Abstract
Background
Comparing the diagnostic performance of widely used 2D FSE technique (fat-suppressed proton density; FS-PD) and the 3D technique (water-selective cartilage scan; WATS-c) in evaluation of the chondromalacia patella by using arthroscopy as reference standard
Results
Seventy-five adult patients were enrolled in this study. They underwent MRI examinations then arthroscopy done in 2–4 days after it. MRI was done using 2D (FS-PD) and 3D (WATS-c) sequences and MR images were compared by two radiologists separately, then grading of the cartilage lesions was performed according to modified Noyes grading system and comparison between grade 0–1, 2, and 3 lesions was done using arthroscopic findings as a reference. A false-negative result is considered if there was undergrading of chondromalacia and false-positive result if chondromalacia was overgraded. Each sequence sensitivity, specificity, and accuracy was calculated by both readers.
For reader 1, the sensitivity is 69% for WATS-c and 80% for FS-PD and the accuracy is 90% for WATS-c and 92% for FS-PD and for reader 2, the sensitivity is 56% for WATS-c and 84% for FS-PD and the accuracy is 88% for WATS-c and 94% for FS-PD.
Conclusion
2D FS-PD images showed better diagnostic performance than 3D WATS-c images for evaluating chondromalacia patella.
Similar content being viewed by others
Background
Chondromalacia patellae is a common patellar cartilage disorder which cannot be diagnosed only on the basis of taking the patient’s symptoms or doing physical examination. Although arthroscopy is the corner stone for diagnosis of chondromalacia patella, magnetic resonance imaging (MRI) is very helpful as a non-invasive method in the diagnosis of patellar chondral lesions [1, 2]. Increasing magnet strength and using a specialized coil increase both sensitivity and specificity in the diagnosis of chondromalacia. In MRI imaging, we have many pulse sequences used for the evaluation of patellar cartilage, one of the ideal pulse sequences is fat-suppressed proton density (FS-PD) which is very valuable in evaluating patellar cartilage as it has high spatial resolution, suitable contrast-to-noise (CNR) ratio, and good scan time [3, 4]. Recently, 3D imaging sequences appear to have a role for diagnosis. 3D T1-fast field echo is one of them that use cartilage water excitation (water-selective cartilage scan; WATS-c). It induces fat suppression by using water excitation [5, 6]. FS-PD sequence has an excellent performance in detecting lesions of patellar cartilage [7, 8], but the 3D sequences are superior in having much thinner slices than that of the 2D images that also gives good diagnostic value, so comparison between the two sequences is valuable in evaluating efficiency of each one in patellar cartilage diagnosis in cases of chondromalacia patella [9, 10].
This prospective study is based on the comparison between the diagnostic performance of widely used 2D fast spin echo (FSE) technique (FS-PD) and the 3D FFE technique (WATS-c) in evaluation of the chondromalacia patella by using arthroscopy as reference standard.
Methods
Patients
Between May 2016 and June 2017, 100 patients underwent MR knee examination were included in the study.
Patient with non-specific knee pain, clinically diagnosed chondromalacia patella, meniscopathy, history of trauma, and osteoarthritic changes are included; twenty-five patients who had tumors, had previous implants, or underwent surgery and patients with motion artifact in MRI images were excluded. Finally, MRI examinations of 75 adult patients (36 women patients and 39 men patients, their mean age 35 years; range, 16–76 years) were enrolled in this study. They underwent MRI examinations then arthroscopy done in 2–4 days after it. Approval was obtained for this prospective study by the institutional review board and all patients gave informed consent before doing MRI acquisition.
MRI examination
MRI examinations of the patellar cartilage was done using knee coil on 1.5-T MRI scanner (Intera; Philips Medical Systems; Best, The Netherlands) by using a 16 channel transmit/receive special dedicated knee coil, the patients were in the supine position. The 2D FSE fat-suppressed proton density (FS-PD) were obtained in axial images, the 3D T1 FFE with water excitation (WATS-c) sequence were also obtained in axial images. Table 1 shows the imaging protocols.
Evaluation of MR images
After doing MRI pulse sequences with data acquisition of all patients’ examinations, obtained MR images were studied and compared by the two radiologists separately and independently.
The grading of the cartilage lesions was performed according to their MRI appearance and following the modified Noyes grading system [11, 12] (Table 2): grade 0, denoting normal appearance of cartilage (homogeneous signal intensity of the cartilage, intact, its surface without fissuring, and normal cartilaginous thickness); grade 1, there is increased T2 signal intensity of morphologically normal cartilage not oriented at 55° to the external magnetic field; grade 2A, there is superficial cartilaginous partial-thickness defect which is less than 50% of the total cartilaginous articular surface thickness; grade 2B, there is cartilaginous deep partial-thickness defect which is more than 50% of the total cartilaginous articular surface thickness; and grade 3, there is full-thickness defect of cartilage.
Evaluation of patellar surface cartilage was done in four areas, i.e., upper part and lower part in both medial and lateral patellar articular facets. Recording of highest grade of each segment was done, and then arthroscopy was performed about 2 to 4 days after doing MRI.
By using the modified Noyes grading system, comparison between MRI grade 0–1, 2, and 3 lesions was done using arthroscopic findings as reference. A false-negative result is considered if there was undergrading of chondromalacia on the MRI examination, false-positive result if chondromalacia was overgraded.
Statistical analysis
Sensitivity, specificity, and accuracy of each MRI sequence for detection of patellar cartilage lesion were calculated by both readers.
Results
A total of 75 patients (M:F = 36:39; mean age, 35 years; range, 16–76 years) were included in our study.
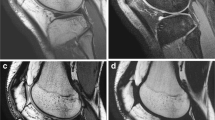
Twenty patients were grade 0, 28 were grade 1 lesions, 17 were grade 2 lesions, and 10 patients were grade 3 lesions were diagnosed by arthroscope. In MRI study, all grade 3 lesions were easily depicted by the two readers in each single pulse sequence, so there was statistical difference only in detection of grade 1 and 2 lesions (Figs. 1 and 2) and no significant difference in diagnosis of grade 3 (Fig. 3).
Thirty-three-year-old man with knee pain, 3D WATC-s image (a) showing normal cartilage thickness displaying bright signal intensity on WATS-c image with superficial linear area of low signal intensity in lateral patellar articular facet in keeping with grade 1 chondromalacia. FS-PD image (b) show corresponding linear area of abnormal high signal intensity on low signal of cartilage with reversing signal seen in WATS-c sequence
Sixty-eight-year-old woman with knee pain, two consecutive axial images of 3D WATS-c (a, b) showing multiple areas of low signal intensity in medial and lateral patellar articular facet with areas of full-thickness cartilage defect and underlying bony erosion in keeping with grade 3. Corresponding two consecutive images of FS-PD (c, d) show high signal intensity in cartilage and associated underlying bony erosion
For reader 1, the sensitivity is 69% for WATS-c and 80% for FS-PD, the specificity is 100% for WATS-c and 96% for FS-PD, and the accuracy is 90% for WATS-c and 92% for FS-PD.
For reader 2, the sensitivity is 56% for WATS-c and 84% for FS-PD, the specificity is 100% for WATS-c and 98% for FS-PD, and the accuracy is 88% for WATS-c and 94% for FS-PD (Fig. 4).
Discussion
Proton density (PD) sequence has been used in the evaluation of knee cartilage with good signal to noise ratio (SNR) comparable to other sequences. Furthermore, fat suppression increases cartilage lesions depiction, The FS-PD pulse sequence is very sensitive for depiction of chondromalacia patella and not only increases the accuracy in detection of cartilage lesions but also increases it in detection of underlying bony lesions in grade 3 chondromalacia patella [13, 14]. As fat-saturated proton density has high spatial resolution in a suitable scan time, it has been considered very efficient in evaluating patellar cartilage. Yoshioka et al. [15] reported that there is a higher signal to noise (SNR) in FS-PD than short tau inversion recovery (STIR) in articular cartilage imaging [16].
The 3D GRE pulse sequences have good images with high spatial resolution due to isotropic voxels; they provide better evaluation of articular cartilage but they are not optimal in assessment of subchondral bone. This assessment is very important in detecting the extent of both degenerative and traumatic cartilaginous lesions [17].
New sequences, which helped us to obtain good images of the patellar cartilage with both high isotropic spatial resolution and contrast resolution, like 3D intermediate-weighted FSE sequences which depend on changing flip angle and reduce time of acquisition that provide isotropic spatial resolution allow multiplanar reformatting with high quality that allows for good depiction of any lesions in subchondral bone [18].
Recently, many 3D sequences appear to be valuable and play a role in cartilage imaging and detecting cartilage lesions. A comparison was done in-between these new sequences and conventional 2D images. More recently, fat-suppression isotropic 3D sequences such as WATS-c appear and have to be included in the search to reach optimal image sequences for diagnosis [19, 20].
As it is less sensitive to magnetic field inhomogeneity, WATS-c sequence has the capacity to suppress fat signal much better than other presaturation techniques [21].
Most of studies done for evaluation of 3D MRI sequences have either surgical reference or arthroscopic reference standards, their aim was to qualitatively compare between these new sequences and the older 2D sequences FS-PD using multiple observers [22, 23].
It was reported by Schaefer et al. [8] that there were underestimation of grade 1 cartilage lesions on the 3D pulse sequences and there were poor internal contrast between intact cartilage and chondromalacia.
In our study, arthroscopic findings were used as a reference in comparing sensitivity, specificity, and accuracy of 2D FS-PD and 3D WATS-c by two radiologists.
In our study, sensitivity of FS-PD is higher than that of WATS-c as it is 80% and 69%, respectively, by one reader and 84% and 56%, respectively, by the other one; also, accuracy of FS-PD is higher than that of WATS-c as it is 92% and 90%, respectively, by one reader and the other one 94% and 88%, respectively; these results are coping with recent studies showed that FS-PD had a higher sensitivity and accuracy for cartilage pathology depiction than WATS-c did [9, 16, 22] as the abnormality found in internal cartilage is hidden by the presence of high signal intensity seen in WATS-c images and there is also low contrast between synovial fluid and cartilage that made it difficult to detect early pathological changes like cartilage fissures or fibrillation [17, 24, 25].
There is difficulty in evaluation of patellar cartilage lesions by both routine and cartilage-specific MRI sequences [26], In our study, WATS-c had both higher signal to noise and contrast to noise ratios than that of FS-PD [27] However, there is limitation of soft-tissue contrast as it has low T1/T2 values [28], and in our study, it is limited in seeing the cartilage substance for chondromalacia detection and also there is difficulty in surface irregularity detection due to joint fluid.
Conclusion
FS-PD images showed better diagnostic performance than 3D WATS-c images for evaluating chondromalacia patella.
Availability of data and materials
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- 3D MRI:
-
Three-dimensional magnetic resonance imaging
- FSE:
-
Fast spin echo
- FS-PD:
-
Fat-suppressed proton density
- WATS-c:
-
Water-selective cartilage scan
References
Outerbridge RE (1961) The etiology of chondromalacia patellae. J Bone Joint Surg Br 43(4):752–757
Pihlajamäki HK, Kuikka PI, Leppänen VV, Kiuru MJ, Mattila VM (2010) Reliability of clinical findings and magnetic resonance imaging for the diagnosis of chondromalacia patellae. J Bone Joint Surg Am 92(4):927–934
Gold GE, Chen CA, Koo S, Hargreaves BA, Bangerter NK (2009) Recent advances in MRI of articular cartilage. Am J Roentgenol 193(3):628–638
Crema MD, Roemer FW, Marra MD, Burstein D, Gold GE, Eckstein F et al (2011) Articular cartilage in the knee: current MR imaging techniques and applications in clinical practice and research. Radiographics 31(1):37–62
Mohr A, Priebe M, Taouli B, Grimm J, Heller M, Brossmann J (2003) Selective water excitation for faster MR imaging of articular cartilage defects: initial clinical results. Eur Radiol 13:686–689
Hauger O, Dumont E, Chateil JF, Moinard M, Diard F (2002) Water excitation as an alternative to fat saturation in MR imaging: preliminary results in musculoskeletal imaging. Radiology 224:657–663
Saadat E, Jobke B, Chu B, Lu Y, Cheng J, Li X et al (2008) Diagnostic performance of in vivo 3-T MRI for articular cartilage abnormalities in human osteoarthritic knees using histology as standard of reference. Eur Radiol 18:2292–2302
Schaefer FK, Kurz B, Schaefer PJ, Fuerst M, Hedderich J, Graessner J et al (2007) Accuracy and precision in the detection of articular cartilage lesions using magnetic resonance imaging at 1.5 Tesla in an in vitro study with orthopedic and histopathologic correlation. Acta Radiol 48:1131–1137
Bauer JS, Barr C, Henning TD, Malfair D, Ma CB, Steinbach L et al (2008) Magnetic resonance imaging of the ankle at 3.0 Tesla and 1.5 Tesla in human cadaver specimens with artificially created lesions of cartilage and ligaments. Investig Radiol 43:604–611
Hardy PA, Recht MP, Piraino DW (1998) Fat suppressed MRI of articular cartilage with a spatial-spectral excitation pulse. J Magn Reson Imaging 8:1279–1287
Kijowski R, Blankenbaker DG, Davis KW, Shinki K, Kaplan LD, Smet AAD (2009) Comparison of 1.5- and 3.0-T MR imaging for evaluating the articular cartilage of the knee joint1. Radiology 250(3):839–848
Gagliardi JA, Chung EM, Chandnani VP, Kesling KL, Christensen KP, Null RN et al (1994) Detection and staging of chondromalacia patellae: relative efficacies of conventional MR imaging, MR arthrography, and CT arthrography. AJR Am J Roentgenol 163(3):629–636
Sonin AH, Pensy RA, Mulligan ME, Hatem S (2002) Grading articular cartilage of the knee using fast spin-echo proton densityweighted MR imaging without fat suppression. AJR Am J Roentgenol 179:1159–1166
Mohr A, Roemer FW, Genant HK, Liess C (2003) Using fat-saturated proton density-weighted MR imaging to evaluate articular cartilage. AJR Am J Roentgenol 181:280–281
Yoshioka H, Stevens K, Hargreaves BA, Steines D, Genovese M, Dillingham MF et al (2004) Magnetic resonance imaging of articular cartilage of the knee: comparison between fat-suppressed three-dimensional SPGR imaging, fat-suppressed FSE imaging, and fat-suppressed three-dimensional DEFT imaging, and correlation with arthroscopy. J Magn Reson Imaging 20:857–864
Ristow O, Steinbach L, Sabo G, Krug R, Huber M, Rauscher I et al (2009) Isotropic 3D fast spin-echo imaging versus standard 2D imaging at 3.0 T of the knee – image quality and diagnostic performance. Eur Radiol 19(5):1263–1272
Friedrich KM, Reiter G, Kaiser B, Mayerhöfer M, Deimling M, Jellus V et al (2011) High-resolution cartilage imaging of the knee at 3T: basic evaluation of modern isotropic 3D MR-sequences. Eur J Radiol 78(3):398–405
Zur Y (2000) Design of improved spectral-spatial pulses for routine clinical use. Magn Reson Med 43:410–420
Recht MP, Piraino DW, Paletta GA, Schils JP, Belhobek GH (1996) Accuracy of fat-suppressed three-dimensional spoiled gradient-echo FLASH MR imaging in the detection of patellofemoral articular cartilage abnormalities. Radiology 198(1):209–212
Duc SR, Koch P, Schmid MR, Horger W, Hodler J, Pfirrmann CWA (2007) Diagnosis of articular cartilage lesions of the knee: prospective clinical evaluation of a 3D water-excitation true FISP sequence. Radiology 243(2):475–482
Mohr A (2003) The value of water-excitation 3D FLASH and fatsaturated PDw TSE MR imaging for detecting and grading articular cartilage lesions of the knee. Skelet Radiol 32:396–402
Yoshioka H, Stevens K, Genovese M, Dillingham MF, Lang P (2004) Articular cartilage of knee: normal patterns at MR imaging that mimic disease in healthy subjects and patients with osteoarthritis. Radiology 231:31–38
Hargreaves BA, Gold GE, Beaulieu CF, Vasanawala SS, Nishimura DG, Pauly JM (2003) Comparison of new sequences for high-resolution cartilage imaging. Magn Reson Med 49:700–709
Scheffler K (2004) Fast frequency mapping with balanced SSFP: theory and application to proton-resonance frequency shift thermometry. Magn Reson Med 51:1205–1211
Vlaardingerbroek MT, den Boer JA (2003) Magnetic resonance imaging: theory and practice, 3rd edn. Springer, New York
Van Dyck P, Kenis C, Vanhoenacker FM, Lambrercht V, Wouters K, Gielen JL et al (2014) Comparison of 1.5- and 3-T MR imaging for evaluating the articular cartilage of the knee. Knee Surg Sports Traumatol Arthrosc 22:1376–1384
Roemer FW, Hunter DJ, Guermazi A (2009) MRI-based semiquantitative assessment of subchondral bone marrow lesions in osteoarthritis research. Osteoarthr Cartil 17(3):414–415 author reply 416–417
Kijowski R, Blankenbaker DG, Klaers JL, Shinki K, De Smet AA, Block WF (2009) Vastly undersampled isotropic projection steady-state free precession imaging of the knee: diagnostic performance compared with conventional MR. Radiology 251(1):185–194
Acknowledgements
Not applicable
Funding
Not applicable
Author information
Authors and Affiliations
Contributions
AT contributed to the study concepts, study design, data acquisition, and manuscript preparation. WK contributed to the quality control of data and algorithms and manuscript review. AT and WK contributed to statistical analysis. ST contributed to the data analysis and interpretation and manuscript editing. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by Research Ethics Committee of Almana General Hospital, Saudi Arabia, on 21 April 2016 (reference number not available) All patients included in this study (all above 16 years old) gave written informed consent to participate in this research.
Consent for publication
All patients included in this research (all above 16 years old) gave written informed consent to publish the data contained within this study.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Tawfik, A.I., Kamr, W.H. & Taman, S.E. Comparison of 2D Fat Suppressed Proton Density (FS-PD) and 3D (WATS-c) MRI pulse sequences in evaluation of chondromalacia patellae. Egypt J Radiol Nucl Med 50, 85 (2019). https://doi.org/10.1186/s43055-019-0102-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43055-019-0102-z