Abstract
Background
The Achenbach System of Empirically Based Assessment (ASEBA) forms are among the most studied instruments for assessing behavioral, emotional, social, and thought problems in children and adolescents worldwide. Although ASEBA instruments have been translated into Arabic, fewer studies have investigated their psychometric properties and norms in Arabic speaking societies than in other societies.
Methods
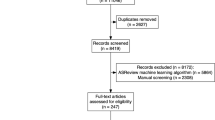
Revisions were made to the Modern Standard Arabic (MSA) translations of the Child Behavior Checklist for Ages 6–18 (CBCL/6–18), the Teacher’s Report Form (TRF), and the Youth Self-Report (YSR). Parents of 6–18-year-olds who came to the general pediatric clinic in Tanta University Hospital during a 2-year period for routine check-ups were invited to fill out the CBCL/6–18 (N = 595), while 11–18-year-olds were invited to fill out the YSR (N = 409). TRFs were filled out by teachers (N = 329).
Results
Confirmatory factor analyses supported the previously reported eight-factor syndrome structure of the forms with good psychometric properties and moderate cross-informant correlations. The mean CBCL/6–18 and YSR Total Problem scores qualified for the previously established ASEBA Multicultural Norm Group 2, while the mean TRF Total Problem score qualified for group 3.
Conclusions
The good psychometric properties and the identification of Multicultural Norm Groups for scores obtained with the Arabic translations of ASEBA forms in Egyptian society support use of the ASEBA for assessment and outcome evaluations of behavioral, emotional, social, and thought problems among Egyptian youth.
Similar content being viewed by others
Introduction
At any point of time, a significant minority of children and adolescents all over the world suffer from serious emotional, cognitive, and/or behavioral problems threatening their sound development, mental wellbeing, and hence the future of humanity at large [1, 2]. Throughout the history of psychological sciences, great efforts have been made to formulate clinical models that can successfully define and measure such clinical problems and differentiate them from normal variations in development [3]. Parallel to the “top-down” diagnostic approaches, which start from experts’ pre-defined constructs, a “bottom-up” approach emerged to explore normal versus abnormal psychological phenomena using empirical data comprising ratings of large samples of individuals in multiple societies. An important example of this approach is the Achenbach System of Empirically Based Assessment (ASEBA) [4].
Starting more than 50 years ago, the ASEBA team developed a family of instruments that assess different aspects of human behavior, as observed by multiple raters, spanning ages 1.5 to 90 + years [5]. Ratings of the ASEBA problem items were repeatedly analyzed via both exploratory and confirmatory factor analyses to derive scales for scoring syndromes of problems that co-occur in each age group [6]. The ASEBA forms are also scored on DSM-oriented scales comprising problems judged by international experts to correspond to DSM-IV and subsequently to DSM-5 diagnostic categories. The ASEBA scales and their correlates have been supported by data from dozens of societies across the globe [5, 6].
Three ASEBA instruments are designed to assess school-age children and adolescents. The Child Behavior Checklist for Ages 6 to 18 (CBCL/6–18) is completed by parents and other caregivers. The Teacher’s Report Form (TRF) is completed for 6–18-year-olds by teachers and other school staff. The Youth Self-Report (YSR) [4] is completed by 11–18-year-olds to describe themselves. Translations are available in more than 110 languages. Confirmatory factor analyses have supported the ASEBA’s eight syndromes in dozens of societies. Syndromes designated as Anxious/Depressed, Withdrawn/Depressed, and Somatic Complaints are scored on the broad-spectrum Internalizing scale. Syndromes designated as Rule-breaking Behavior and Aggressive Behavior are scored on the broad-spectrum Externalizing scale. Syndromes designated as Social Problems, Thought Problems, and Attention Problems are not scored on either of the broad-spectrum scales, but are included with all other problems in the Total Problem score [6]. Analyses of CBCL/6–18 forms completed by the parents of 72,493 children living in 45 societies across the world revealed that only 10% of the variance in problem scores was explained by cultural and societal differences. About 90% of the variance was explained by individual differences in parents’ ratings of their children. That is to say that most of the differences in these children’s behavior could be explained by individual variations rather than by cultural or societal differences [6, 7]. According to their deviation from the “omnicultural mean” (the mean of the mean Total Problem score in all societies), Achenbach classified different societies into three groups, Multicultural Norm Group 1 that included societies scoring more than one standard deviation (SD) below the omnicultural mean, Multicultural Norm Group 3 including societies scoring more than one standard deviation (SD) above the omnicultural mean, and Multicultural Norm Group 2 which included societies scoring from 1 SD below to 1 SD above the omnicultural mean [6]. The Total Problem scores overlapped between all societies so that no society was categorically different from any other society [6]. The modest correlations between ratings by different informants indicated that no one informant’s ratings sufficed for comprehensive evaluations of children [5].
With a large, mostly youthful [8], population, the Arabic world needs standardized instruments to evaluate the behavior of younger generations. Arabic, a semitic language within the afro-asiatic family originating in the Arabian Peninsula, is spoken by more than 350 million people around the world. However, Arabic language has different forms and dialects that include traditional Arabic (the language of the Quran), Modern Standard Arabic (MSA), used in schools, official papers and news bulletins, plus spoken dialects used for everyday oral communication varying greatly from one area to another [9]. The mutual intelligibility between spoken dialects is usually related to the distance between the areas where these dialects are spoken, with some dialects being mutually unintelligible [10]. The 22 Arabic-speaking states are roughly divided into 3 major segments: North African western Arabic world, Eastern Mediterranean, and gulf states. Egypt is the most populous country in the Arab world with a population exceeding 100 million, more than 40% less than 19 years old. Its central location and strong cultural relations to almost every Arab country both make Egypt a representative country for the Arab world [11]. As spoken dialects are region-specific and not usually used in written language, findings with Modern Standard Arabic translations of ASEBA instruments in Egypt may be especially informative for the Arabic world.
Several Arabic translations of ASEBA forms have been used in the Arab world. Two unpublished theses utilized Arabic translations of the 1991 versions of the CBCL/1.5–5 and CBCL/6–18 in community studies but did not establish psychometric properties in Egyptian society [12, 13]. Most subsequent studies used these Arabic translations for evaluation of clinical samples without testing its psychometric properties in community normative samples [14,15,16,17,18,19,20,21,22,23,24,25]. Two studies attempted to establish the psychometric properties of ASEBA forms in Arabic speaking countries, Algeria and Tunisia, using the 1991 versions of the CBCL/6–18 and YSR. However, these two studies used the French, not the Arabic, translations of the instruments [26, 27]. Another study attempted to evaluate the psychometric properties of the CBCL/6–18 in a large representative sample of youth in Qatar, a relatively small gulf state, and supported the factor structure of Achenbach’s eight-syndrome scales of the CBCL/6–18 [28]. However, because this study did not include other forms, such as the TRF and YSR, it could not test cross-informant correlations. An unpublished thesis tested psychometric properties of the CBCL/6–18 and TRF in a community sample of 1440 6–12-year-olds in the Egyptian city of Alexandria. The authors reported strong internal consistency and acceptable cross informant agreement but did not compare the results with previously reported multicultural norms for the ASEBA instruments [29]. To our knowledge, ours is the first test of the CBCL/6–18, TRF, and YSR in a community sample of Arab speaking families. We tested the psychometric proprieties and cross- informant correlations of the translated instruments and compared their scores with scores for previously established Multicultural Norm Groups [30]
Subjects and methods
First, the extant translations of the three ASEBA forms to Modern Standard Arabic were obtained from the ASEBA team. The translations were all thoroughly revised and modified by three bilingual professionals, a child psychiatrist, a psychologist, and a specialist of rhetoric and linguistics. Modified translations and back translations were sent back to the ASEBA team for checking. After final translated forms were agreed upon, the required licenses were obtained from the Research Center for Children, Youth, & Families at the University of Vermont, USA. Our study was approved by the Ethical Research Committee of the Faculty of Medicine, Tanta University under the approval code of 33,171/06/19.
The study was performed in Tanta University Hospital, a large public tertiary hospital serving a wide catchment area in the middle of the Nile delta. This area includes the Kafr El-Sheikh, Gharbia, and Monofia governates, with a population of about 13 million people, approximately 75% of whom live in rural areas [11]. We visited the general pediatric clinic in Tanta University Hospital on a regular basis between February 2020 and March 2022 and attempted to recruit all 6–18-year-olds coming to the clinic for routine check-ups and vaccinations for COVID-19 with no specific behavioral or psychiatric complaints, enrolled in regular school education, and accompanied by parents who had completed at least the 6 years of education needed to comprehend written Modern Standards Arabic. Parents signed statements of informed consent, while their children provided verbal assent. Parents were assured that information would be confidential and anonymous. We checked every form for completeness. Cases with missing data were excluded. Among 1998 distributed forms, 1333 were completed, including 595 CBCL/6–18 forms, 409 YSR forms, and 329 TRF forms. Some 66.7% of the targeted informants completed the forms.
Data analysis
All forms were scored using the Assessment Data Manager (ADM 9.1) software, Burlington, Vermont, USA. Confirmatory factor analyses (CFA) were performed using MPlus software to check if our data fit the eight-syndrome structure of the forms found in other societies [4, 7, 31]. As the observed variables are ordinal, Weighted Least Square Mean and Variance Adjusted (WLMSV) CFAs were conducted. The minimum sample to detect an effect was 177, which was exceeded for all three forms. To confirm the structure of the previously reported eight-factor model of the ASEBA instruments, the Jeffreys Amazing Statistics Program (JASP) software was utilized [32]. First, the reliability of the tools was evaluated using the McDonald Omega [33] coefficient. Values equal to or greater than 0.65 were considered satisfactory. Second, to confirm the construct validity, a CFA was conducted. Finally, the goodness-of-fit was evaluated using the Comparative Fit Index (CFI), root mean square error of approximation (RMSEA), and Tucker-Lewis Index (TLI).
Results
The mean age was 12.7 ± 3.1 years for the CBCL/6–18 sample (n = 595) and 11.9 ± 3.4 years for the TRF sample (n = 329). Youth who completed YSR forms for themselves (n = 409) ranged in age from 11 to 18 years, with a mean age of 14.0 ± 2.1 years. Females comprised 47.4% of the CBCL/6–18 sample, 49.8% of the TRF sample, and 47.9% of the YSR sample.
The McDonald Omega coefficients of the eight syndromes ranged from 0.65 (withdrawn/depressed) to 0.89 (aggressive behavior) for the CBCL/6–18; from 0.66 (thought problems) to 0.92 (aggressive behavior) for the TRF; and from 0.71 (withdrawn/depressed) to 0.87 for both Somatic Complaints and Aggressive Behavior for the YSR. RMSEA values for the CBCL/6–18, YSR, and TRF were 0.047, 0.040, and 0.044, respectively, indicating good fits for the three forms in the Egyptian sample. Good fit was also indicated by CFIs of 0.96 for the CBCL/6–18, 0.97 for the TRF, and 0.98 for the YSR. Finally, TLI values were 0.95, 0.96, and 0.98 for the CBCL/6–18, TRF, and YSR, respectively. The overall goodness-of-fit was thus good for all three forms. Most of the individual items showed good correlations with their factors (factor loadings of 0.50 and higher). Fewer items had moderate correlations (factor loadings between 0.30 and 0.50) [34] while only three items (32, 52, and 56 g) showed factor loadings less than 0.30 (For complete list of McDonald Omega coefficients and factor loadings, see Supplementary Tables S1–3). Factors were all significantly correlated to each other in all three instruments (Supplementary Tables S4–6).
The mean Total Problem scores were 28.7 ± 25.9 for the CBCL/6–18, 29.8 ± 30.3 for the TRF, and 36.7 ± 29.5 for the YSR. Relative to ASEBA Multicultural Norm Groups [5,6,7, 31], the mean score for our CBCL/6–18 sample was at the high end of Multicultural Norm Group 2 (medium scores). The mean score for our TRF sample was at the low end of Multicultural Norm Group 3 (high scores), while the mean score for our YSR sample was at the low end of Multicultural Norm Group 2 (medium scores). The means and standard deviations of the individual scale scores for the three instruments are listed in Tables 1, 2, and 3. Cross-informant correlations were computed for forms completed for the same individuals. Moderate correlations were found between Internalizing, Externalizing, and Total Problem scores from the CBCL, TRF, and YSR (Table 4).
Discussion
To our knowledge, this is the first test of the psychometric properties of the Modern Standard Arabic translations of the CBCL/6–18, TRF, and YSR. We found good psychometric properties, including replication of the previously reported [28, 31] eight syndromes with good fit of the model for all three instruments. When compared to the previously reported multicultural norms [5, 6, 31], our Egyptian Total Problem scores were at the high end of the ASEBA Group 2 (medium scores) for the CBCL/6–18, the low end of Group 2 for the YSR, and at the low end of Group 3 (high scores) for the TRF.
The problem scores for all three forms were in the medium to high range for studied societies, an unsurprising finding given the central location of Egypt in the Middle East that made it a historical hub for many interacting Eastern and Western cultures, which have traded, colonized, and mixed with the Egyptian population. The frequent long-term mixing between different ethnic groups characteristic for regions like Egypt may lead to moderation of genetic susceptibility to different emotional and behavioral problems leading to the noted pattern of medium scores. The mean Egyptian CBCL/6–18 scale scores approximated the corresponding mean scale scores in Multicultural Group 2 except for the Anxious/Depressed, Withdrawn/Depressed, and Internalizing problem scores of the school-age boys, which were comparable to the scores of Multicultural Group 3. A previous study by our team [35] found depressive disorders to be the second most common diagnoses after ADHD in a large clinical sample of Egyptian children. Overcrowded population together with strained economic conditions and culturally accepted physical punishment might contribute to elevated levels of depressive problems in Egyptian children [25]
The modest cross-informant correlations reported in previous studies [36, 37] support the use of forms completed by multiple informants to obtain a comprehensive understanding of the child. Our correlation of 0.54 between CBCL and YSR Total Problem scores was larger than the mean of 0.41 reported by Rescorla et al. [38] in a sample totaling 27,861 adolescents from 25 societies. Rescorla et al. reported correlations ≥ 0.50 in samples from Tunisia, Algeria, Germany, Lithuania, Korea, and Denmark. Our correlation of 0.52 between CBCL and TRF Total Problem scores was also above the mean of 0.26 reported by Rescorla et al. [39] in samples totaling 27,962 children from 21 societies, but a correlation as high as 0.49 was reported for the Danish sample. The large percentage of Egyptian families that use private home tutoring instead of regular schools [40], with continuous communication between family and home tutors and being at home rather than in classrooms, might explain the higher correlation between parent and teacher reports than found in many other societies. Despite the relatively high cross-informant correlations in our sample.
Our study was limited by a relatively small sample size, recruited from one center. This makes it difficult to generalize our findings to the entire Egyptian population. Second, the socioeconomic status of the families was not assessed. Third, only parents who completed 6 years of school and youth who attend school participated in the survey. Illiterate parents and youth who dropped out of school were excluded as they cannot read Modern Standard Arabic. The omission of school dropouts might not affect the representativeness of the youth sample, as the drop-out rate from Egyptian middle schools is currently only 0.87% [11]. However, the representativeness of the parent sample is limited, as 24.9% of Egyptian adults were illiterate in 2019 [11]. Finally, the sample was partially recruited during COVID-19 lockdown, which although limited in Egypt, might still be a psychosocial stressor that could have altered the psychological status of both youth and their families.
Conclusions
The use of standardized psychometric tools in assessment of youth is still a rare phenomenon in the clinical practice of child and adolescents in Egypt and other Arab countries. By providing Egyptian data for ASEBA forms, our study may help practitioners to screen, assess, and follow up Egyptian and other Arab children and adolescents with emotional and behavioral problems.
Availability of data and materials
The dataset created and analyzed during the current study will be available from the corresponding author on reasonable request.
Change history
11 October 2023
A Correction to this paper has been published: https://doi.org/10.1186/s43045-023-00368-4
Abbreviations
- ADM:
-
Assessment Data Manager
- ASEBA:
-
Achenbach System of Empirically Based Assessment
- CBCL:
-
Child Behavior Checklist
- CFA:
-
Confirmatory factor analyses
- CFI:
-
Comparative Fit Index
- COVID:
-
Coronavirus disease
- DSM:
-
Diagnostic and Statistical Manual of Mental Disorders
- ICD:
-
International Classification of Disease
- MSA:
-
Modern Standard Arabic
- RMSEA:
-
Root means square error of approximation
- SD:
-
Standard deviation
- TLI:
-
Tucker–Lewis index
- TRF:
-
Teacher Report Form
- USA:
-
United States of America
- WLMSV:
-
Weighted Least Square Mean and Variance Adjusted
- YSR:
-
Youth Self-Report
References
Costello EJ et al (2003) Prevalence and development of psychiatric disorders in childhood and adolescence. Arch Gen Psychiatry 60(8):837–844
O’Connell ME, Boat T, Warner KE (2009) Preventing mental, emotional, and behavioral disorders among young people: progress and possibilities. The National Academic Press, Washington, DC
Achenbach T, Ndetei DM (2012) Clinical models for child and adolescent behavioral, emotional, and social problems. R. JM, Editor. In: IACAPAP e-Textbook of Child and Adolescent Mental Health. International Association for Child and Adolescent Psychiatry and Allied Professions, Geneva
Achenbach T, Rescorla LA (2001) Manual for the ASEBA school-age forms & profiles. Research Centre for Children, Youth and Families, University of Vermont, Burlington
Achenbach TM (2009) The Achenbach System of Empirically Based Assessment (ASEBA): development, findings, theory, and applications. University of Vermont, Research Center for Children, Youth, & Families, Burlington
Achenbach TM (2019) International findings with the Achenbach System of Empirically Based Assessment (ASEBA): applications to clinical services, research, and training. Child Adolesc Psychiatry Ment Health 13:30
Rescorla LA et al (2019) Effects of society and culture on parents’ ratings of children’s mental health problems in 45 societies. Eur Child Adolesc Psychiatry 28(8):1107–1115
Hassan I, Dyer P (2017) The State of Middle Eastern Youth. The Muslim World 107(1):3–12
Hooshmand D (2019) Arabic dialects compared: Maghrebi, Egyptian, Levantine, Hejazi, Gulf, and MSA", discover discomfort
(2021) Varieties of Arabic. www.wikipedia.org. https://en.wikipedia.org/wiki/Varieties_of_Arabic#cite_note-3. Cited 2022 4–11
Egypt Central Agency for Public Mobilization And Statistics (CAPMAS) (2018) Egypt in numbers
El Hady M, Atef A, El Defrawy MH, El Wahab AA (1995) Psychiatric and behavioral problems in preschool children in Ismailia city in psychiatry. University of Suez Canal, Suez City, p 168
Koura M, Abdelaal NM, Seif-eldin AG, Khairy AE (1991) A study of the role of Alexandria primary health care program in the assessment of behavior disorders of primary school children. Dol:, in Publish Health. Alexandria University, Alexandria. p 202
Auerbach JL, Yirmiya N, Kamel FN (1996) Behavior problems in Israeli Jewish and Palestinian preschool children. J Clin Child Psychol 25:398–405
El-Defrawi MH (1997) Psychiatric disorders in a sample of Egyptian preschool children. Egypt J Psychiatr 20:271–282
Al-Asmary SM, Abdel-Fattah MM, Asal AA, Al-Helali NS, Al-Jabban TM, Arafa MA (2004) Emotional and behavioral problems among male Saudi schoolchildren and adolescents. Neurosciences (Riyadh) 9(4):299–306
Eapen V et al (2004) Child psychiatric disorders in a primary care Arab population. Int J Psychiatry Med 34(1):51–60
Loughry M et al (2006) The impact of structured activities among Palestinian children in a time of conflict. J Child Psychol Psychiatry 47(12):1211–1218
Yunis F et al (2007) Psychometric properties of the Child Behavior Checklist/2-3 in an Arab population. Psychol Rep 100(3 Pt 1):771–776
Mubarak AA, Elsawy HE, Seleem MA, Abdel-Wahab DM (2016) Self-concept and psychiatric comorbidity in a sample of Egyptian adolescents with secondary nocturnal enuresis. Egypt J Psychiatr 37:17–24
Bahnasy WS, El-Heneedy YA, El-Seidy EA, Ibrahim IS, Seleem MA, Ahmed AY (2018) Primary monosymptomatic nocturnal enuresis: an etiological study. Egypt J Neurol Psychiatry Neurosurg 54:19
Eldod AE, Eid MA, Heba AA, Seleem MA, Fnoon NF (2015) Role of the serotonin transporter gene in susceptibility to mood disorders in children of depressed parents. Egypt J Psychiatr 36:73–85
Seleem MA, El-Seht R, Saada SA (2016) Parenting discipline styles and child psychopathology in a sample of Egyptian children with accidental ocular trauma: a case–control study. Middle East Curr Psychiatr 23(4):188–193
Shaaban SS, Seleem MA, Badawy AA, Eissa MA (2020) Psychiatric comorbidities among children with attention deficit hyperactivity disorders. J Adv Med Med Res 32:85–96
Seleem MA, Amer RA (2020) Parenting discipline styles and child psychopathology in a clinical sample of Egyptian children in the Nile Delta region. Middle East Curr Psychiatr 27(56):1–11
Petot D, Petot JM, Achenbach TM (2008) Behavioral and emotional problems of Algerian children and adolescents as reported by parents. Eur Child Adolesc Psychiatry 17(4):200–208
Chahed M (2010) Contribution of the Child Behavior Checklist (CBL) and the Youth Self-Report (YSR) to the study of the emotional and behavioral disorders of Tunisian children and adolescents (in Frensh), in Psychologie clinique. Université Paris Nanterre, Paris
Al-Hendawi M, Keller C, Cloninger L (2016) A psychometric analysis of the child behavior checklist for elementary school children in Qatar. Assess Eff Interv 41:220–229
Ibrahim NN, Wahdan IM, Abou-Nazel MW, Sallam SA (2016) Psychometric properties and diagnostic accuracy of the Arabic version of the strngths and difficulties questionnaire and the child behavior checklist, in epidemiology. Alexandria. p. 122
Achenbach TM, Rescorla L (2007) Multicultural Supplement to the manual for the ASEBA school-age forms & profiles: child behavior checklist for ages 6–18, teacher's report form, youth self-report: an integrated system for multi-informant assessment. ASEBA, Vermont
Ivanova MY et al (2007) Testing the 8-syndrome structure of the child behavior checklist in 30 societies. J Clin Child Adolesc Psychol 36(3):405–417
JASP Team (2019) JASP (Version 0.17) [Computer software]
Hayes AF, Coutts JJ (2020) Use omega rather than Cronbach’s alpha for estimating reliability. Commun Methods Meas 14(1):1–24
Tavakol M, Wetzel A (2020) Factor analysis: a means for theory and instrument development in support of construct validity. Int J Med Educ 11:245–247
Seleem MA et al (2019) Demographic and clinical characteristics of children seeking psychiatric services in the Nile Delta region: an observational retrospective study. Int J Ment Health Syst 13:66
Achenbach TM, Krukowski RA, Dumenci L, Ivanova MY (2005) Assessment of adult psychopathology: meta-analyses and implications of cross-informant correlations. Psychol Bull 131(3):361–382
Achenbach TM, McConaughy SH, Howell CT (1987) Child/adolescent behavioral and emotional problems: implications of cross-informant correlations for situational specificity. Psychol Bull 101(2):213–232
Rescorla LA et al (2013) Cross-informant agreement between parent-reported and adolescent self-reported problems in 25 societies. J Clin Child Adolesc Psychol 42(2):262–273
Rescorla LA et al (2014) Parent-teacher agreement on children’s problems in 21 societies. J Clin Child Adolesc Psychol 43(4):627–642
Kabadaya M (2020) Students’ participation in private tutoring activities in Egypt in Egyptian lower primary schools: a qualitative investigation, in International and Comparative education. The American University in Cairo (AUC), Knowledge Fountain
Acknowledgements
We would like to express our deep appreciation to the late professor Leslie Rescorla for her help and support in revising our back translations of the ASEBA forms. We are also indebted to Lori V. Turner and Masha Ivanova from the University of Vermont Research Center for Children, Youth, and Families (RCCYF), which publishes the Achenbach System of Empirically Based Assessment (ASEBA), for their kind and patient help in handling and analyzing our statistical data. We are also sincerely grateful for our clinical psychologists, social workers, and nursing teams in Tanta University Hospitals and for all participating families.
Funding
This study was self-funded by the authors. Subjects were willing to participate without any monetary compensation.
Author information
Authors and Affiliations
Contributions
MS planned and supervised the project’s team, revised the extant Arabic translations of the forms, participated in statistical analysis of the results, participated in writing, and revising the manuscript, and is responsible of responding to the reviewers’ comments. RA participated in recruiting families and youth to fill in the forms, applied for the ethical board approval, and participated in writing the manuscript. ME participated in recruiting families and youth to fill in the forms and participated in writing the manuscript. SS participated in back translating revised translations and participated in statistical analysis of the results. EA participated in statistical analysis of the results, and in writing the results section in the manuscript. YE, SA, and IK all participated in recruiting families and youth to fill in the forms and participated in writing the manuscript. Finally, TA suggested the idea of the work, planned, and supervised the study design and revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Ethical Research Committee of the Faculty of Medicine, Tanta University under the approval code of 33171/06/19.
Consent for publication
All participating authors consent for publication.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original version of this article was revised: “Affiliation details have been updated.
Supplementary Information
Additional file 1: Supplementary Table S1.
Factor Loadings of CBCL/6-18. Supplementary Table S2. Factor Loadings of TRF. Supplementary Table S3. Factor Loadings of YSR. Supplementary Table S4. Factor Correlations of CBCL/6-18. Supplementary Table S5. Factor Correlations of TRF. Supplementary Table S6. Factor Correlations of YSR.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Seleem, M.A., Amer, R.A., Elhosary, M. et al. Psychometric properties and cross-cultural comparison of the Arabic version of the Child Behavior Checklist (CBCL), Youth Self Report (YSR), and Teacher’s Report Form (TRF) in a sample of Egyptian children. Middle East Curr Psychiatry 30, 61 (2023). https://doi.org/10.1186/s43045-023-00328-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43045-023-00328-y