Abstract
Background
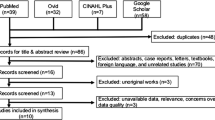
The diagnostic approach for patients with laryngeal lesions differs among otolaryngologists. Indirect laryngoscopy, flexible fibrooptic laryngoscopy, CT, and MRI are all modalities used for diagnosis. Ultrasonography is noninvasive, non-irradiating, and safe. The availability, affordability, and usability of portable ultrasound units have undergone dramatic improvements. It is well tolerated by patients, dynamic technique that can be performed easily in phonation, quickly performed, and allows for photo-documentation. Our objective is to evaluate the laryngeal ultrasound as a diagnostic tool to evaluate different laryngeal structure as regard laryngeal dynamics (range and abnormality), and anatomic structures. This prospective study was carried out on individuals in “blinded for peer review” hospitals. They were divided into group I (healthy volunteers), group II (unilateral vocal fold paralysis), and group III (patients underwent vertical hemilaryngectomies). All patients were subjected to full history taking, detailed head and neck examination, and fibrooptic nasopharyngolaryngoscopy then all patients underwent laryngeal sonographic examination. The photos were analyzed to identify various laryngeal structures and to measure glottic areas and inter-arytenoid distances.
Results
After recognition of laryngeal anatomic details and different measurements, we found that the percent of change in length and area were much less in group III than group I or II. Another important finding is that glottic area during respiration is related significantly to interarytenoid length during respiration with a statistically significant regression coefficient.
Conclusion
Laryngeal ultrasound is a valid diagnostic tool for imaging laryngeal structures and measuring various distances and areas inside the larynx. It is recommended to consider ultrasonography as a reliable imaging modality, and at least a useful adjunct to endoscopy when identification of airway patency, vocal fold mobility, or structural alterations is suspected. To our best knowledge, this study may contain a hitherto undescribed correlation between inter-arytenoid length and glottic area.
Similar content being viewed by others
Background
Otolaryngologists use different diagnostic approaches in evaluation of patients with laryngeal lesion, and no definite clear consensus have been approached as regard the sequence of work up for those patients. Yet complete detailed history with through physical examination usually revealed the etiology of the diagnosis in most of the patients.
A wide variety of techniques to assess laryngeal function are available. These techniques can generally be divided into clinical and investigational categories. A practical technique optimally should be safe, non-invasive, well-tolerated, and reliable. The results should be reproducible, accurate, and recordable for future reference [1].
CT and MRI are valuable diagnostic tools for true and false vocal folds pathology yet with concern of radiation exposure in CT. With MRI, imaging times are relatively long, and respiratory, swallowing, and other motion artifacts can degrade image quality [2].
Using rigid laryngoscope may lead to over- and under-diagnosis of vocal fold paralysis due to the fact of splinting of the larynx, poor visualization due to supraglottic collapse, and fixation of cricoarytenoid and paradoxical movements of vocal fold resulting from the respiratory glottic air flow (Bernoulli effect) [3].
Ultrasonography is routinely done for patient with head and neck tumors to detect cervical lymph nodal metastases, although recent studies shows promising results as regard the use of US technology for diagnosis and staging laryngeal neoplasm yet so far it is not routinely used. Ultrasound is superior to CT and MRI in evaluation of vocal cord motility [4].
It was considered that laryngoscopy was the golden standard test of vocal fold mobility, recurrent laryngeal nerve injury, anatomical and functional variation after, and/or before cervical or thoracic surgery. Yet it imposes extra costs (financial burden), time-consuming, and is an unpleasant experience for most patients [5].
Ultrasonography is a cost-effective, safe, rapid, painless, widely available, well-tolerated, not requiring sedation, non-invasive, and non-irradiating technique with accuracy comparable to that of laryngoscopy; it can be used as a useful adjunct to endoscopy—the current gold standard—especially in children [3].
Portable ultrasound devices are now more available, affordable, and of high diagnostic value due to the dramatic technology improvement. These advances now offer otolaryngologists a portable tool that increases diagnostic accuracy, facilitates commonly performed procedures, and adds to patient convenience and safety. Given the knowledge of head and neck anatomy that otolaryngologists possess, adding ultrasound to an otolaryngology practice is becoming so much easier and making much more sense [6].
The aim of this work is to evaluate the laryngeal ultrasound as a diagnostic tool to evaluate different laryngeal structure as regard laryngeal dynamics (range and abnormality), and anatomic structures.
Methods
This prospective study was carried out on individuals, attending hospital [blinded for peer review] between October 2018 and November 2019. Patients were divided into three groups. The first group included healthy volunteers with no definite signs or symptoms of vocal fold paralysis or any history laryngeal surgeries or pathologies. The second group included patients with unilateral vocal fold paralysis. Their ages ranged from 21 to 50 years. The third group included patients that underwent vertical hemilaryngectomies. They were all males except one female. Their ages ranged from 49 to 72 years.
Inclusion criteria are as follows:
-
1.
Patients with unilateral adductor paralysis
-
2.
Patients that underwent vertical hemilaryngectomy, with no evidence of recurrence of malignancy
Exclusion criteria are as follows:
-
1.
Any patient with bilateral vocal fold paralysis
-
2.
Any patient with abductor paralysis
-
3.
Any patient underwent any medialization surgery to the vocal folds
All included patients were subjected to the following after taking their written consent:
➲ Full clinical history taking
➲ Thorough clinical head and neck examination
➲ Fiberoptic nasopharyngolaryngoscopic examination
➲ Ultrasound examination
The sonographic examination was done as detailed as possible and all patients are asked to lie supine with exposed neck and upper chest and extended neck. The examination was done using ultrasound devise (Logiq P5) high frequency 7–12 MHz linear probe. The examined structures including the larynx and surrounding structures are scanned in at least two perpendicular planes with respect to its anatomical orientation (longitudinal, transverse +/− oblique).
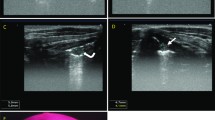
The technique of laryngeal ultrasound involved systematic identification of specific structures in the following order: hyoid bone, laryngeal cartilages, vocal folds, pre-epiglottic space, para-glottic space, epiglottis, thyroid gland, subglottic region, neck vessels, and neck nodes (Figs. 1 and 2).
Subjects were directed to perform various laryngeal maneuvers to determine the range of laryngeal mobility and dimensions, including phonation, inhalation, Valsalva maneuver, swallowing, and coughing. The real-time ultrasonic video clips were retrieved from the device and processed to take snap shots via the so-called Adobe After Effects CS6 (11.0.2) program (Fig. 3 and 4).
An ultrasound photo assessing vocal cord mobility in a patient with VC paralysis (abducted type) by drawing imaginary perpendicular line from the junction between both thyroid cartilage anteriorly where distance 3 (0.14 mm) and 4 (0.38) represent contribution of the right VC in respiratory chink in both respiration and phonation. Where distance 5 (0.33 mm) and 6 (0.38 mm) represent contribution of the right VC in respiratory chink in both respiration and phonation
An ultrasound photo assessing vocal cord mobility in a patient with VC paralysis (adducted type) by drawing imaginary perpendicular line from the junction between both thyroid cartilage anteriorly where distance 2 (0.43 mm) and 5 (0.29) represent contribution of the right VC in respiratory chink in both respiration and phonation. Where distance 3 (0.21 mm) and 6 (0.21 mm) represent contribution of the right VC in respiratory chink in both respiration and phonation
The photos were analyzed to measure glottic areas and inter-arytenoid distances using an image processing program (ImageJ version 1.45s). The inter-arytenoid distance was measured by this program by drawing a line between the hyperechoic arytenoid cartilages, which can be seen in the transverse midline view at the superior thyroid notch with oblique caudal orientation.
While the glottic area was measured by this program by drawing a triangle between three points: the first anterior point at the meeting of the inner plates of thyroid laminae moving along the true vocal folds which look as couple of hypoechoic triangular shadows being medially outlined by hyperechoic vocal ligaments then going posteriorly to the hyperechoic arytenoid cartilages.
Results
Using ultrasound, we managed to identify different laryngeal structures by analysis of the photos using the image processing program called ImageJ version 1.45s.
After analysis of images using ImageJ program, we managed to calculate inter-arytenoid distance during phonation (glottic gap or length min) and during respiration (respiratory chink or length max.). We also managed to measure the glottic area during phonation (area min.), and during respiration (area max.).
The results showed that the length min. (glottic gap) was 0.55 ± 0.32 cm, with minimum of 0.2 cm, and maximum of 1.3 cm. The length max (respiratory chink) showed to be 0.93 ± 0.29 cm, with minimum of 0.43 cm and maximum of 1.5 cm. On measuring the glottic area, we found that area min. showed to be 0.57 ± 0.35 cm2 with a minimum of 0.15 cm2 and a maximum of 1.5 cm2. The area max. showed to be 0.98 ± 0.42 cm2, with a minimum of 0.4 and a maximum of 2.2 cm2 (Table 1).
We found the inter-arytenoid distances during phonation (length min.) to be highest in partially laryngectomized patients 0.81 ± 0.37 cm with statistically significant difference than control group.
On the contrary, the percent of change in length and area were much less in group 3 (partially laryngectomized) than group 1 or 2 (Fig. 5).
Another finding after data analysis is that the age is significantly correlated with the length min., i.e., the more the age, the less the length min. (r = 0.494), and the area min (r = 0.492) (Table 2).
A rather interesting finding after data analysis is that we found that change of area during respiration and during phonation was higher among females 53.07 ± 29.25 cm2 than among males 32.25 ± 20.47 cm2 (Fig. 6).
A strong correlation was found between area minimum (minimum glottic area during expiration) and length minimum (glottic gap) which states that: to calculate area min., we can substitute in the following equation: Table 3
A similar strong correlation was found between area maximum (maximum glottic area during inspiration) and length maximum (respiratory chink) which states that: to calculate area max., we can substitute in the following equation: Table 4
Discussion
Thanks to the great nineteenth century voice teacher Manuel Garcia (1805–1906) who was the first to perform laryngoscope in vivo. Since then, the basic approach of examining the pharynx and larynx has changed little, although the technology available has improved dramatically [7].
As a technique, indirect mirror examination has some limitations including perceptual difficulties in reliably recording side of lesion, learning curve in acquiring and maintaining skills, and a significant failure rate which prior to the era of readily available flexible endoscopy often mandated direct endoscopy under general anesthesia [8].
Endoscopic assessment, either with a rigid or flexible laryngoscope, has replaced mirrors due to better optical resolution and higher sensitivity. With the advance in technology, video techniques have been involved in most of the endoscopic procedures with a lot of advantages including record ability, magnification power which render better identification of anatomical structures with easy diagnosis of any anomaly or abnormality [8].
Though no significant discussion of complications of flexible nasoendoscopy, the most commonly used diagnostic tool in laryngeal lesions exists in the literature, but these possible complications may include discomfort of variable degrees, occasional epistaxis during difficult insertion, fiberoptic laryngoscopy also lacks the ability to show other important causes of laryngeal lesions such as thyroid diseases or lymph nodes enlargement. Also, fiberoptic laryngoscopy lacks any ability to show hidden laryngeal spaces as pre-epiglottic and para-glottic spaces [9].
CT and MRI are known to play an important role in the diagnosis of head and neck diseases. We know that CT and MRI features of suggesting the paralysis of the recurrent laryngeal nerve as atrophy of thyroarytenoid muscle, an enlarged ventricle ipsilateral enlargement of the pyriform sinus, paramedian position, decreased size, and/or fatty infiltration of the true vocal cord [2].
Unfortunately, CT and MRI cannot reveal the mobility of the vocal folds in real time. In addition to artifact caused by respiration and motion with decreased image quality, especially the need for sedation in children is also considered drawback. CT has the potential to deliver significantly greater radiation doses to children than to adults and in view of their greater susceptibility to radiation effects, care should be taken to avoid unnecessary CT examinations [10].
The disadvantages of MRI include the long acquisition time of the scans with consequent degradation of the images due to motion artifact from breathing, swallowing, and vascular pulsations. Claustrophobia and the contraindications due to the use of a strong magnetic field including the presence of cochlear implants, cardiac pacemakers, aneurysm clips, and any metal within the eye are also a problem [10].
In 1984, Shawker and others used real-time ultrasound during swallowing in ten normal subjects and found that the motions of the tongue, hyoid bone, and larynx can be monitored and timed [11].
The ultrasound appearance of the laryngeal region is always a clinical challenge, so the deep knowledge of the complex of the head and neck was essential. A good knowledge of the normal radiological anatomy of the head and neck renders easy identification of any abnormality.
Recently, US imaging has become a very powerful diagnostic tool, especially in scanning head and neck regions. With the advance in technology of ultrasound, it renders higher image quality with tissue differentiation putting in mind that it is noninvasive, nonionizing radiation dependent, non-time consuming, repeatable, bedside technique in addition to the great advantage of dynamic evaluation of the vocal cords [12].
Also, laryngeal US has numerous advantages in the diagnosis of vocal cords palsy in pediatric age group as it is well tolerated by infants with no need for anesthesia, safe, reliable, and noninvasive bed side [12].
The aim is to evaluate the laryngeal ultrasound as a diagnostic tool to evaluate different laryngeal structure as regarded laryngeal dynamics (range and abnormality), and anatomical structures.
We managed to achieve these goals by measurements of distances and cross sectional areas, calculating the range of cross-sectional areas in patients with vocal fold palsy and partial laryngectomy, assessment of gender variations in normal controls, and identification of all anatomical structures of larynx.
On analysis of the results, it was found that both glottic area and inter-arytenoid distance varies significantly between the phonation and inspiration phases being wider in respiratory phase more than during phonation with a mean percent of change in inter-arytenoid length of 41.99 +/22.66% and a percent of change in glottic area of 40.82 +/25.85%.
We also found that the inter-arytenoid distances during phonation to be highest in partially laryngectomized patients 0.81 ± 0.37 cm with statistically significant difference than control group. This finding is due to the fact that one vocal fold is missing, so the distance will be greater than the control group. However, the percent of change in length and area were much less in group 3 (partially laryngectomized) than group 1 or 2. This could be explained by the fact that laryngeal reconstruction after partial laryngectomies may have decreased the pliability of the larynx causing this significant decrease in the area change than the normal.
On studying the relation between the age and vocal folds movements, it was found that there was inverse relation in males with statistically significance as regard change in area r = 0.713 and length r = 0.687, where the older the age, the less the change in the area between both phases phonation and respiration. This may be due to many possible contributing factors including gradual decline of lung capacity, reduced muscle bulk, decreased type I slow contracting muscle fibers, decreased hyaluronic acid in the lamina propria, arthritic changes, and ossification of the laryngeal skeleton.
A rather interesting finding after data analysis is that we found that change of area during respiration and during phonation was higher among females 53.07 ± 29.25 cm2 than among males 32.25 ± 20.47 cm2. The explanation of this is that vocal folds in females have less tensile stress than males for fixed percent elongation (from 2 to 5 times less) likely due to the approximately 59% of the collagen found in adult male vocal folds. Thus, female vocal folds are significantly less stiff than male vocal folds during equal elongation or strain.
A rather striking correlation was found between area minimum and length minimum which states that: to calculate area min., we can substitute in the following equation: A min = L min + 0.917. We also found that area max. (glottic areas during respiration) are related significantly to length max. (inter-arytenoid length during respiration) with another important statistically valid correlation. This strong correlation was found between area maximum and length maximum which states that: to calculate area max., we can substitute in the following equation: A max = L max + 1.111. These two equations are very important to determine glottic area by measuring inter-arytenoid distance.
We acknowledge the limitations to this study. The linear transducers and convex curved transducers are not conforming to neck anatomy and thus contributing to limiting views. These technical issues may be resolved by development of high-frequency concave curve transducer for preserving skin surface and probe contact; this is essential to assess the airway and airway-related anatomical structures as standard of care. Additional limitation is that the air-mucosa interface has linear hyperechoic appearance which is sometimes difficult to discriminate.
We experienced other technical limitation during our work where we found difficulty in stabilization of the probe over thyroid cartilage. We instructed all patients not to hold their breath as vocal cord movement can be fairly observed during quiet respiration. Some cases with dense laryngeal cartilage calcification can cause image distortion and poor image quality.
Conclusion
Laryngeal ultrasound is a reliable diagnostic tool on identifying different laryngeal anatomic structure, calculating various distances and areas with comparable accuracy to other previously used modalities as CT and MRI. In addition to the ability to diagnose laryngeal dynamic abnormality in patients with vocal fold palsy and partial laryngectomy. We recommend considering laryngeal ultrasound as initial method of screening in patient with query laryngeal injury either structural or functional (vocal cord palsy).
Availability of data and materials
All data generated or analyzed during this study are included in this published article are available from the corresponding author.
Abbreviations
- CT:
-
Computerized tomography
- MRI:
-
Magnetic resonance imaging
- US:
-
Ultrasound
- MHz:
-
Megahertz
- VC:
-
Vocal cord
- L max:
-
Length maximum
- L min:
-
Length minimum
- A max:
-
Area maximum
- A min:
-
Area minimum
- Phon:
-
Phonation
- Res:
-
Respiration
References
Friedman EM (1997) Role of ultrasound in the assessment of vocal cord function in infants and children. Ann Otol Rhinol Laryngol 106(3):199–209
Becker M, Burkhardt K, Dulguerov P, Allal A (2008) Imaging of the larynx and hypopharynx. Eur J Radiol 66(3):460–479
Vats A, Worley G, De Bruyn R, Porter H, Albert D, Bailey C (2004) Laryngeal ultrasound to assess vocal fold paralysis in children. J Laryngol Otol 118(6):429–431
Xia C, Zhu Q, Zhao H, Yan F, Li S, Zhang S (2013) Usefulness of ultrasonography in assessment of laryngeal carcinoma. Br J Radiol 86(1030):20130343
Dedecjus M, Adamczewski Z, Brzeziński J, Lewiński A (2010) Real-time, high-resolution ultrasonography of the vocal folds—a prospective pilot study in patients before and after thyroidectomy. Langenbecks Arch Surg 395(7):859–864
Ol'khova E, IuL S, Onufrieva E, Shchepin N (2009) Laryngeal ultrasound studies: potential, prospects, limitations. Vestn Otorinolaringol 5:9–12
Lapeña JF (2013) Mirrors and reflections: the evolution of indirect laryngoscopy. Ann Saudi Med 33(2):177–181
Kaplan MB, Ward DS, Berci G (2002) A new video laryngoscope—an aid to intubation and teaching. J Clin Anesth 14(8):620–626
Alvi S (2020) Harsha P. Flexible nasopharyngoscopy, StatPearls
Afsah OE (2015) Approach to diagnosis of vocal fold immobility: a literature review. Egyptian J Otolaryngol 31(2):78
Shawker TH, Sonies B, Stone M, Baum BJ (1983) Real-time ultrasound visualization of tongue movement during swallowing. J Clin Ultrasound 11(9):485–490
ALEEM M, NASSER HM (2019) Ultrasound diagnostic value in assessment of vocal cord mobility before neck surgery. Med J Cairo Univ 87(December):4371–4377
Acknowledgements
Not applicable.
Funding
This study did not receive funding, sponsorship, or financial support to be disclosed.
Author information
Authors and Affiliations
Contributions
The authors have read and approved the manuscript. AH, the corresponding author, contributed by doing the study concept and design, Also, patient recruitment, follow-up, and acquisition of data were by done by AA. Procedures were done by HM and AH. Analysis and interpretation of data and the drafting of the manuscript were done by HM. Revision of the manuscript was by HM and AH. Technical or material support was done by HM, AH, and AA.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Research Ethics Committee of the Faculty of Medicine at Ain shams University in Egypt. The Reference Number of approvals: not applicable. All patients included in this study gave written informed consent to participate in this work.
Consent for publication
All The patients in the study gave written informed consent for catheterization and for the possibility to publish the data within this research publication.
Competing interests
All The authors declare that they have no competing interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Nasser, H.M., Askoura, A. & Hussein, A. Ultrasonography diagnostic validity in structural and functional laryngeal disorders. Egypt J Radiol Nucl Med 51, 219 (2020). https://doi.org/10.1186/s43055-020-00334-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43055-020-00334-8