].
Jung et al. compared isotropic 3D FSE and conventional 2D FSE without valid differences in diagnostic accuracy in the assessment of menisci and ligament lesions [7]. This was concordant with our results, as we also did not reach any significant difference in diagnostic accuracy for the assessment of ACL and PCL lesions and both menisci tears.
In our study, the results of both protocols, compared with arthroscopy, showed sensitivity, specificity, and accuracy of 100%, 100%, and 100%, respectively, for the diagnosis of anterior cruciate ligament tears; 100%, 96%, and 97.44%, respectively, for the detection of MM tears; and 50%, 100%, 97%, respectively, for LM tears.
In a previous study, “Duc et al.” agreed with us and demonstrated that their 3D sequence had similar sensitivity, specificity, and accuracy compared with conventional 2D imaging study and reported 3D fast imaging sensitivity, specificity, and accuracy of 80%, 95%, and 90%, respectively, for the assessment of anterior cruciate ligament tears; 100%, 82%, and 90%, respectively, for the assessment of medial meniscus tears; and 83%, 83%, and 83%, respectively, for lateral meniscus tears [5].
A large study by “Kijowski” was in accordance with us and stated that 3D sequence had a comparable sensitivity (90%) and specificity (100%) for assessment MM tears compared with standard MRI sequences [3].
In another study, “Li et al.” agreed with us and demonstrated that at 1.5 T machine, a 3D-FSE sequence had similar diagnostic accuracy in the assessment of meniscal and cruciate ligament tears in comparison with routine 2D sequences in the orthogonal planes with accuracy 90% for MM and LM tears and 95% for ACL and PCL, but this research work was limited because the standard knee protocol was used as the reference gold standard, not arthroscopy [8]. Our study used arthroscopy as gold standard reference with net results of accuracy 97.44% for menisci and 100% for cruciate ligaments. Also, their study did not evaluate the time factor between the two protocols, and our study demonstrated that protocol A consumed 13.7 min., while protocol B consumed 6.6 min.
It had been documented that LM tears are more likely to be missed in conventional 2D MR images because of the LM anatomical complexity, especially if the tear affects only one third of the meniscus or found in the posterior horn [2]. Although the FS 3D VISTA sequence has isotropic voxels and smaller inter-slice gap, it did not have a better diagnostic accuracy in LM evaluation. This was in agreement with our results, as both protocols missed one case with LM tear, which was detected at arthroscopy.
The MPR images were automatically achieved in a few seconds focusing on abnormal lesions with reduced partial volume and summation artifacts and consequently increasing diagnostic accuracy. The shorter acquisition time renders the study more comfortable for the patient, which might reduce motion artifacts and improve the image quality as a concomitant effect.
Limitations
First, we had a relatively small sample (39 subjects). Second, patient choice bias may have been erroneously made because we studied only those patients who had arthroscopic surgery. Also, another limitation is that our patient sample did not include other ligamentous injuries, like collateral ligament injury; at the same setting, cartilage and bone marrow lesions were not investigated in the current study. Finally, based upon the results of our study, we cannot simply recommend that radiologists substitute the standard 2D FSE technique with the 3D FSE protocol for knee evaluation, because our study was confined to the menisci and cruciate ligament lesions.
Conclusion
In conclusion, our results showed that FS 3D VISTA has a diagnostic potential for the evaluation of meniscal and cruciate ligament lesions at 1.5 T MRI machine. The ability for time saving, with diagnostic accuracy similar to conventional 2D sequence, is important in clinical practice to achieve patient comfort.
The described 3D isotropic MR sequence produces thin-section data without inter-slice gaps and multi-planar reformatted images in orthogonal planes that are essential for the detection of complex lesions.
Availability of data and materials
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- VISTA:
-
Volume isotropic turbo spin-echo acquisition
- MRI:
-
Magnetic resonance imaging
- MM:
-
Medial meniscus
- LM:
-
Lateral meniscus
- ACL:
-
Anterior cruciate ligament
- PCL:
-
Posterior cruciate ligament
- PD:
-
Proton density
- FSE :
-
Fast spin echo
- SE:
-
Spin echo
- 2D:
-
Two dimensional
- 3D:
-
Three dimensional
- FS:
-
Fat suppression
- DICOM:
-
Digital imaging and communication in medicine
References
Kijowski R, Davis KW, Blankenbaker DG, Woods MA, Del Rio AM, De Smet AA (2012) Evaluation of the menisci of the knee joint using three-dimensional isotropic resolution fast spin-echo imaging: diagnostic performance in 250 patients with surgical correlation. Skeletal Radiol 2012 41(2):169–178
Lim D, Lee YH, Kim S, Song H-T, Suh J-S (2016) Clinical value of fat-suppressed 3D volume isotropic spin-echo (VISTA) sequence compared to 2D sequence in evaluating internal structures of the knee. Acta Radiologica 57(1):66–73
Kijowski R, Blankenbaker DG, Woods M, Del Rio AM, De Smet AA, Reeder SB (2011) Clinical usefulness of adding 3D cartilage imaging sequences to a routine knee MR protocol. AJR Am J Roentgenol 196(1):159–167
Yao L, Pitts JT, Thomasson D (2007) Isotropic 3D fast spin-echo with proton-density-like contrast: a comprehensive approach to musculoskeletal MRI. Am J Roentgenol 188:W199–W201
Lim D, Lee YH, Kim S et al (2013) Fat-suppressed volume isotropic turbo spin echo acquisition (VISTA) MR imaging in evaluating radial and root tears of the meniscus: focusing on reader-defined axial reconstruction. Eur J Radiol 82:2296–2302
Lee JH, Yoon YC, Park KJ, Wang JH (2017) Diagnosis of internal derangement of the knee: volume isotropic turbo spin-echo acquisition MRI with fat suppression versus without fat suppression. Am J Roentgenol 208:1304–1311. https://doi.org/10.2214/AJR.16.17217
Jung JY, Yoon YC, Kim HR et al (2013) Knee derangements: comparison of isotropic 3D fast spin-echo, isotropic 3D balanced fast field-echo, and conventional 2D fast spin-echo MR imaging. Radiology 268:802–813
Li CQ, Chen W, Rosenberg JK, Beatty PJ, Kijowski R, Hargreaves BA et al (2014) Optimizing isotropic three-dimensional fast spin-echo methods for imaging the knee. J Magn Reson Imaging 39(6):1417–1425
Acknowledgements
The authors gratefully acknowledge the valuable contributions of Dr. Sherihan Salah, resident of radiology, in facilitating and performing this work.
The authors are really appreciating the role of the Kasr Al-Aini Institute and Hospital for providing the study with the required type of patients and the help of reaching optimum diagnose for the proper management service.
Funding
None to declare
Author information
Authors and Affiliations
Contributions
NE conceived the study, designed it, was the primary radiologist who interpreted the images blindly from the second radiologist, and drafted the manuscript. HK participated in the design of the study and revised and adjusted the manuscript. AS was the orthopedic surgeon who made all the arthroscopies and revised the orthopedic part of the manuscript. All authors have read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study had been approved by the Research Ethics Committee of the Faculty of Medicine at Cairo University in Egypt on 201572016, in compliance with Helsinki Declaration (DoH-oct20081).
All patients included in this study gave written informed consent to participate in this research. If the patient was less than 16 years old or unconscious at the time of the study, written informed consent for their participation was given by their parent or legal guardian.
Consent for publication
All patients included in this research gave written informed consent to publish the data contained within this study. If the patient was less than 16 years old, deceased, or unconscious when consent for publication was requested, written informed consent for the publication of this data was given by their parent or legal guardian.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
El-Liethy, N.E., Rashwan, A.S. & Kamal, H. Single isotropic 3D fast spin echo sequence compared with conventional 2D sequences for detecting meniscal and cruciate ligament tears in the knee. Egypt J Radiol Nucl Med 51, 258 (2020). https://doi.org/10.1186/s43055-020-00362-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43055-020-00362-4