Abstract
Background
The use of oxytocin as a therapy to treat social deficiencies in autism spectrum disorders (ASD) is gaining popularity. This study aimed to determine oxytocin nasal spray’s effect in combination with applied behavior analysis (ABA) method in improving social impairments in pediatrics with ASD.
Results
Our study’s main findings have revealed that intervention with INT-OXT compared to NS effectively reduced the ASD index and stereotyped behaviors on the GARS-2 scale (p < 0.05), in addition to teacher and parent’s SDQ mean score (p < 0.001). Also, during the follow-up time, the intervention with INT-OXT in ASD index, stereotyped behaviors, communication, social interaction, and parent and teacher mean SDQ scores were statically significant (p < 0.001).
Conclusions
In pediatrics with autism aged between 4 and 17 years, a 6-week course of INT-OXT combination therapy with ABA improved GARS-2 and teacher and parent SDQ scores compared to NS.
Similar content being viewed by others
Background
Autism spectrum disorder (ASD) is a severe neurodevelopmental disorder that affects people of all racial and socioeconomic backgrounds [1]. It is known to manifest before age 3 and affects boys four times more often than girls [2]. Autism spectrum disorder has three diagnostic symptom domains: limited social interaction, verbal and nonverbal communication, and constrained, repetitive behavior patterns, interests, or hobbies [3]. Individuals with the autistic phenotype are less skilled in typical social interaction, expressive language, nonverbal communication (such as maintaining eye contact), peer relationships, and behavioral flexibility [4]. Autism spectrum disorder is prevalent in 0.1% of children between 6 and 18 in Iran, with a male-to-female ratio of 2:1 [5].
According to recent studies, intranasal oxytocin (IN-OXT) may be a possible treatment for ASD [6,7,8]. Intranasal OXT treatment promotes in-group trust [9] and interoceptive awareness [10] while decreasing fear [11], according to studies in normally developing individuals. On the other hand, preclinical research has shown that OXT plays a critical part in sociality. For instance, OXT controls or begins grooming and social recognition behaviors in mammalian nonhuman models and other pro-social behaviors, including paternal and reproductive activity [12, 13]. There is growing interest in the application of OXT to improve social communication deficits in ASD since there is a need for effective therapies for core ASD symptoms. Benefits in social functioning, including improved emotion detection [7], greater eye gaze [14], and improved emotions of trust in others [15], have been observed in certain research on the effects of IN-OXT in ASD.
The mechanisms of action of OXT remain unclear, despite accumulating indications that it may be therapeutically advantageous for at least a sizable percentage of people with ASD. The ability of OXT to modify the sensitivity to and perceived salience of external rewards that impact behavior and support reward-based learning may be one possible mechanism of action. Preclinical research suggests that OXT exerts its pro-social effects through the mesocorticolimbic dopamine pathway [16, 17]. This neural network consists of midbrain components (ventral tegmental area (VTA) and substantia nigra), the striatum, and cortical areas such as the orbitofrontal, anterior cingulate, and prefrontal cortices [18]. The interaction between OXT and mesocorticolimbic dopamine increases dopaminergic activity across the whole mesocorticolimbic system when OXT-responsive neurons in the VTA are activated [19].
Recent studies show that the effects of OT are small and elusive and depend on biological and psychological factors. Long-term treatment could be more beneficial than single-dose administration [20,21,22]. This study aimed to determine the effect of 6 week’s administration of oxytocin nasal sprays concomitant to the applied behavior analysis (ABA) method to improve social impairments in pediatrics with ASD.
Methods
Participants
This study was a randomized, double-blind, placebo-controlled, parallel design trial. The study was done in Isfahan, Iran, Autism Center from December 2021 to March 2022.
Pediatrics between the ages of 4 and 17 with a verified diagnosis of ASD based on the Diagnostic and Statistical Manual of Mental Disorders V met the inclusion criteria [23]. Major psychiatric disorders, like bipolar disorder, psychosis, post-traumatic stress disorder, schizophrenia, major depressive/anxiety disorder, a history of significant neurological diseases such as unstable epilepsy disorder, known genetic syndromes, known abnormal brain magnetic resonance imaging (structural brain lesions), and evidence of or a history of malignancy or any significant hematological, endocrine, or gastrointestinal disorder, were all exclusion criteria. In addition, we do not included high-functioning autism patients.
The study protocol was approved by the Isfahan University of Medical Sciences Ethics Committee (IR.MUI.MED.REC.1400.442) and the Iranian registration of clinical trials (IRCT20211004052670N1). The parent or legal guardian of each participant provided written informed permission for their involvement in the trial, and, where necessary, participants’ agreement was also acquired. The modified Declaration of Helsinki regulations were followed throughout the experiment. The trial was free of any commercial interference.
Random double blocks allocated participants to either INT-OXT or NS group. An impartial assessor who was blinded to the groups’ assignments and side effects conducted all effectiveness evaluations. A doctor who was unaware of the group assignment conducted each safety assessment.
Medication
Intranasal sprays of oxytocin (Syntocinon; NOVARTIS) and a normal saline (NS) were given. In the morning, participants were given 24 IU (six puffs) of INT-OXT or an NS once a week, 15 min before starting ABA. Participants were told to take one puff every 30 s while switching nostrils in a straight position. To ensure proper administration and tolerability, each participant took their first dosage in front of the research doctor. The placebo included regular NS in the same bottles and labeling. After the first dosage, participants were asked to remark on the taste and scent. Also, to ensure dosing compliance, bottles were weighed after use. No person mentioned a scent. The research pharmacist designed a computer-generated randomization table that was utilized to randomize participants. Caregivers recorded adverse events during the study period. It should also be noted that none of the children had used previous medication regimens for ASD.
Applied behavior analysis
Applied behavior analysis is a scientific method in which techniques based on behavioral principles are consistently utilized to find environmental factors influencing socially appropriate behavior and are then used to create tailored and effective treatments. The teaching of fundamental communication, games, sports, social interaction, everyday living, and self-help skills with this system is quite successful [24]. The ABA sector has seen even more substantial expansion in behavioral therapies for children with autism, as the rising number of service providers and qualified experts in the field has revealed [25]. Studies show that ABA has helped children with ASD improve their social, linguistic, and cognitive skills since the mid-1980s [26,27,28]. In this study, a trained psychiatrist performed ABA for each person once a week in both groups. In each session, 15 min before ABA onset, INT-OXT or NS was administered, and then, the ABA therapy started and lasted for 4 h.
Measures
The strengths and difficulties questionnaire (SDQ) and Gilliam Autism Rating Scale-2 (GARS-2) were used to assess the main outcomes. Questionnaires were filled at baseline before starting INT-OXT or NS, at the end of the first session, at the end of the study in week 6 (session six which administrations were ended), and at the end of 6 weeks of follow-up after the ending study.
Strengths and difficulties questionnaire (SDQ)
The SDQ is a 25-item screening tool created to assess children’s and teenagers’ social, emotional, and behavioral functioning. It encompasses four clinical domains, including conduct issues, emotional symptoms, hyperactivity-inattention, peer-relationship issues, and emotional symptoms, as well as one specific prosocial behavior category. A Likert scale of 3 points is used to score each item [29]. The SDQ effectively separates children with ASD from other kids with and without psychiatric conditions [30]. Through a study on the psychometric properties of SDQ in an Iranian sample, the SDQ in Persian was a reliable instrument for identifying mental health issues in children and is available in both parent and teacher forms [31].
Gilliam Autism Rating Scale-2 (GARS-2)
The Diagnostic and Statistical Manual of Mental Disorders diagnostic criteria and the Autism Society of America’s (1994) definition of the disorder are used to evaluate autism using the parent-report survey known as the GARS-2 [32]. The three GARS-2 subscales, stereotyped behaviors, social interaction, and communication, are based on the three primary symptomological categories of the illness. The AI, which has a mean score of 100 and a standard deviation of 15, is the result of summing the subscale scores. The AI score is a general assessment of the severity of autism [33]. Also, in the psychometric properties study of GARS in Iranian samples, results indicated that the GARS scale is reliable for assessing autism. In terms of good validity and reliability, this scale can be employed in research and treatment facilities [34].
Sample size
The sample size was estimated using the following formula and based on the data extracted from the study of Hollander et al. [35]:
-
Z1: 95% confidence interval = 1.96
-
Z2: 80% power = 0.84
-
S = 20 for the score of the GARS-2 questionnaire, which is one-sixth of the range of changes, i.e., zero to 120
-
D = the minimum difference in the mean score of Conners between the two groups, which is considered 14. As a result, the number of 32 people is calculated. And taking into account 10% dropout, the sample size for the study was estimated at 70 people.
Statistical analysis
Statistical analysis was performed in SPSS 24 for Windows (IBM Inc., Armonk, NY, USA). The Kolmogorov–Smirnov test confirmed the normal distribution of the data. Categorical data were compared using chi-square, and the repeated-measure ANOVA model was used for continuous parameters. An alpha error of 0.05 was set as the critical point of significance.
Results
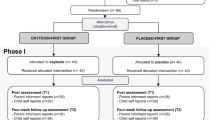
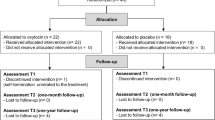
Seventy children with ASD were divided into the INT-OXT (intervention) and NS (control) groups. During the study period, 11 patients (three in the INT-OXT group and eight in the NS group) were excluded from the study due to the lack of follow-up visits. Finally, data analysis was performed on 59 cases (32 in INT-OXT and 27 in NS groups) (Fig. 1).
The mean age of the INT-OXT and NS groups was 11.5 ± 3.1 and 10.03 ± 2.8 years, respectively, and there was no significant difference between them (p > 0.05). In the INT-OXT and NS groups, 21 and 17 (65.6% versus 63%) were boys, and the rest were girls, and no significant difference was seen between the two groups (p > 0.05). The mean intelligence quotient (IQ) score in the above two groups was 73.5 ± 4.3 and 75.3 ± 3.8, respectively, and no significant difference was seen between the two groups (p > 0.05). The financial status of 16 cases from the INT-OXT group and 19 cases from the NS group (50% vs. 70.4%) was poor, and the rest were moderate, and no significant difference was seen between the two groups (p > 0.05) (Table 1).
The GARS-2 mean ASD index in the INT-OXT group decreased from 76.9 ± 14.5 at baseline to 54.19 ± 15.13 posttreatment compared to the NS group (75.2 ± 8.7 to 69.78 ± 11.12) (p < 0.05). The results demonstrated that intervention with INT-OXT on the ASD index was significant during the overall study follow-up time (p < 0.001). Also, the trend of decretion in both groups was statically significant (p < 0.001).
Furthermore, the stereotyped behaviors mean in the INT-OXT group significantly decreased from baseline to posttreatment compared to the NS group (24.1 ± 5.5 to 16.6 ± 5.9 vs. 25.7 ± 4.7 to 21.3 ± 4.6) (p < 0.05). Also, this decretion was significant during the overall study follow-up time (p < 0.001). But the trend of decretion in both groups was not statically significant (p > 0.05).
Still, communication and social interactions mean scores did not show significant differences between the two groups (p > 0.05). But the decretion trend in both groups during the study was statically significant (p < 0.001) (Table 2; Fig. 2).
The parent SDQ mean score in INT-OXT group at baseline was 51.3 ± 2.7 and decreased significantly to 46.8 ± 3.3 posttreatment. This decretion during the follow-up compared to the NS group was statically significant. In addition, the teacher SDQ mean score in the INT-OXT group decreased from 60.3 ± 3.7 at baseline to 46 ± 3.2 posttreatment. Also, this decretion during follow-up time compared to the NS group was significantly meaningful (p < 0.001).
In addition, this decretion for both SDQ questionnaires during the study follow time was significant (p < 0.001). Also, the decretion trend in both groups was significant for parent SDQ (p < 0.001) and for teacher SDQ (p < 0.05) (Table 3; Figs. 3 and 4).
Adverse event
All individuals tolerated the nasal spray well, and no adverse event was reported.
Discussion
Our study’s main findings have revealed that intervention with INT-OXT compared to NS effectively reduced the ASD index and stereotyped behaviors (GARS-2 scale) and the teacher and parent’s SDQ mean scores. Also, in the ASD index, stereotyped behaviors, communication, social interaction, and parent and teacher mean SDQ scores, the intervention with INT-OXT during follow-up time was significantly effective. Despite preclinical evidence that OXT may be a viable therapeutic for human social impairments, prior intranasal OXT treatment trial findings for ASD have been conflicting; some trials claimed that OXT improves social abilities [22, 36], while others did not [37, 38]. A double-blind, randomized, placebo-controlled, parallel design study on the effect of INT-OXT (24 international units, twice daily) on the treatment of social deficits in ASD patients has demonstrated that children with ASD showed dramatically improved social skills after a 4-week intranasal OXT therapy compared to placebo. Additionally, they discovered that pretreatment blood OXT levels predicted treatment outcomes, with those with the lowest pretreatment OXT levels demonstrating the largest social progress [39].
Furthermore, a 5-week double-blind clinical trial of nasal oxytocin spray (24 IU per day) increased caregiver-rated social responsiveness. It was discovered that oxytocin therapy was well tolerated, and there were no appreciable variations in the reported adverse events between conditions [36]. In a study of the effectiveness of 4-day continuous oxytocin administration in 38 males with ASD aged 7–16 years in a randomized, double-blind, placebo-controlled methodology, during parent–child interaction training sessions, intranasal placebo or oxytocin, in 12- or 24-IU dosages depending on body weight, was delivered once daily. At several measurement time points, parent reports, clinician evaluations, and independent observations were utilized to assess side effects, social interaction skills, repetitive behaviors, emotion identification, and diagnostic status in all individuals with ASD and their parents. However, compared to a placebo, intranasal oxytocin had no meaningful effect on all outcomes in children with ASD [37]. One study revealed that a 6-week course of OXT intranasal administration (24 IU, single dose) plays its role in ASD core symptoms by enhancing brain activity and improving functional coordination in the medial prefrontal region (mPFC) [22]. In a study on the plausible neurobiological mechanism of OXT-induced behavioral enhancement, it has been shown that modulation of the reward prediction errors (RPEs) signal in the nucleus accumbens (NAcc) is a critical neuronal hub for reinforcement-based learning. Their findings suggest that OXT’s beneficial effect on social processing in ASD is mediated by a selective enhancement of the brain’s motivational system in response to social stimuli, eventually boosting reinforcement learning in social situations [40]. Many challenges remain, such as optimizing delivery route, dosage, and therapy duration and developing a technique to measure improvements in ASD core symptoms.
We draw attention to the study’s shortcomings, which include its dependence on caregiver, teacher, and parent reports as outcome measures and its modest sample size. In this area, where many elements still need to be investigated in order to establish the therapeutic value of oxytocin, funding for independently led, well-powered clinical studies must continue to be prioritized.
The role of parental belief in modulating OT treatment responses which were evaluated using SDQ in this trial was the novelty of this study.
Conclusions
Among children with autism aged between 7 and 17 years, a 6-week course of INT-OXT (24 IU per day) along with ABA improved GARS-2 and teacher and parent SDQ scores compared with a placebo.
Availability of data and materials
The corresponding author, Safie Shafiezadegan Isfahani, had full access to all of the data in this study and took complete responsibility for the data’s integrity and the data analysis’s accuracy.
Abbreviations
- IN-OXT:
-
Intranasal oxytocin
- ASD:
-
Autism spectrum disorders
- ABA:
-
Applied behavior analysis
- VTA:
-
Ventral tegmental area
- NS:
-
Normal saline
- SDQ:
-
Strengths and difficulties questionnaire
- GARS-2:
-
Gilliam Autism Rating Scale-2
- IQ:
-
Intelligence quotient
- RPEs:
-
The reward prediction errors
- mPFC:
-
Medial prefrontal region
- NAcc:
-
Nucleus accumbens
- IU:
-
International unit
References
Fombonne E (2009) Epidemiology of pervasive developmental disorders. Pediatr Res 65(6):591–598
Baron-Cohen S, Knickmeyer RC, Belmonte MK (2005) Sex differences in the brain: implications for explaining autism. Science 310(5749):819–823
Edition F (2013) Diagnostic and statistical manual of mental disorders. Am Psychiatric Assoc 21(21):591–643
Lord C, Elsabbagh M, Baird G, Veenstra-Vanderweele J (2018) Autism spectrum disorder. The lancet 392(10146):508–520
Mohammadi MR, Ahmadi N, Khaleghi A et al (2019) Prevalence of autism and its comorbidities and the relationship with maternal psychopathology: a national population-based study. Arch Iran Med. 22(10):546–553
Althaus M, Groen Y, Wijers A, Noltes H, Tucha O, Hoekstra P (2015) Oxytocin enhances orienting to social information in a selective group of high-functioning male adults with autism spectrum disorder. Neuropsychologia 79:53–69
Guastella AJ, Einfeld SL, Gray KM, Rinehart NJ, Tonge BJ, Lambert TJ et al (2010) Intranasal oxytocin improves emotion recognition for youth with autism spectrum disorders. Biol Psychiat 67(7):692–694
Tachibana M, Kagitani-Shimono K, Mohri I, Yamamoto T, Sanefuji W, Nakamura A et al (2013) Long-term administration of intranasal oxytocin is a safe and promising therapy for early adolescent boys with autism spectrum disorders. J Child Adolesc Psychopharmacol 23(2):123–127
Kosfeld M, Heinrichs M, Zak PJ, Fischbacher U, Fehr E (2005) Oxytocin increases trust in humans. Nature 435(7042):673–676
Quattrocki E, Friston K (2014) Autism, oxytocin and interoception. Neurosci Biobehav Rev 47:410–430
Kirsch P, Esslinger C, Chen Q, Mier D, Lis S, Siddhanti S et al (2005) Oxytocin modulates neural circuitry for social cognition and fear in humans. J Neurosci 25(49):11489–11493
Carter CS, Grippo AJ, Pournajafi-Nazarloo H, Ruscio MG, Porges SW (2008) Oxytocin, vasopressin and sociality. Prog Brain Res 170:331–336
Insel TR, Fernald RD (2004) How the brain processes social. Annu Rev Neurosci 27:697–722
Guastella AJ, Mitchell PB, Dadds MR (2008) Oxytocin increases gaze to the eye region of human faces. Biol Psychiat 63(1):3–5
Andari E, Duhamel J-R, Zalla T, Herbrecht E, Leboyer M, Sirigu A (2010) Promoting social behavior with oxytocin in high-functioning autism spectrum disorders. Proc Natl Acad Sci 107(9):4389–4394
Love TM (2014) Oxytocin, motivation and the role of dopamine. Pharmacol Biochem Behav 119:49–60
Hung LW, Neuner S, Polepalli JS, Beier KT, Wright M, Walsh JJ et al (2017) Gating of social reward by oxytocin in the ventral tegmental area. Science 357(6358):1406–1411
Haber SN, Knutson B (2010) The reward circuit: linking primate anatomy and human imaging. Neuropsychopharmacology 35(1):4–26
Xiao L, Priest MF, Nasenbeny J, Lu T, Kozorovitskiy Y (2017) Biased oxytocinergic modulation of midbrain dopamine systems. Neuron 95(2):368–84.e5
Anagnostou E, Soorya L, Chaplin W, Bartz J, Halpern D, Wasserman S et al (2012) Intranasal oxytocin versus placebo in the treatment of adults with autism spectrum disorders: a randomized controlled trial. Mol Autism 3(1):16
Parker KJ, Oztan O, Libove RA, Sumiyoshi RD, Jackson LP, Karhson DS et al (2017) Intranasal oxytocin treatment for social deficits and biomarkers of response in children with autism. Proc Natl Acad Sci U S A 114(30):8119–8124
Watanabe T, Kuroda M, Kuwabara H, Aoki Y, Iwashiro N, Tatsunobu N et al (2015) Clinical and neural effects of six-week administration of oxytocin on core symptoms of autism. Brain 138(11):3400–3412
American Psychiatric Association (2013) Diagnostic and statistical manual of mental disorders, 5th edn. APA, Washington, DC
Baer DM, Wolf MM, Risley TR (1987) Some still-current dimensions of applied behavior analysis. J Appl Behav Anal 20(4):313–327
Shook GL (2005) An examination of the integrity and future of the Behavior Analyst Certification Board® credentials. Behav Modif 29(3):562–574
Fenske EC, Zalenski S, Krantz PJ, McClannahan LE (1985) Age at intervention and treatment outcome for autistic children in a comprehensive intervention program. Anal Interv Dev Disabil 5(1–2):49–58
Remington B, Hastings RP, Kovshoff H, Degli Espinosa F, Jahr E, Brown T et al (2007) Early intensive behavioral intervention: outcomes for children with autism and their parents after two years. Am J Ment Retard 112(6):418–438
Yu Q, Li E, Li L, Liang W (2020) Efficacy of interventions based on applied behavior analysis for autism spectrum disorder: a meta-analysis. Psychiatry Investig 17(5):432–443
Mansbach-Kleinfeld I, Apter A, Farbstein I, Levine SZ, Ponizovsky AM (2010) A population-based psychometric validation study of the strengths and difficulties questionnaire–Hebrew version. Front Psych 1:151
Salayev KA, Sanne B (2017) The strengths and difficulties questionnaire (SDQ) in autism spectrum disorders. Int J Disabil Hum Dev 16(3):275–280
Shahrivar Z, Tehrani-Doost M, Pakbaz B, Rezaie A, Ahmadi F (2009) Normative data and psychometric properties of the parent and teacher versions of the strengths and difficulties questionnaire (SDQ) in an Iranian community sample. J Res Med Sci 14(2):69–77
Association AP (2010) Diagnostic and statistical manual of mental disorders, text revision (DSM-IV-TR®)
Gilliam J (2006) Gilliam autism rating scale–second edition (GARS-2). Pro-Ed, Austin, TX
Ahmadi S, Safari T, Hemmatian M, Khalili Z (2011) The psychometric properties of Gilliam autism rating scale (GARS). Res Cogn Behav Sci 1(1):87–104
Hollander E, Novotny S, Hanratty M, Yaffe R, DeCaria CM, Aronowitz BR et al (2003) Oxytocin infusion reduces repetitive behaviors in adults with autistic and Asperger’s disorders. Neuropsychopharmacology 28(1):193–198
Yatawara C, Einfeld S, Hickie I, Davenport T, Guastella A (2016) The effect of oxytocin nasal spray on social interaction deficits observed in young children with autism: a randomized clinical crossover trial. Mol Psychiatry 21(9):1225–1231
Dadds MR, MacDonald E, Cauchi A, Williams K, Levy F, Brennan J (2014) Nasal oxytocin for social deficits in childhood autism: a randomized controlled trial. J Autism Dev Disord 44(3):521–531
Guastella AJ, Gray KM, Rinehart NJ, Alvares GA, Tonge BJ, Hickie IB et al (2015) The effects of a course of intranasal oxytocin on social behaviors in youth diagnosed with autism spectrum disorders: a randomized controlled trial. J Child Psychol Psychiatry 56(4):444–452
Parker KJ, Oztan O, Libove RA, Sumiyoshi RD, Jackson LP, Karhson DS et al (2017) Intranasal oxytocin treatment for social deficits and biomarkers of response in children with autism. Proc Natl Acad Sci 114(30):8119–8124
Kruppa JA, Gossen A, Oberwelland Weiß E, Kohls G, Großheinrich N, Cholemkery H et al (2019) Neural modulation of social reinforcement learning by intranasal oxytocin in male adults with high-functioning autism spectrum disorder: a randomized trial. Neuropsychopharmacology 44(4):749–756
Acknowledgements
The authors would like to express gratitude to the study staff at the Isfahan, Iran, Autism Center and the study participants and their families.
Funding
None of the authors has any financial disclosures.
Author information
Authors and Affiliations
Contributions
AK, concept and design, formal analysis, data collection, drafting and working, revising and editing. SSHI, concept and design, formal analysis, data collection, drafting and working, revising and editing. MRM, concept and design, formal analysis, data collection, drafting and working, revising and editing. AMS, concept and design, formal analysis, data collection, drafting and working, revising and editing. The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study protocol was approved by the Isfahan University of Medical Sciences Ethics Committee (IR.MUI.MED.REC.1400.442) and the Iranian registration of clinical trials (IRCT20211004052670N1). The parent or legal guardian of each participant provided written informed permission for their involvement in the trial, and, where necessary, participants’ agreement was also acquired. The modified Declaration of Helsinki regulations were followed throughout the experiment. The trial was free of any commercial interference.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Karbasi, A., Shafiezadegan Isfahani, S., Maracy, M.R. et al. Effect of intranasal oxytocin combination therapy with applied behavior analysis on social impairments in pediatric’s children with autism spectrum disorder. Middle East Curr Psychiatry 30, 35 (2023). https://doi.org/10.1186/s43045-023-00300-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43045-023-00300-w