Abstract
Background
Red cell distribution width (RDW) measures the extent of variation in red blood cell (RBC) volume in terms of coefficient of variation. It reflects the degree of variation in RBC’s sizes and shapes, characteristic of iron deficiency and anemias involving RBC destruction, especially hemoglobinopathies. Its values are often available as one of the RBC indices generated as complete blood cell count (CBC) using automated hematology analyzers. Hemoglobinopathies are highly prevalent in malaria-endemic geographical settings like the Sub-Saharan African which has over 200,000 currently documented annual major hemoglobinopathies with an alarming mortality rate of 50–90% by the age of 5 years usually undiagnosed. With a vast growing majority of hemoglobinopathy carriers, this public health problem is projected to escalate by the year 2050 due to unaffordable laboratory tests for screening of newborns and populations as recommended by World Health Organization in resource-limited settings. Therefore, innovative of a cost-effective diagnostic method would improve the survival of these children. The current study aimed to evaluate the overall ability of RDW in discriminating hemoglobinopathy and hemoglobinopathy-free cases within the Lake Victoria Economic Block region of Western Kenya served partly by the Aga Khan Hospital, Kisumu.
Objective
To determine the significance of RDW as a tool to differentiate between individuals with hemoglobinopathies and those without.
Method
This was a cross-sectional retrospective comparative hospital-based study that analyzed data from the hematology laboratory database for patients examined using high-performance liquid chromatography during the years 2015–2020. The study consisted of 488 participants (49.4%, n = 241 control; 50.6% n = 247 case, p = 0.786) aged between 1 month and 66 years selected conveniently through census. The relationship between RDW of the controls and cases was analyzed using Mann–Whitney U, Kruskal–Wallis tests among population groups and Dunn’s post hoc test within groups since the data were non-normally distributed.
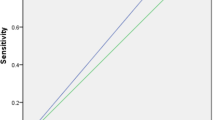
Results
The RDW cutoff value was computed at 95% confidence interval (CI), and values greater than this indicated a diagnosis of hemoglobinopathy.
Conclusion
RDW at 95% CI was 19.9 [14.5 + (2.7 × 2 = 19.9)] cutoff point which proved to be an excellent screening tool for sickle cell disease phenotypes in Western Kenya but would generate many false positive and false negatives for pure Hb AS. RDW is a poor screening tool for, Hb AS + HbF, Hb AS + β thal and β-thalassemia since it could not differentiate diseased from non-diseases populations. Even though RDW proved to be a poor screening tool for beta thalassemia, other complete blood count (CBC) parameters such as MCV and red cell count can be used to identify thalassemia syndromes as well as iron deficiency anemia. Though out of the scope of this work, highlighting the significance of these parameters in addition to the RDW would improve its feasibility as a screening tool for all hemoglobinopathies. Normal reference range for children ≤ 5 years needs to be developed using prospective data for precise marking of disorders associated with red cell anisocytosis, and individuals ≥ 6 years can share RDW normal reference range regardless of their gender.
Similar content being viewed by others
Introduction
A readily measured hemoglobinopathy biomarker enabling affordable detection of the condition in resource-limited settings is urgently needed. Hemoglobinopathies are hereditary disorders of hemoglobin, associated with often fatal anemia [1]. They are an increasing but neglected global public health problem that needs urgent attention of the global community [2,3,4]. Studies estimate that 7% of the global population carries an inherited Hb disorder gene and about 300,000 infants are born with severe forms of hemoglobin (Hb) disorders with 200,000 being born in sub-Saharan Africa annually with a high mortality rate of 50–80% by the age of 5 years [5, 6]. Majority of those who survive 5 years without diagnosis live unproductive lives due to painful crises and anemia resulting from hemolysis and vaso-occlusive crisis triggered by infections [7] which would have been avoided by early diagnosis leading to proper palliative care that would in turn improve the quality of life. However, with a vast growing majority of hemoglobinopathy carriers who have 25% risk of passing a potentially severe disorder to offspring, this public health problem is projected to escalate by the year 2050, with over 14 million births each year with major Hb disorders where 82% will come from these African countries [8].
In Kenya, research reports spanning several years indicate that the burden of hemoglobinopathies is significantly higher in malaria holo-endemic regions that include Western Kenya and coastal region [9]. A review of these studies documented a prevalence of 18.7% for HbS (HbAS 17.1% and HbSS 1.6%) and 48.1% for α-thalassemia (heterozygous 38.5% and homozygous 9.6%) in Western Kenya [10] and in a hemoglobinopathy survey done in Kombewa, Kisumu County, published an overall HbS prevalence of 19.9% (HbAS 19.0% and HbSS 0.9%) and 53.2% for α-thalassemia (heterozygous 44.4% and homozygous 8.8%) hemoglobinopathies [11]. Another population Kenya survey of children, conducted in Kilifi County, reported prevalence of 0.8% for sickle cell disease (HbSS heterozygotes 7.8% and HbSS homozygotes 92.2%) plus 65.5% for α-thalassemia (heterozygous 48.6% and homozygous 16.9%) [7]. A HbS prevalence of 31.8% (HbAS 20.7% and HbSS 11.1%) was also reported in a hospital-based study of cases of acute plasmodium falciparum malaria resident in Kisumu County, Western Kenya [12]. Concordant with these reports, a population study of children in rural areas of Kakamega, Bungoma and Vihiga counties, reported an HbS prevalence of 16.4% (HbAS 16.2%; HbSS 0.2%) plus 48.2%, α-thalassemia (heterozygous 40% and homozygous 8.2%) [13]. These reports of high prevalence of hemoglobinopathies in Kenya (Table 1) underscore an urgent need for laboratory methods that are accessible, to enable easy and early detection of hemoglobinopathies. This will help improve management of those Hb disorders and minimize transmission by asymptomatic carriers, as recommended by WHO as one of the key diagnostic interventions that form part of the maternal and child health care (MCHC) services [14]. However, many Sub-Saharan Africa countries including Kenya have not implemented newborn and population screening, due to the high cost of accurate laboratory technologies with good turnaround time [5, 9, 14].
Red cell distribution width (RDW) is potentially a suitable hemoglobinopathy biomarker enabling laboratory detection of the Hb disorders for resource poor settings, like Kenya. That is because of the easy and ready availability of its assay results as one of the hematological indices generated by automated hematology analyzers as part of the complete blood count (CBC) [15]. Derangement of RDW values has been reported widely in diseases involving red cell destruction and is a biomarker of disease severity in patients who are critically ill; it is also an independent predictor of all-cause mortality in sepsis and congestive heart failure [16,17,18,19]. Mathematically, it is the coefficient of variation (CV) of the mean corpuscular (cell) volume (MCV), i.e., RDW = 1SD/MCV × 100% [17]. Several empirical studies have demonstrated significant elevation in RDW values in the presence of sickle cell and thalassemia disorders and the potential of this hematological parameter to distinguish hemoglobinopathy cases from other hematological disorders. Some of these investigated uses of RDW to distinguish thalassemia from iron deficiency anemia [20,21,22,23,24,25], while others demonstrate the potential of RDW to serve as laboratory biomarkers for discriminating bearers of sickle cell Hb (HbSS and HbAS) and thalassemia from those with other hematological disorders [26, 27]. The currently documented normal value for RDW (CV) is 11–14.5% [13]. Despite the apparent potential of this hematological index as a diagnostic marker for hemoglobinopathies, the literature reviewed reports no previous rigorous evaluation of its utility for this purpose in Kenya and indeed Africa. Owing to the reported variation in biological characteristics between human populations in different geographical locations due to the impact of physical and sociocultural environment on the expression of genes for various phenotypic characteristics, it is uncertain as to whether the findings of these studies are generalizable to Kenya [1, 8, 28]. Besides, even in these studies, the utility of RDW as a hemoglobinopathy diagnostic biomarker has not been rigorously and formally evaluated. There is a need therefore to determine empirically the ability of RDW to discriminate hemoglobinopathy and hemoglobinopathy-free individuals in Kenyan population.
Material and methods
Patients and specimens
This was a hospital-based cross-sectional retrospective comparative study of 488 conveniently selected through census from HPLC-confirmed hemoglobinopathy subjects (cases) (n = 247, 50.6%) and hemoglobinopathy-free and non-anemic (control group) (n = 241, 49.4%) results with corresponding complete blood counts from Aga Khan Hospital, Kisumu, and its Western Kenya satellites for the past 5 years from 2015 to 2020. The subjects excluded from the study were those HPLC results that lacked their respective complete blood counts, those confirmed to have leukemia, those transfused in the past 3 months, those confirmed to have iron deficiency anemia, and those that were tested for blood cultures and antinuclear antibodies (ANA).
The control group comprised of presumed normal healthy individuals who were free from hemoglobinopathies and other erythrocytic disorders known to affect RDW values. These were age-mixed people stratified into three age sets confirmed using HPLC to have normal Hb (Hb AA) whose Hb concentrations of ≥ 9.5 g/dl for ≤ 5-year-olds, ≥ 10.5 g/dl for ≤ 12-year-olds and ≥ 11 g/dl for ≥ 13-year-olds were selected to rule out iron deficiency anemia according to documented selection criteria [29]. Both cases and control group had their respective RDW generated as part of full hemogram output.
To ensure accurate and reliable patients results, equipment calibrations are properly monitored using daily internal quality controls (IQC) and monthly external quality assurance (EQA); therefore, owing to sustained quality, the Aga Khan Hospital, Kisumu Laboratory, has attained ISO 9001:2015 certification, ISO 15189:2012 accreditation and is at advanced stage of attaining Joint Commission International Accreditation.
Sample size determination
The sample size was calculated using Cochran’s formula which was suggested by a previous study as the effective formula for calculation of case–control and other comparative studies [30]. A vaccine trial study done in Kombewa Kisumu County gave 19% prevalence of thalassemia and sickle cell which generated a P value of 0.19. On employing 95% confidence interval and a precision of 5%, a sample size of 237 was therefore obtained; thus, a minimum of 474 study subject was required since the present study was a two-arm study (case–control) [11].
Statistical analysis
Data were analyzed using the Statistical Package for Social Sciences (SPSS) version 23, where hemoglobinopathy profiles were summarized as frequencies, proportions and percentages, compared between groups as proportions using chi-square and analyzed variations across population groups using Pearson’s chi-square of association. Values for RDW for the hemoglobinopathy-free (control) group were non-normally distributed as revealed by Kolmogorov–Smirnov and Shapiro–Wilks, and so the median and interquartile range (IQR) were used as descriptive statistics to derive the normal reference or cutoff value for hemoglobinopathy diagnosis as recommended [31]. The inference relationship across variables, Mann–Whitney U and Kruskal–Wallis tests were used with Dunn post hoc test being applied within groups. By comparing the RDW values of the hemoglobinopathy cases with the normal control group, its significance difference (p < 0.05) of this hematological index as a hemoglobinopathy discriminant was computed.
Results
Demographic characteristics of the study subjects
The study involved a total of 488 study subjects consisting of basically groups (cases, n = 247, 50.6% and a control group, n = 241, 49.4%), p = 0.786. The proportions of females and males did not differ significantly (56.1%, n = 274; 43.9%, n = 214, p = 0.502). There was a significant difference in (p < 0.0001) proportions of subjects from Aga Khan Hospital sites with Kisumu having the largest (49.0%, n = 239), followed by Busia (15.4%, n = 75) and then Homa Bay (12.3%, n = 60), while the rest contributed the remainder in small proportions. The proportions of subjects in the three age-groups varied significantly (p < 0.0001): ≤ 5-year-olds, 42.4%, n = 207; ≤ 12-year-olds, 19.9%, n = 97; and ≥ 13-year-olds, 37.7%, n = 184. These results are shown in Table 2.
The overall red cell distribution width in study groups, gender and age
The overall median RDW for the control group was 14.5 (IQR = 2.7) and was significantly lower than for the case group, with a median of 20.7 (IQR = 8.3) (p < 0.0001). The overall RDW for the study subjects was not significantly different between males, median 17.1 (IQR = 8.0) and females, median 15.5 (IQR = 6.7), p = 0.317. Similarly, for the control group there was no significant difference in median RDW between males 14.55 (IQR = 1.90) and females 14.2 (IQR = 2.40), p = 0.089. However, there was a variation in RDW with age for both the control group and cases. Thus, age ≤ 5 years had the highest median, 19.0 (IQR = 7.1), followed by a median of 15.5 (IQR = 8.2) of 6–12-year-olds, while age ≥ 13 years had the lowest median of 14.1 (IQR = 2.8), p < 0.05. For the control group again the median RDW generally varied significantly with age: ≤ 5-year-olds had the highest, 15.95 (IQR = 4.2), compared with 6–12-year-olds, 14.2 (IQR = 1.7) and ≥ 13-year-olds, 13.7 (IQR = 1.8), (p < 0.0001). See Table 3 for details.
The overall red cell distribution width in control groups
The control group of children ≤ 5 years had the highest RDW median of 15.95 (IQR = 4.2) which was significantly (p = 0.001) high compared to 14.2 (IQR = 1.7) that of 6–12 years of age-group (Table 3). The control group of those ≥ 13 years had a RDW median of 13.7 (IQR = 1.8) which was statistically (p < 0.0001) lower when compared to control group of children ≤ 5 years. There was no statistical significance (p = 0.347) of RDW median of age-group 6–12 years when compared to the age-group ≥ 13 years in their respective control groups (Table 3).
Red cell distribution width in hemoglobinopathies
The case group of age set ≥ 13 years had a median of 16.5 (IQR = 2.75) which was significantly lower (p < 0.0001) when compared to children’s cases ≤ 5 years with a median of 21.2 (IQR = 7.10) (Table 3). The age-group of 6–12 years had a RDW median of 19.9 (IQR = 7.90) in their case group and did not have statistical significance (p = 0.138) when compared to the case group of children ≤ 5 years. Similarly, there was no significant difference (p = 0.225) of RDW in the case group of age set 6–12 years when compared to RDW of case group in those individuals ≥ 13 years (Table 3).
RDW stratification on age in male control and case groups
The red cell distribution width showed statistical significance (p = 0.042) in control group of males ≤ 5 years who had a RDW median of 16.75 (IQR = 4.7) when compared to 6–12 years males control group with a median of 15.1 (IQR = 1.6). Similarly, there was a significant difference (p < 0.0001) in RDW for males control group ≤ 5 years when compared to males control group age-group ≥ 13 years who had a median of 13.7 (IQR = 1.8). However, there was no statistical significance (p = 0.137) in RDW of age-group 6–12 years when compared to the same males control group ≥ 13 years. The RDW in the case group males between the three age sets did not have statistical significance (p = 0.145). These results are summarized in Table 4.
RDW stratification based on age among female control and case group
The red cell distribution width significance in the three age sets in females followed the same trend as males with female age-group ≤ 5 years who had a median of 15.55 (IQR = 3.76) showed significant difference (p = 0.017) when compared to control group females of age 6–12 years with a median of 13.8 (IQR = 1.81). There was also a significant difference (p < 0.0001) in RDW of female control group ≤ 5 years when compared to age ≥ 13 years female control group who had a median of 13.75 (IQR = 2.22). However, there was no significant difference (p = 0.860) in RDW of 6–12 years female control group when compared to the age-group ≥ 13 years female control group. The female case group ≥ 13 years had the lowest median of 14.75 with statistical significance (p < 0.0001) when compared to ≤ 5 years and also when compared to the age set 6–12 years (p = 0.024) as shown in Table 4.
Red cell distribution width in hemoglobinopathies
The median RDW of the control group, 14.5 (IQR = 2.7), was significantly lower than for hemoglobinopathy cases combined, median 20.7 (IQR = 8.3), p < 0.0001. It was also lower compared to the various combinations of HbSS with non-HbS hemoglobinopathies, which had values: 25.4 (IQR = 5.5) for HbSS; 23.3 (IQR = 7.9) for Hb SS + β-thalassemia, and HbSS + HbF for 20.9 (IQR = 5.5) (p < 0.0001). RDW had a significance (p < 0.0001) difference in pure Hb AS with a median of 16.4 (IQR = 6.5); however, HbAS + HbF, Hb AS + β-thalassemia and β-thalassemia had high RDW medians of 24.2 (IQR = 7.4), 21.0 (IQR = 10.5) and 18.1 (IQR = 8.3), respectively, but did not have statistical significance (p > 0.05) as summarized in Table 3.
Discussion
The red cell distribution width was significantly (p < 0.0001) elevated in the overall hemoglobinopathy cases with an overall median of 20.7 (IQR = 8.3) meaning it could be used to differentiate diseased (hemoglobinopathy) from non-diseased (hemoglobinopathy-free) individuals, thus serving as a potential biomarker of hemoglobinopathies in Western Kenya. However, when hemoglobinopathies were broken into their respective phenotypes, some phenotypes had statistically significant (p < 0.0001) elevated RDW, while others did not have statistical significance. Therefore, the present study obtained RDW cutoff value of 19.9 [14.5, IQR = 2.7; 95% CI 9.1–19.9, p < 0.0001], meaning that 95% of the normal population [32] have RDW ≤ 19.9; thus, above that could be indicating a marked anisocytosis suggesting a hemoglobinopathy that needs confirmation using the gold standard tests. This cutoff value was developed from the normal controls who had RDW median of 14.5 (IQR = 2.7), which is higher compared to 11.3 documented by a previous study [33]. This explains the issue of addressing establishment of local reference values as recommended by previous studies, that clinical laboratories need to obtain their own normal ranges [34]. Variation of hematological normal ranges has been reported in many parts of Africa due to several factors that include sex, geographical location, race, altitude and diet [34, 35]. In a study done in Nakuru County, similarly, documented reduced hematological ranges with the author citing genetic, ethnic and demographic variations which she recommends regions to develop their reference ranges for better patient management [36]. In another study done in Kenya medical research institute in Kisumu, found out that use of locally established reference ranges resulted in fewer participants classified as having abnormal hematological or biochemical values compared to use of USA-derived reference intervals [37]. In a similar population-based cohort study done in Kericho, Kenya, in a potential Phase I/II HIV vaccine trial site, necessitated establishment of region-specific clinical reference ranges for trial enrollment and participant monitoring. The authors documented that use of (USA) reference range which defines anemia in African-American men and women as hemoglobin of 12.9 g/dL and 11.5 g/dL, respectively, would result into the entire Kericho population classified as anemic, leading to erroneous and unnecessary treatments [38]. To this effect, the present study developed a RDW standard cutoff value of 19.9 at 95% confidence interval calculated from the control median of 14.5 + (IQR = 2.7 × 2) as required by normal distribution curves [32].
RDW was higher in males with a median of 17.1 (IQR = 8.0) than females who had a median of 15.5 (IQR = 6.7) but did not have statistical significance (p = 0.317) between the two sexes as shown in Table 3, similar to respective control groups (p = 0.089). Similar findings are reported by Qurtom et al. that RDW showed no statistically significant difference in the mean RDW for males and females [26], consistent with results reported by Hoffmann et al. [22]. The red cell distribution width (RDW) decreased significantly as the study subjects aged (p < 0.05), starting with ≤ 5-year-olds who has the highest median, while those ≥ 13 years have the lowest RDW median (Table 3). However, the RDW for participants aged 6–12 years, like those for age ≥ 13 years, did not differ significantly (p = 0.347), irrespective of gender, from those for the respective control groups (Table4). This implies that same normal reference RDW values could apply to persons aged ≥ 6 years, but children aged < 6 years should have separate values. The reason behind high RDW in children ≤ 5 years may be due to a vigorous activity of bone marrow releasing immature RBC (reticulocytes) that are usually larger than normal red blood cells bringing about this variation of erythrocytes in children.
Red cell distribution normal range for children ≤ 5 years does not exist currently and globally despite studies showing similar findings of children < 2 years having a higher significant RDW mean as compared to the adult population [26]. It has also been noted that RDW becomes abnormal early before Hb or even MCV; thus, it is an excellent biomarker in children ≤ 5 years with anemia-related disorders [26]. The mean RDW of 13.2 ± 0.9 was reported by Qurtom et al. in individuals < 2 years old which varied slightly with our findings (control groups) of 15.95 (IQR = 4.2) of children ≤ 5 years and 14.2 (IQR = 1.7) of individuals aged 6–12 years, which could be due to variation of study designs or sociocultural epigenetic differences that affect phenotypic gene expression of biological characteristics in humans based on geographical locations [8, 28]. Another study reported a strong association between RDW and age; however, the age sets were majorly < 18 years and those > 18 years, where RDW increased with age which could be due to exposure of environmental factors or infections to these individuals as they aged [22].
The overall case group had a RDW median of 20.7 (IQR = 8.3), significantly (p < 0.0001) elevated compared to control group 14.5 (IQR = 2.7) indicating a marked anisocytosis in hemoglobinopathies. Hb SS had a RDW median of 25.4 (IQR = 5.5), the highest (p < 0.0001) among hemoglobinopathies listed by the present study with similar findings being recorded by Webster and Castro whose Hb SS had a mean of 22.4 ± 4 [39]. Hb SS + β thalassemia, was the second highest (p < 0.0001) with a RDW median of 23.3 (IQR = 7.9) while Hb SS + HbF recorded a median of 20.9 (IQR = 5.5), the lowest among Hb SS phenotypes. Similar order of decreasing magnitude of RDW was reported in anemic patients, with the highest value being seen in sickle cell anemia, sickle cell + β thalassemia, sickle cell trait, β-thalassemia and iron deficiency anemia [33]. RDW was the lowest in Hb SS + HbF due to the stability of Hb F that is known to reduce red cell anisocytosis since it does not enter HbS-polymerization phase, thus regulating clinical and hematological features of SCD [40]. In a prospective cohort study done in Kilifi area in Kenya, noted reduced morbidity and mortality in children < 5 years with Hb SS + HbF demonstrating the stability of hemoglobin F in resisting hemolysis [7]. In a study done in Kisumu County to differentiate malaria in SCD using hematological parameters, documented RDW of 14.9 (3.3) in HbSS phenotypes contrasts our finding of 25.4 (IQR = 5.45) in Hb SS, 20.85 (IQR = 5.47) in HbSS + HbF and 23.3(IQR = 7.9) in HbSS + β-thalassemia. This reduced RDW in that study could be associated with sample size error, analysis error or equipment used in the study since anisocytosis is inevitable in Hb SS phenotypes based on previous studies [12, 26, 33, 39].
Pure HbAS recorded a RDW median of 16.4 (IQR = 6.5) which was the lowest among hemoglobin disorders investigated by the present study. Though significantly elevated (p < 0.0001), RDW would generate many false positive results if used as a screening tool for SCT since its median was within the standard cutoff value of 19.9. Similar findings are documented by studies showing SCT patients having normal RDW, which makes it difficult to use this parameter to distinguish diseased (SCT) from the healthy population [41].
HbAS + HbF and HbAS + β thalassemia had medians of 24.15 (IQR = 7.43) and 20.9 (IQR = 10.5), respectively, which were high compared to the control group but, when subjected under statistical test, did not have statistical significance (p = 0.449, p = 0.791, respectively), suggesting that small sample size could have resulted into an abnormally high RDW. Similarly, there was no statistical significance (p = 1.0) between RDW of pure β-thalassemia compared to the control group with similar information being documented by previous studies that RDW cannot be used to discriminate β-thalassemia from β-thalassemia-free population [26].
Conclusion
Red cell distribution width at 95% C.I was 19.9 [14.5 + (2.7 × 2 = 19.9)] cutoff point which proved to be an excellent screening tool for sickle cell disease (SCD) phenotypes in Western Kenya but would generate many false positive and false negative results for pure HbAS. RDW is a poor screening tool for HbAS + HbF, HbAS + β thal and β-thalassemia since it could not differentiate diseased from non-diseases population. Even though RDW proved to be a poor screening tool for beta thalassemia, other CBC parameters such as MCV and red cell count can be used to identify thalassemia syndromes as well as iron deficiency. Though out of the scope of this work, highlighting the significance of these parameters in addition to the RDW would improve its feasibility as a screening tool for all hemoglobinopathies. Normal reference range for children ≤ 5 years needs to be developed using prospective data for precise marking of disorders associated with red cell anisocytosis and individuals ≥ 6 years can share RDW normal reference range regardless of their gender.
Availability of data and materials
Data will be made available if needed.
Abbreviations
- WHO:
-
World Health Organization
- RDW:
-
Red cell distribution width
- HPLC:
-
High-performance liquid chromatography
- C.I:
-
Confidence interval
- SCD:
-
Sickle cell disease
- CBC:
-
Complete blood count
- MCV:
-
Mean corpuscular volume
- Hb:
-
Hemoglobin
- CV:
-
Coefficient of variation
- SPSS:
-
Statistical Package Social Sciences
- IQR:
-
Interquartile range
- USA:
-
United States of America
- Hb F:
-
Hemoglobin F genotype
- Hb S:
-
Hemoglobin S genotype
- SCT:
-
Sickle cell trait
- RBC:
-
Red blood cell
- HIV:
-
Human immunodeficiency virus
- RDW-CV:
-
Red cell distribution width-coefficient of variation
- MCHC:
-
Maternal and child health care
- HbSS:
-
Hemoglobin SS genotype
- HbAS:
-
Hemoglobin AS genotype
- SD:
-
Standard deviation
- Hb AA:
-
Hemoglobin AA genotype
- Hb:
-
Hemoglobin
- β:
-
Beta
- ANA:
-
Antinuclear antibodies
- IQC:
-
Internal quality control
- EQA:
-
External quality assurance
- SPSS:
-
Statistical Package for Social Sciences
References
Mutua BM, Sowayi G, Okoth P (2022) Red cell distribution width as a surrogate marker of haemoglobinopathies in western Kenya. Afr J Lab Med 11:1. https://doi.org/10.4102/ajlm.v11i1.1644
Weatherall D (2011) The inherited disorders of haemoglobin: an increasingly neglected global health burden. Indian J Med Res 134(4):493
Chakravorty S, Williams TN (2015) Sickle cell disease: a neglected chronic disease of increasing global health importance. Arch Dis Child 100(1):48–53
Modell B, Darlison M (2008) Global epidemiology of haemoglobin disorders and derived service indicators. Bull World Health Organ 86:480–487
Arishi WA, Alhadrami HA (2021) Techniques for the detection of sickle cell disease: a review. Micromachines 12(5):519
Piety NZ et al (2016) Validation of a low-cost paper-based screening test for sickle cell anemia. PLoS ONE 11(1):e0144901
Uyoga S et al (2019) The epidemiology of sickle cell disease in children recruited in infancy in Kilifi, Kenya: a prospective cohort study. Lancet Glob Health 7(10):e1458–e1466
Mutua B, Sowayi G, Okoth P (2022) Distribution of hemoglobinopathy phenotypes in western Kenya: a retrospective study done at Aga Khan Hospital, Kisumu. Egypt J Intern Med 34(1):1–9
Kosiyo P, Otieno W, Gitaka J, Munde EO, Ouma C (2021) Haematological abnormalities in children with sickle cell disease and non-severe malaria infection in western Kenya 1–11
Suchdev PS et al (2014) The burden and consequences of inherited blood disorders among young children in western Kenya. Matern Child Nutr 10(1):135–144
Kifude CM (2007) Prevalence of sickle cell and α-thalassemia traits in children enrolled in a malaria vaccine clinical trial, in Kombewa, Western Kenya. Diss. Kenyatta University
Kosiyo P et al (2020) Association between haematological parameters and sickle cell genotypes in children with Plasmodium falciparum malaria resident in Kisumu County in Western Kenya. BMC Infect Dis 20(1):1–11
Byrd et al (2019) A behaviour change intervention with lipid‐based nutrient supplements had little impact on young child feeding indicators in rural Kenya. Matern Child Nutr 15(1):e12660.
Tluway F, Makani J (2017) Sickle cell disease in Africa: an overview of the integrated approach to health, research, education and advocacy in Tanzania, 2004–2016. Br J Haematol 177(6):919–929
Willard MD, Tvedten H (2011) Small animal clinical diagnosis by laboratory methods. Elsevier Health Sciences, Hoboken
Ramby AL et al (2015) Red blood cell distribution width as a pragmatic marker for outcome in pediatric critical illness. PLoS ONE 10(6):e0129258
Titcomb CP (2017) Red cell distribution width (RDW): an under appreciated marker for increased mortality. On Risk 33(1):30–46
Jandial A et al (2017) Elevated red cell distribution width as a prognostic marker in severe sepsis: a prospective observational study. Indian J Crit Care Med 21(9):552
Kaori M, Litao S, Kamat D. Back to basics red blood cell distribution width
Vehapoglu A et al (2014) Hematological indices for differential diagnosis of Beta thalassemia trait and iron deficiency anemia. Anemia 2014
Al-Numan AH, Al-Obeidi RA (2021) The value of the red cell distribution width index versus other parameters in the differentiation between iron deficiency anemia and beta thalassemia trait among children in Mosul, Iraq. Expert Rev Hematol 14(4):401–406
Hoffmann JJML, Nabbe KCAM, van den Broek NMA (2015) Effect of age and gender on reference intervals of red blood cell distribution width (RDW) and mean red cell volume (MCV). Clin Chem Lab Med (CCLM) 53(12)
Song B et al (2020) Utility of red cell distribution width as a diagnostic and prognostic marker in non-small cell lung cancer. Sci Rep 10(1):1–7
Jahangiri M, Rahim F, Malehi AS (2019) Diagnostic performance of hematological discrimination indices to discriminate between βeta thalassemia trait and iron deficiency anemia and using cluster analysis: introducing two new indices tested in Iranian population. Sci Rep 9(1):1–13
Wickramaratne KAC, Wijewickrama DC (2021) Screening for beta-thalassemia trait; applicability of red cell indices and parameters: a study in Sri Lanka. Int J Health Sci 15(1):29
Qurtom HA et al (1989) The value of red cell distribution width in the diagnosis of anaemia in children. Eur J Pediatr 148(8):745–748
Thame M et al (1991) The red cell distribution width in sickle cell disease—is it of clinical value? Clin Lab Haematol 13(3):229–237
Boyce WT, Sokolowski MB, Robinson GE (2020) Genes and environments, development and time. Proc Natl Acad Sci 117(38):23235–23241
Wacholder S et al (1992) Selection of controls in case–control studies: I. Principles. Am J Epidemiol 135(9):1019–1028
Nam J (1992) Sample size determination for case–control studies and the comparison of stratified and unstratified analyses. Biometrics 389–395
Nahm FS (2016) Nonparametric statistical tests for the continuous data: the basic concept and the practical use. Korean J Anesthesiol 69(1):8
Lee DK, In J, Lee S (2015) Standard deviation and standard error of the mean. Korean J Anesthesiol 68(3):220
Roberts GT, Badawi SBEL (1985) Red blood cell distribution width index in some hematologic diseases. Am J Clin Pathol 83(2):222–226
Lugada ES et al (2004) Population-based hematologic and immunologic reference values for a healthy Ugandan population. Clin Vaccine Immunol 11(1):29–34
Karita E et al (2009) CLSI-derived hematology and biochemistry reference intervals for healthy adults in eastern and southern Africa. PLoS ONE 4(2):e4401
Gachie NRN (2018) Haematological reference intervals for adolescents and adults in Nakuru County, Kenya (doctoral dissertation, department of pathology a thesis submitted for the award of the degree of Doctor of Philosophy (Cell haematology) in the school of medicine, Kenyatta University)
Odhiambo C et al (2015) Evaluation of locally established reference intervals for hematology and biochemistry parameters in Western Kenya. PLoS ONE 10(4):e0123140
Kibaya RS et al (2008) Reference ranges for the clinical laboratory derived from a rural population in Kericho, Kenya. PLoS ONE 3(10):e3327
Webster PAUL, Castro OSWALDO (1986) Red cell distribution width in sickle cell disease. Ann Clin Lab Sci 16(4):274–277
Damanhouri GA et al (2015) Clinical biomarkers in sickle cell disease. Saudi J Biol Sci 22(1):24–31
Olujohungbe A, Haem D, Garvey B (1993) Red cell distribution width (RDW) in sickle cell disease. Clin Lab Haematol 15(1):72–73
Acknowledgements
We would like the thank Mr. Raphael Kitonga for allowing us to use his home-based library and all is accessories in addition to moral support. We appreciate the Aga Khan Hospital, Kisumu Laboratory manager Lucy Mathenge and Dr. Simon Onsongo Head of Pathology Department.
Funding
No funding.
Author information
Authors and Affiliations
Contributions
BM conceptualized the study and wrote the original manuscript. GS conceptualized the study and reviewed and corrected the manuscript. PO supervised and reviewed the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by Masinde Muliro University Ethics Review Committee and by National Commission of Science and Technology (NACOSTI). Permit to collect data was also granted by Aga Khan Hospital, Kisumu Ethics and Research Review Board.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mutua, B., Sowayi, G. & Okoth, P. Prognostic Potential of RDW in Discriminating Hemoglobinopathies among Patients reporting to Aga Khan Hospital, Kisumu. Egypt J Med Hum Genet 23, 121 (2022). https://doi.org/10.1186/s43042-022-00334-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43042-022-00334-5