Abstract
Background
Advanced biological techniques have helped produce more insightful findings on the genetic etiology of infertility that may lead to better management of the condition. This review provides an update on genes predisposing to syndromic and nonsyndromic infertility.
Main body
The review identified 65 genes linked with infertility and infertility-related disorders. These genes regulate fertility. However, mutational loss of the functions of the genes predisposes to infertility. Twenty-three (23) genes representing 35% were linked with syndromic infertility, while 42 genes (65%) cause nonsyndromic infertility. Of the 42 nonsyndromic genes, 26 predispose to spermatogenic failure and sperm morphological abnormalities, 11 cause ovarian failures, and 5 cause sex reversal and puberty delay. Overall, 31 genes (48%) predispose to male infertility, 15 genes (23%) cause female infertility, and 19 genes (29%) predispose to both. The common feature of male infertility was spermatogenic failure and sperm morphology abnormalities, while ovarian failure has been the most frequently reported among infertile females. The mechanisms leading to these pathologies are gene-specific, which, if targeted in the affected, may lead to improved treatment.
Conclusions
Mutational loss of the functions of some genes involved in the development and maintenance of fertility may predispose to syndromic or nonsyndromic infertility via gene-specific mechanisms. A treatment procedure that targets the affected gene(s) in individuals expressing infertility may lead to improved treatment.
Similar content being viewed by others
Background
Infertility is generally defined as the inability of an organism to reproduce naturally. In humans, it is complex and defined as the failure to conceive after a year of regular and unprotected sexual intercourse [1]. Infertility affects about 48.5 million couples, representing 15% of couples worldwide [2]. Males are responsible for 20–30% of infertility, while females account for 20–35%, and the remaining is shared by both [2, 3]. However, the prevalence of infertility varies worldwide, being highest in South East Asia and West Africa [4, 5].
Infertility causes psychological, economic, and health burdens, resulting in trauma and stress, particularly in societies that emphasize childbearing [6]. In some parts of the world such as Africa and Asia, infertile couples, particularly women, face stigmatization, discrimination, and divorce. A variety of pathologies are suspected in infertility, which includes endocrine dysfunction, genetic abnormalities, infection and diseases, and autoimmune disorders [7, 8]. These pathologies are triggered by environmental factors, including toxic substance exposure as well as lifestyles, such as delayed marriage, nutrition, obesity, stress, smoking, drug use, and alcohol consumption [9]. An in-depth understanding of these mentioned causes is necessary for the prevention and effective treatment of infertility [7]. The genetic causes, in particular, need more attention and understanding because it accounts for 15–30% of male infertility alone [10, 11]. Fortunately, in the last few decades, technological innovations in biological studies have made possible more insightful findings on the genetic etiology of infertility that may lead to better treatment. This review, therefore, provides an update on genetics and pathophysiology of syndromic and nonsyndromic infertility.
Main text
Database searching and search strategy
To identify relevant papers on the topic, academic databases such as PubMed, Google Scholar, Uniport, GeneCards, Genetics Home Reference (GHR), and National Center for Biotechnology Information (NCBI) were searched. Key search words used include ‘infertility’, ‘male infertility’, ‘female infertility’, ‘etiology of infertility’, and ‘causes of infertility’. Others are ‘genetic etiology of infertility’, ‘gene mutations predisposing to infertility’, ‘syndromic and nonsyndromic infertility’, and ‘gene mutations causing infertility’. Each database was searched independently, after which the articles retrieved were pooled together and double citations removed.
Inclusion and exclusion criteria
Articles were included if they are available in the English language, focused on infertility, genetic etiology of infertility, and pathophysiology of infertility. Studies published before the year 2000 were excluded, except sometimes in which the information was vital. This was done to ensure up-to-date information.
A total of 133 articles were identified from all the databases, of which 120 were retained after removing duplicates (Fig. 1). Of the 120 articles retained, 110 passed the relevance test for eligibility. From the eligibility test, 101 articles fit the study objectives and were reviewed and included in this study.
Genes predisposing to syndromic and nonsyndromic infertility
The searches identified several gene mutations linked with infertility and infertility-related disorders and syndromes. However, it is beyond this study to discuss all the genes. As such, 65 genes frequently encountered in our searches and with sufficient information were included in this study. The genes were classified into genes predisposing to syndromic infertility, genes predisposing to nonsyndromic spermatogenic failure and sperm morphology abnormalities, genes predisposing to nonsyndromic sex reversal and pubertal delay, and genes predisposing to nonsyndromic ovarian failure.
Genes predisposing to syndromic infertility
Twenty-three (23) genes, representing 35% of the total genes collected, were linked with syndromic infertility (Table 1). The most common syndromes associated with infertility identified by this study are polycystic ovary syndrome (PCOS), Swyer syndrome, and Sertoli cell-only syndrome, respectively. Others include the congenital bilateral absence of the vas deferens (CBAVD), Wilm’s tumour, fibroid, Kallmann syndrome, Frasier syndrome, Denys-Drash syndrome, and Bordet-Biedl syndrome. Most of the genes cause female infertility with features such as hypogonadotropic hypogonadism, ovarian failure, sex reversal, gonad underdevelopment, puberty delay, and menstrual disorders. Some genes also predispose to male infertility with phenotypic presentations, including hypogonadotropic hypogonadism, sex reversal, puberty delay or absence, gonad underdevelopment, and spermatogenic failure.
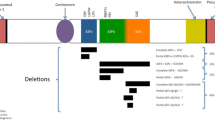
Genes predisposing to nonsyndromic spermatogenic failure and sperm morphology abnormalities
Twenty-six (26) genes, representing 40% of the total genes collected, predispose to nonsyndromic spermatogenic failure and sperm morphology abnormalities (Table 2). Most often, mutations in the genes cause meiotic arrest, resulting in acrosome malformation or absence, ultimately ending in sperm head abnormalities such as azoospermia, globozoospermia, oligospermia, and oligozoospermia. In some cases, the meiotic arrest may result in polyploidy spermatozoa, characterized by an enlarged sperm cell head called macrozoospermia. A meiotic arrest may also decrease sperm motility and hyperactivation needed to push spermatozoa through the uterus. Sometimes, mutations in the genes may cause chromatin damage or DNA fragmentation, disrupting spermatogenesis and causing sperm cell structural defects and loss.
Genes predisposing to nonsyndromic sex reversal and pubertal delay
Five (5) of the genes collected, representing 7.69% of the total genes, predispose to sex reversal and puberty delay or absence (Table 3). Most mutations in the genes cause reduced circulating levels of gonadotropins and testosterone, resulting in hypogonadotropic hypogonadism, characterized by the absence or incomplete sexual maturation. Mutations in the genes may also cause complete or partial gonadal dysgenesis, characterized by underdeveloped or presence of both gonads.
Genes predisposing to nonsyndromic ovarian failure
Eleven (11) of the genes collected, representing 16.92% of the total genes, predispose to nonsyndromic ovarian failure (Table 4). Some mutations in the genes may reduce the sensitivity of fully grown immature oocytes to progestin hormone, resulting in a reduced number of oocytes undergoing meiotic maturation. Mutations in the genes may also cause ovarian dysgenesis, characterized by absence or puberty delay, primary amenorrhea, uterine hypoplasia, and hypogonadotropic hypogonadism. Some mutations prevent the formation of primordial follicles, resulting in reduced oocyte numbers after birth.
In summary, 23 genes, representing 35%, were linked with syndromic infertility, while 42 genes, accounting for 65% cause nonsyndromic infertility. Of the 42 nonsyndromic genes, 26 predispose to spermatogenic failure and sperm morphology abnormalities, 11 cause ovarian failures, and 5 cause sex reversal and puberty delay. Overall, 31 genes (48%) predispose to male infertility, 15 genes (23%) cause female infertility, and 19 genes (29%) predispose to both. The common features of male infertility were spermatogenic failure and sperm morphology abnormalities, while ovarian failure has been the most frequently reported among infertile females. This analysis infers that male genetic infertility was more prevalent than female, with spermatogenic failure and sperm morphology abnormalities being most prevalent.
Genetic testing for infertility disorders
Knowing the exact cause of infertility allows for better diagnostic decisions and enables enhanced counseling for parents with regard to risks to their children. For this reason, when there is a means, testing of embryos should be recommended for a family with a history of genetic infertility disorders discussed above. Moreover, every healthy-looking individual is a carrier of between 5 to 8 recessive genetic disorders; so the test should be extended to everyone who has the means [157]. It is specifically recommended for embryos of couples who are recessive for a gene infertility disorder.
The conventional method used in genetic testing of embryos is the whole sequence amplification. After fertilization, the embryo undergoes mitotic divisions for 5 to 7 days, ending with the development of the blastocyst stage. A biopsy of some blastocysts is done, after which a whole genome amplification of the cells is conducted, usually using polymerase chain reaction [157, 158]. This technique is laborious, time-consuming, and expensive, so recently, a new technique known as the next-generation sequencing is being used for testing genetic disorders in infertile couples and embryos [159]. The protocol is based on an enlarged panel of disease-associated genes (approximately 5000 genes). The large panel of marker genes allows the identifications of a large number of target and non-target genes [157]. However, the technique has some limitations too, which is its inability to detect haploidies, polyploidies, and mosaicisms [157].
Conclusion
Several studies reviewed showed that certain genes embedded in the hypothalamus, pituitary gland, gonads, and gonadal outflow regulate fertility in both males and females. However, mutational inactivation of these genes may cause syndromic or nonsyndromic infertility. The common features of male infertility include spermatogenic failure, resulting in azoospermia, oligospermia, and chromosome structural abnormalities. Most females express ovarian failure, resulting in menstrual dysfunction and pregnancy loss. Males and females may also express sex reversal, pubertal delay or absence, and genital abnormalities such as micro-penis and absence of the breast. Male genetic infertility was more prevalent than female, with spermatogenic failure and sperm morphology abnormalities being most prevalent. The mechanisms leading to these pathologies are gene-specific, which, if targeted in the affected, may lead to improved treatment. Medical practitioners are advised to target these genes in the affected.
Availability of data and materials
Not applicable.
Abbreviations
- AIS:
-
Androgen insufficiency syndrome
- BBS:
-
Bordet-Biedl syndrome
- CBAVD:
-
Congenital bilateral absence of the vas deferens
- CF:
-
Cystic fibrosis
- FSH:
-
Follicle-stimulating hormone
- FXPOI:
-
Fragile X-associated primary ovarian insufficiency
- GHR:
-
Genetic home reference
- HH:
-
Hypogonadotropic hypogonadism
- LH:
-
Luteinizing hormone
- NCBI:
-
National Center for Biotechnology Information
- OHSS:
-
Ovarian hyperstimulation syndrome
- ODG:
-
Ovarian dysgenesis
- PCOS:
-
Polycystic ovary syndrome
- POF:
-
Premature ovarian failure
- SCOS:
-
Sertoli cell-only
- SNP:
-
Single nucleotide polymorphism
- SPGF:
-
Spermatogenic failure
References
Venkatesh T, Suresh PS, Tsutsumi R (2014) New insights into the genetic basis of infertility. Appl Clin Genet. 7:235–243. https://doi.org/10.2147/TACG.S40809
Agarwal A, Mulgund A, Hamada,A, et al. A unique view on male infertility around the globe. Reprod Biol Endocrinol. 2015; 13: 37 https://doi.org/10.1186/s12958-015-0032-1.
Chowdhury SH, Cozma AI, Chowdhury JH. Infertility. Essentials for the Canadian Medical Licensing Exam: review and prep for MCCQE Part I. 2nd edition. Wolters Kluwer. Hong Kong. 2017.
Mascarenhas MN, Flaxman SR, Boerma T et al (2012) National, regional, and global trends in infertility prevalence since 1990: a systematic analysis of 277 health surveys. PLoS Med. 9:e1001356 https://dx.plos.org/10.1371
Odunvbun W, Oziga D, Oyeye L, Ojeogwu C (2018) Pattern of infertility among infertile couple in a secondary health facility in Delta State, South South Nigeria. Trop J Obstet Gynaecol. 35:244–248. https://doi.org/10.4103/TJOG.TJOG_61_18
Kumar N, Singh AK (2015) Trends of male factor infertility, an important cause of infertility: a review of literature. J Hum Reprod Sci. 8:191–196. https://doi.org/10.4103/0974-1208.170370
The ESHRE Capri Workshop Group (2002) Physiopathological determinants of human infertility. Hum Reprod Update. 8(5):435–447
Brugo-Olmedo S, Chillik C, Kopelman S (2001) Definition and causes of infertility. Reprod BioMed Online. 2(1):41–53. https://doi.org/10.1016/s1472-6483(10)62187-6
Durairajanayagam D (2018) Lifestyle causes of male infertility. Arab J Urol. 16(1):10–20. https://doi.org/10.1016/j.aju.2017;12:004
Ferlin A, Raicu F, Gatta V et al (2007) Male infertility: role of genetic background. Reprod Biomed Online. 14:734–745. https://doi.org/10.1016/s1472-6483(10)60677-3
O'Flynn O'Brien KL, Varghese AC, Agarwal A (2010) The genetic causes of male factor infertility: a review. Fertil. Steril. 93:1–12. https://doi.org/10.1016/j.fertnstert.2009.10.045
Genetic Home Reference. 2020. CFTR gene. Available at https://ghr.nlm.nih.gov/gene/CFTR. .
Tahmasbpour E, Balasubramanian D, Agarwal A (2014) A multi-faceted approach to understanding male infertility: gene mutations, molecular defects and assisted reproductive techniques (ART) J. Assist Reprod Genet. 31:1115–1137. https://doi.org/10.1007/s10815-014-0280-6
Dada R, Thilagavathi J, Venkatesh S, Esteves SC, Agarwal A (2011) Genetic testing in male infertility. Open Reprod Sci. 3:42–56. https://doi.org/10.2174/1874255601103010042
Ajonuma LC, Ng EH, Chow PH et al (2005) Increased cystic fibrosis transmembrane conductance regulator (CFTR) expression in the human hydrosalpinx. Hum Reprod. 20(5):1228–1234. https://doi.org/10.1093/humrep/deh773
Genetic Home Reference. 2020. NR5A1 gene. Available at .
Jedidi I, Ouchari M, Yin Q (2018) Autosomal single-gene disorders involved in human infertility. Saudi J Biol Sci. 25(5):881–887. https://doi.org/10.1016/j.sjbs.2017.12.005
Bashamboo A, Ferraz-de-Souza B, Lourenço D et al (2010) Human male infertility associated with mutations in NR5A1 encoding steroidogenic factor 1. Am J Hum Genet. 87:505–512. https://doi.org/10.1016/j.ajhg.2010.09.009
Fabbri HC, de Andrade JGR, Soardi FC, et al. The novel p.Cys65Tyr mutation in NR5A1 gene in three 46, XY siblings with normal testosterone levels and their mother with primary ovarian insufficiency. BMC Med Genet. 2014; 15:7. DOI: 10.1186/1471-2350-15-7.
Genetic Home Reference. 2020. WT1 gene. Available at https://ghr.nlm.nih.gov/gene/WT1. .
Nathan A, Reinhardt P, Kruspe D et al (2017) The Wilms tumor protein Wt1 contributes to female fertility by regulating oviductal proteostasis. Hum Mol Genet. 26:1694–1705. https://doi.org/10.1093/hmg/ddx075
Wang XN, Li ZS, Ren Y et al (2013) The Wilms tumor gene, Wt1, is critical for mouse spermatogenesis via regulation of Sertoli cell polarity and is associated with non-obstructive azoospermia in humans. PLoS Genet. 9:e1003645. https://doi.org/10.1371/journal.pgen.1003645
Sakamoto J, Takata A, Fukuzawa R et al (2001) A novel WT1 gene mutation associated with Wilms’ Tumor and congenital male genitourinary malformation. Pediatr Res. 50:337–344. https://doi.org/10.1203/00006450-200109000-00008
Seabra CM, Quental S, Lima AC et al (2015) The mutational spectrum of WT1 in male infertility. J Urol. 193:1709–1715. https://doi.org/10.1016/j.juro.2014.11.004
Wang Y, Xiao M, Chem X et al (2015) WT1 recruits TET2 to regulate its target gene expression and suppress leukemia cell proliferation. Is. Mol Cell. 57(4):662–673. https://doi.org/10.1016/j.molcel.2014.12.023
Genetic Home Reference. 2020. FMR1 gene. Available at https://ghr.nlm.nih.gov/gene/FMR1. .
Coffee B, Keith K, Albizua I et al (2009) Incidence of fragile X syndrome by newborn screening for methylated FMR1 DNA. Am J Hum Genet. 85(4):503–514. https://doi.org/10.1016/j.ajhg.2009.09.007
Genetic Home Reference. 2020. GALT gene. Available at https://ghr.nlm.nih.gov/gene/GALT#conditions. .
Fridovich-Keil JL, Gubbels CS, Spencer JB (2011) Ovarian function in girls and women with GALT-deficiency galactosemia. J Inherit Metab Dis. 34(2):357–366. https://doi.org/10.1007/s10545-010-9221-4
Zorrilla M, Yatsenko AN (2013) The genetics of infertility: current status of the field. CurrGenet Med Rep. 1(4):10. https://doi.org/10.1007/s40142-013-0027-1
National Center for Biotechnology Information. 2020. GDF9 growth differentiation factor 9 [Homo sapiens (human)]. Available at https://www.ncbi.nlm.nih.gov/gene/2661. .
Zhao H, Qin Y, Kovanci E, Simpson JL, Chen ZJ, Rajkovic A (2007) Analyses of GDF9 mutation in 100 Chinese women with premature ovarian failure. Fertil Steril. 88(5):1474–1476. https://doi.org/10.1016/j.fertnstert.2007.01.021
Uniport .2020. UniProtKB - O60383 (GDF9_HUMAN). Available at https://www.uniprot.org/uniprot/O60383. Accessed March 18, 2020.
Genetic Home Reference. 2020.. MED12 gene. Available at https://ghr.nlm.nih.gov/gene/MED12#conditions. .
Genetic Home Reference. 2020. ANOS1 gene. Available at https://ghr.nlm.nih.gov/gene/ANOS1#location. .
Lopategui DM, Griswold AJ, Arora H, Clavijo RI, Tekin M, Ramasamy R (2018) A rare ANOS1 variant in siblings with Kallmann syndrome identified by whole exome sequencing. Androl. 6(1):53–57. https://doi.org/10.1111/andr.12432
Genetic Home Reference. 2020. LEP gene. Available at https://ghr.nlm.nih.gov/gene/LEP#location. .
Layman LC (2002) Human gene mutations causing infertility. J Med Genet. 39:153–161. https://doi.org/10.1136/jmg.39.3.153
Hodžić AM, Ristanović B, Zorn C et al (2017) Genetic variation in leptin and leptin receptor genes as a risk factor for idiopathic male infertility. Androl. 5(1):70–74. https://doi.org/10.1111/andr.12295
Genetic Home Reference. 2020. LEPR gene. Available at https://ghr.nlm.nih.gov/gene/LEPR#location. .
Genetic Home Reference. 2020. NR0B1 gene. Available at https://ghr.nlm.nih.gov/gene/NR0B1#location. .
Genetic Home Reference. 2020. HESX1 gene. Available at https://ghr.nlm.nih.gov/gene/HESX1#location. .
National Center for Biotechnology Information. 2020. LHB gene. Available at https://ghr.nlm.nih.gov/gene/LHB#location. .
El-Shal SA, Zidan HE, Rashad MN, Abdelaziz AM, Harira MM (2016) Association between genes encoding components of the leutinizing hormone/luteinizing hormone choriogonadotrophin receptor pathway and polycystic ovary syndrome in Egyptian women. Inter Union of Biochem Mol Biol. 68(1):23–36. https://doi.org/10.1002/iub.1457
Reen JK, Kerekoppa R, Deginal R et al (2018) Luteinizing hormone beta gene polymorphism and its effect on semen quality traits and luteinizing hormone concentrations in Murrah buffalo bulls. Asian-Australas J Anim Sci. 31(8):1119–1126. https://doi.org/10.5713/ajas.17.0679
Genetic Home Reference. 2020. LHCGR gene. Available at https://ghr.nlm.nih.gov/gene/LHCGR. .
Genetic Home Reference. 2020. AR gene. Available at https://ghr.nlm.nih.gov/gene/AR#location. .
Genetic Home Reference. 2020. SRY gene. Available at https://ghr.nlm.nih.gov/gene/SRY#synonyms. .
Lerchbaum B, Obermayer-Pietsch B (2012) Vitamin D and fertility: a systematic review. Eur JEndocrinol. 166:765–778. https://doi.org/10.1530/EJE-11-0984
Genetic Home Reference. 2020. VDR gene. Available at https://ghr.nlm.nih.gov/gene/VDR#location. .
Reginatto MW, Pizarro BM, Antunes RA, Mancebo ACA, Hoffmann L, Fernandes P. Vitamin D receptor TaqI polymorphism is associated with reduced follicle number in women utilizing assisted reproductive technologies. Front Endocrinol. 2018; 9: 252.| https://doi.org/10.3389/fendo.2018.00252.
Bagheri M, Abdi RI, Hosseini JN, Nanbakhsh F (2013) Vitamin D receptor TaqI gene variant in exon 9 and polycystic ovary syndrome risk. Int J Fertil Steril. 7(2):116–121
Szczepańsk M, Mostowska A, Wirstlein P, Skrzypczak J. Matthew MM, Jagodziński PP. Polymorphic variants in vitamin D signaling pathway genes and the risk of endometriosis-associated infertility. Mol Med Rep. 2015; 12 (5): 7109-7115. https://doi.org/10.3892/mmr.2015.4309.
Sunnotel O, Hiripi L, Lagan K et al (2010) Alterations in the steroid hormone receptor co-chaperone FKBPL are associated with male infertility: a case-control study. Reprod Biol Endocrinol. 8:22. https://doi.org/10.1186/1477-7827-8-22
Ketefian A, Jones MR, Krauss RM. Association study of androgen signaling pathway genes in polycystic ovary syndrome. Fertil Steril. 2016; 105(2):467-73.e4. DOI: 10.1016/j.fertnstert.2015;09: 043.
Demetriou C, Chanudet E, Joseph A et al (2019) Exome sequencing identifies variants in FKBP4 that are associated with recurrent fetal loss in humans. Hum Mol Genet. 28(20):3466–3474. https://doi.org/10.1093/hmg/ddz203
Ditton HJ, Zimmer J, Kamp C, Rajpert-De ME, Vogt PH (2004) The AZFa gene DBY (DDX3Y) is widely transcribed but the protein is limited to the male germ cells by translation control. Hum Mol Genet. 13(19):2333–2341. https://doi.org/10.1093/hmg/ddh240
Luddi A, Margollicci M, Gambera L et al (2009) Spermatogenesis in a man with complete deletion of USP9Y.N. Engl J Med. 360(9):881–885. https://doi.org/10.1056/NEJMoa0806218
Uniport. 2020. UniProtKB - O00507 (USP9Y_HUMAN). Available at https://www.uniprot.org/uniprot/O00507.
Habedanck R, Stierhof YD, Wilkinson CJ, Nigg EA (2005) The Polo kinase Plk4 functions in centriole duplication. Nat Cell Biol. 7:1140–1146. https://doi.org/10.1038/ncb1320
GeneCards. 2020. PLK4 Gene. Available at https://www.genecards.org/cgi-bin/carddisp.pl?gene=PLK4. .
Harris RM, Weiss J, Jameson JL (2011) Male hypogonadism and germ cell loss caused by a mutation in Polo-like kinase 4. Endocrinol. 152:3975–3985. https://doi.org/10.1210/en.2011-1106
Miyamoto T, Minase G, Shin T, Ueda H, Okada H, Sengoku K (2017) Human male infertility and its genetic causes. Reprod Med Biol. 16(2):81–88. https://doi.org/10.1002/rmb2.12017
Veleri S, Bishop K, Dalle Nogare DE et al (2012) Knockdown of Bardet-Biedl syndrome gene BBS9/PTHB1 leads to cilia defects. PLoS ONE. 7(3):e34389. https://doi.org/10.1371/journal.pone.0034389
HyunJun K, Seung KL, Min-Ho K et al (2008) Parathyroid hormone-responsive B1 gene is associated with premature ovarian failure. Hum Reprod. 23(6):1457–1465. https://doi.org/10.1093/humrep/den086
Genetic Home Reference. 2020. FSHR gene. Available at https://ghr.nlm.nih.gov/gene/FSHR#location. .
Aittomäki K, Lucena JD, Pakarinen P et al (1995) Mutation in the follicle-stimulating hormone receptor gene causes hereditary hypergonadotropic ovarian failure. Cell. 82(6):959–968 https://doi.org/10.1016/0092-8674(95)90275-9
Uniport. 2020. UniProtKB - P23945 (FSHR_HUMAN). Available at https://www.uniprot.org/uniprot/P23945. .
Miyamoto T, Tsujimura A, Miyagawa Y, Koh E, Namiki SK. Male infertility and its causes in human. Adv Urol. 2012; Article ID 384520. DOI: 10.1155/2012/384520.
Uniport. 2020. UniProtKB - Q9BXB7 (SPT16_HUMAN). Available at https://www.uniprot.org/uniprot/Q9BXB7. Accessed 23 march, 2020.
Dam AH, Koscinski I, Kremer JA et al (2007) Homozygous mutation in SPATA16 is associated with male infertility in human globozoospermia. Am J Hum Genet. 81(4):813–820. https://doi.org/10.1086/521314
Genetic Home Reference. 2020. AURKC gene. Available at https://ghr.nlm.nih.gov/gene/AURKC. .
Genetic Home Reference. 2020. CATSPER1 gene. Available at https://ghr.nlm.nih.gov/gene/CATSPER1#location. .
Avenarius MR, Hildebrand MS, Zhang Y et al (2009) Human male infertility caused by mutations in the CATSPER1 channel protein. Am J Hum Gen. 84(4):505–510 https://doi.org/10.1016/j.ajhg.2009.03.004
Nuti F, Krausz C (2008) Gene polymorphisms/mutations relevant to abnormal spermatogenesis. Reprod Biomed Online. 16:504–513. https://doi.org/10.1016/s1472-6483(10)60457-9
Genetic Home Reference. 2020. MTHFR gene. Available at https://ghr.nlm.nih.gov/gene/MTHFR#normalfunction. Accessed March, 2020.
Friedman G, Goldschmidt N, Friedlander Y et al (1999) A common mutation A1298C in human methylenetetrahydrofolate reductase gene: association with plasma total homocysteine and folate concentrations. J Nutr. 129:1656–1661. https://doi.org/10.1093/jn/129.9.1656
Marques CJ, Costa P, Vaz B et al (2008) Abnormal methylation of imprinted genes in human sperm is associated with oligozoospermia. Mol Hum Reprod. 14:67–74. https://doi.org/10.1093/molehr/gam093
National Center for Biotechnology Information. 2020. SYCP3 synaptonemal complex protein 3 [Homo sapiens (human)]. Available at https://www.ncbi.nlm.nih.gov/gene/50511. .
Uniport. 2020. UniProtKB - Q8IZU3 (SYCP3_HUMAN). Available at https://www.uniprot.org/uniprot/Q8IZU3. .
GeneCards. 2020. HSF2 Gene. Available at https://www.genecards.org/cgi-bin/carddisp.pl?gene=HSF2. .
Mou L, Wang Y, Li H et al (2013) A dominant-negative mutation of HSF2 associated with idiopathic azoospermia. Hum Genet. 132(2):159–165
Wang G, Ying Z, Jin X et al (2004) Essential requirement for both hsf1 and hsf2 transcriptional activity in spermatogenesis and male fertility. Genesis. 38(2):66–80. https://doi.org/10.1002/gene.20005
GeneCards. 2020. SYCP2 Gene. Available at https://www.genecards.org/cgi-bin/carddisp.pl?gene=SYCP2. .
Schilit SLP, Menon S, Friedrich C et al (2020) SYCP2 translocation-mediated dysregulation and frameshift variants cause human male infertility. Am J Hum Genet. 6(1):41–57. https://doi.org/10.1016/j.ajhg.2019.11.013
Takemoto K, Imai Y, Saito K et al (2020) Sycp2 is essential for synaptonemal complex assembly, early meiotic recombination and homologous pairing in zebrafish spermatocytes. PLoS Genet. 16(2):e1008640. https://doi.org/10.1371/journal.pgen.1008640
Bolcun-Filas E, Bannister LA, Barash A et al (2011) A-MYB (MYBL1) transcription factor is a master regulator of male meiosis. Develop. 138:3319–3330. https://doi.org/10.1242/dev.067645
Yang F, Silber S, Leu NA. TEX11 is mutated in infertile men with azoospermia and regulates genome-wide recombination rates in mouse. EMBO Mol Med. 2015; 7(9):1198–1210. doi:10.15252/emmm.201404967.
Uniport. 2020. UniProtKB - Q8IYF3 (TEX11_HUMAN). Available at https://www.uniprot.org/uniprot/Q8IYF3. .
Genetic Home Reference. 2020. KIT gene. Available at https://ghr.nlm.nih.gov/gene/KIT#conditions. .
Lars R, Johan L (2016) KIT (v-kit Hardy-Zuckerman 4 feline sarcoma viral oncogene homolog). Atlas Genet Cytogenet Oncol Haematol. 20(8):441–444 http://atlasgeneticsoncology.org/Genes/KITID127.html
Uniport. 2020. UniProtKB - Q8IZP9 (AGRG2_HUMAN). Available at https://www.uniprot.org/uniprot/Q8IZP9. .
Patat O, Pagin A, Siegfried A et al (2016) Truncating mutations in the adhesion G protein-coupled receptor G2 gene ADGRG2 cause an X-linked congenital bilateral absence of vas deferens. Am J Hum Genet. 99(2):437–442. https://doi.org/10.1016/j.ajhg.2016.06.012
National Center for Biotechnology Information. 2020. FKBP6 FKBP prolyl isomerase 6 [Homo sapiens (human)]. Available at https://www.ncbi.nlm.nih.gov/gene/8468. .
Crackower MA, Kolas NK, Noguchi J (2003) Essential role of Fkbp6 in male fertility and homologous chromosome pairing in meiosis. Science. 300(5623):1291–1295. https://doi.org/10.1126/science.1083022
Uniport. 2020. UniProtKB - O75344 (FKBP6_HUMAN). Available at https://www.uniprot.org/uniprot/O75344. .
Akmal M, Aulanni’am A, Widodo MA, Sumitro SB, Purnomo BB (2016) The important role of protamine in spermatogenesis and quality of sperm: a mini review. Asian Pac J Reprod. 5:357–360. https://doi.org/10.1016/j.apjr.2016.07.013
Ravel C, Chantot-Bastaraud S, El Houate B et al (2007) Mutations in the protamine 1 gene associated with male infertility. Mol Hum Reprod. 13(7):461–464. https://doi.org/10.1093/molehr/gam031
Jiang W, Sun H, Zhang J (2005) Polymorphisms in protamine 1 and protamine 2 predict the risk of male infertility: a meta-analysis. Sci Rep. 5:15300. https://doi.org/10.1038/srep15300
Siasi E, Aleyasin A, Mowla J, Sahebkasha H (2012) Association study of six SNPs in PRM1, PRM2 and TNP2 genes in iranian infertile men with idiopathic azoospermia. Iran J Reprod Med. 10:329–336
Miyagawa Y, Nishimura H, Tsujimura A et al (2005) Single-nucleotide polymorphisms and mutation analyses of the TNP1 and TNP2 genes of fertile and infertile human male. J Androl. 26(6):779–786. https://doi.org/10.2164/jandrol.05069
Heidari MM, Khatami M, Talebi AR, Moezzi F. Mutation analysis of TNP1 gene in infertile men with varicocele. Iran J Reprod Med. 2014; 12(4):257-62. .
Adham IM, Nayernia K, Burkhardt-Göttges E et al (2001) Teratozoospermia in mice lacking the transition protein 2 (Tnp2). Mol Hum Reprod. 7(6):513–520. https://doi.org/10.1093/molehr/7.6.513
Uniport. 2020. UniProtKB - Q9NQZ3 (DAZ1_HUMAN). Available at https://www.uniprot.org/uniprot/Q9NQZ3. .
Fernandes K, Huellen J, Goncalves H et al (2002) High frequency of DAZ1/DAZ2 gene deletions in patients with severeoligozoospermia. Mol Hum Reprod. 8(3):286–298. https://doi.org/10.1093/molehr/8.3.286
Genetic Home Reference. 2020. DAZI gene. Available at https://ghr.nlm.nih.gov/gene/DAZ1. .
Deans B, Griffin CS, Maconochie M, Thacker J (2000) Xrcc2 is required for genetic stability, embryonic neurogenesis and viability in mice. EMBO J. 19(24):6675–6685. https://doi.org/10.1093/emboj/19.24.6675
Yang Y, Guo J, Dai L (2018) XRCC2 mutation causes meiotic arrest, azoospermia and infertility. J Med Genet. 55:628–636. https://doi.org/10.1136/jmedgenet-2017-105145
GeneCards. 2020. CCDC62 Gene. Available at https://www.genecards.org/cgi-bin/carddisp.pl?gene=CCDC62. .
Li Y, Li C, Lin S et al (2017) A nonsense mutation in Ccdc62 gene is responsible for spermiogenesis defects and male infertility in repro29/repro29 mice. Biol Reprod. 96(3):587–597 https://doi.org/10.1095/biolreprod.116.141408
Hwang JY, Mannowetz N, Zhang Y. EFCAB9 is a pH-Dependent Ca2+ sensor that regulates CatSper channel activity and sperm motility. BioRxiv. 2018; Article no 459487. doi: https://doi.org/10.1101/459487.
Yatsenko AN, Roy A, Chen R (2006) Non-invasive genetic diagnosis of male infertility using spermatozoal RNA: KLHL10 mutations in oligozoospermic patients impair homodimerization. Hum Mol Genet. 15:3411–3419. https://doi.org/10.1093/hmg/ddl417
Kuo YC, Lin YH, Chen HI et al (2012) SEPT12 mutations cause male infertility with defective sperm annulus. Hum Mutat. 33:710–719. https://doi.org/10.1002/humu.22028
Uniport. 2020. UniProtKB - Q92750 (TAF4B_HUMAN). Available at https://www.uniprot.org/uniprot/Q92750. .
Ayhan Ö, Balkan M, Guven A et al (2014) Truncating mutations in TAF4B and ZMYND15 causing recessive azoospermia. J Med Genet. 51:239–244. https://doi.org/10.1136/jmedgenet-2013-102102
Yan W, Si Y, Slaymaker S et al (2010) Zmynd15 encodes a histone deacetylase-dependent transcriptional repressor essential for spermiogenesis and male fertility. J Biol Chem. 285:31418–31426. https://doi.org/10.1074/jbc.M110.116418
Uniport. 2020. UniProtKB - Q9H091 (ZMY15_HUMAN). Available at https://www.uniprot.org/uniprot/Q9H091. .
National Center for Biotechnology Information. 2020. NANOS1 nanos C2HC-type zinc finger 1 [Homo sapiens (human)]. Available at https://www.ncbi.nlm.nih.gov/gene/340719. .
Kusz-Zamelczyk K, Sajek M, Spik A (2013) Mutations of NANOS1, a human homologue of the Drosophila morphogen, are associated with a lack of germ cells in testes or severe oligo-astheno-teratozoospermia. J Med Genet. 50:187–193. https://doi.org/10.1136/jmedgenet-2012-101230
Uniport. 2020. UniProtKB - Q8WY41 (NANO1_HUMAN). Available at https://www.uniprot.org/uniprot/Q8WY41. .
Uniport. 2020. UniProtKB - Q7Z4T8 (GLTL5_HUMAN). Available at https://www.uniprot.org/uniprot/Q7Z4T8. .
Takasaki N, Tachibana K, Ogasawara S (2014) A heterozygous mutation of GALNTL5 affects male infertility with impairment of sperm motility. Proc Natl Acad Sci USA. 111:1120–1125. https://doi.org/10.1073/pnas.1310777111
National Center for Biotechnology Information. 2020. GNRHR gonadotropin releasing hormone receptor [Homo sapiens (human)]. Available at https://www.ncbi.nlm.nih.gov/gene/2798. .
Zernov N, Skoblov M, Baranova A, Boyarsky K (2016) Mutations in gonadotropin-releasing hormone signaling pathway in two nIHH patients with successful pregnancy outcomes. Reprod Biol Endocrinol. 14:48. https://doi.org/10.1186/s12958-016-0183-8
Uniport. 2020. UniProtKB - P30968 (GNRHR_HUMAN). Available at https://www.uniprot.org/uniprot/P30968. .
Genetic Home Reference. 2020. PROP1 gene. Available at https://ghr.nlm.nih.gov/gene/PROP1#location. .
Uniport (2020) UniProtKB - Q9Y5R6 (DMRT1_HUMAN). Available at https://www.uniprot.org/uniprot/Q9Y5R6.Accessed (March 25, 2020)
Uniport. 2020. UniProtKB - P41225 (SOX3_HUMAN). Available at https://www.uniprot.org/uniprot/P41225. .
Uniport. 2020. UniProtKB - Q2MKA7 (RSPO1_HUMAN). Available at https://www.uniprot.org/uniprot/Q2MKA7. .
Tomaselli S, Megiorni F, De Bernardo C et al (2007) Syndromic true hermaphroditism due to an R-spondin1 (RSPO1) homozygous mutation. Human Mutat. 29(2):220–226. https://doi.org/10.1002/humu.20665
National Center for Biotechnology Information. 2020. BMP15 bone morphogenetic protein 15 [Homo sapiens (human)]. Available at https://www.ncbi.nlm.nih.gov/gene/9210. .
Uniport. 2020. UniProtKB - O95972 (BMP15_HUMAN). Available at https://www.uniprot.org/uniprot/O95972. .
National Center for Biotechnology Information. 2020. FIGLA folliculogenesis specific bHLH transcription factor [Homo sapiens (human)]. Available at https://www.ncbi.nlm.nih.gov/gene/344018. .
Zhao H, Chen ZJ, Qin Y et al (2008) Transcription factor FIGLA is mutated in patients with premature ovarian failure. Am J Hum Genet. 82(6):1342–1348. https://doi.org/10.1016/j.ajhg.2008.04.018
Soyal SM, Amleh A, Dean J (2000) FIGalpha. A germ cell-specific transcription factor required for ovarian follicle formation. Develop. 127(21):4645–4654
Uniport. 2020. UniProtKB - Q6QHK4 (FIGLA_HUMAN). Available at https://www.uniprot.org/uniprot/Q6QHK4. .
Rajkovic A, Pangas SA, Ballow D, Suzumori N, Matzuk MM (2004) NOBOX deficiency disrupts early folliculogenesis and oocyte-specific gene expression. Science. 305(5687):1157–1159. https://doi.org/10.1126/science.1099755
Bouilly J, Bachelot A, Broutin I, Touraine P, Binart N (2011) Novel NOBOX loss-of-function mutations account for 6.2% of cases in a large primary ovarian insufficiency cohort. Hum Mutat. 32(10):1108–1113. https://doi.org/10.1002/humu.21543
Qin Y, Choi Y, Zhao H, Simpson JL, Chen ZJ, Rajkovic A (2007) NOBOX homeobox mutation causes premature ovarian failure. Am J Hum Genet. 81(3):576–581. https://doi.org/10.1086/519496
Tahara N, Kawakami H, Zhang T et al (2018) Temporal changes of Sall4 lineage contribution in developing embryos and the contribution of Sall4-lineages to postnatal germ cells in mice. Sci Rep. 8:16410 https://doi.org/10.1038/s41598-018-34745-5
Wang B, Li L, Ni F (2009) Mutational analysis of SAL-Like 4 (SALL4) in Han Chinese women with premature ovarian failure. Mol Hum Reprod. 15(9):557–562. https://doi.org/10.1093/molehr/gap046
GeneCards. 2020. FSHB Gene. Available at https://www.genecards.org/cgi-bin/carddisp.pl?gene=FSHB#summaries. .
Layman LC, Lee EJ, Peak DB (1997) Delayed puberty and hypogonadism caused by a mutation in the follicle stimulating hormone β-subunit gene. N Engl J Med. 337:607–611
Rull1 K, Laan M. Expression of β-subunit of human chorionic gonadotropin genes during the normal and failed pregnancy. Hum Reprod. 2005; 20(12): 3360–3368. doi: https://doi.org/10.1093/humrep/dei261.
Nagirnaja L, Venclovas C, Rull K et al (2012) Structural and functional analysis of rare missense mutations in human chorionic gonadotrophin β-subunit. Mol Hum Reprod. 18(8):379–390. https://doi.org/10.1093/molehr/gas018
Poikkeus P, Hiilesmaa V, Tiitinen A (2002) Serum HCG 12 days after embryo transfer in predicting pregnancy outcome. Hum Reprod. 17:1901–1905. https://doi.org/10.1093/humrep/17.7.1901
ational Center for Biotechnology Information. 2020. SOHLH1 spermatogenesis and oogenesis specific basic helix-loop-helix 1 [Homo sapiens (human)]. Available at https://www.ncbi.nlm.nih.gov/gene/402381. .
Uniport. 2020. UniProtKB - Q5JUK2 (SOLH1_HUMAN). Available at https://www.uniprot.org/uniprot/Q5JUK2. .
Toyoda S, Yoshimura T, Mizuta J, J-i M (2014) Auto-regulation of the Sohlh1 gene by the SOHLH2/SOHLH1/SP1 complex: implications for early spermatogenesis and oogenesis. PLoS ONE. 9(7):e101681. https://doi.org/10.1371/journal.pone.0101681
Shin YH, Ren Y, Suzuki H et al (2017) Transcription factors SOHLH1 and SOHLH2 coordinate oocyte differentiation without affecting meiosis I. J Clin Invest. 127(6):2106–2211. https://doi.org/10.1172/JCI90281
Qin Y, Jiao X, Dalgleish R et al (2014) Novel variants in the SOHLH2 gene are implicated in human premature ovarian failure. Fertil Steril. 101(4):1104–1109. https://doi.org/10.1016/j.fertnstert.2014.01.001
Song B, Zhang Y, He XJ et al (2015) Association of genetic variants in SOHLH1 and SOHLH2 with non-obstructive azoospermia risk in the Chinese population. Eur J Obstet Gynecol Reprod Biol. 184:48–52. https://doi.org/10.1016/j.ejogrb.2014.11.003
Hao J, Yamamoto M, Richardson TE et al (2008) Sohlh2 knockout mice are male-sterile because of degeneration of differentiating type A spermatogonia. Stem Cells 26(6):1587–1597
Wu X, Thomas P, Yong ZY (2018) Pgrmc1 Knockout impairs oocyte maturation in zebrafish. Front.Endocrinol. 9:560. https://doi.org/10.3389/fendo.2018.00560
Paskulin DD, Cunha-Filho JS, Paskulin LD, Souza CAB, Ashton-Prolla P (2013) ESR1 rs9340799 is associated with endometriosis-related infertility and in vitro fertilization failure. Disease Markers. 35(6):907–913. https://doi.org/10.1155/2013/796290
Manosalva I, González A, Kageyama R (2013) Hes1 in the somatic cells of the murine ovary is necessary for oocyte survival and maturation. Develop Biol. 375(2):140–151. https://doi.org/10.1016/j.ydbio.2012.12.015
Cariati F, D’Argenio V, Tomaiuolo R (2019) The evolving role of genetic tests in reproductive medicine. J Transl Med. 17:267. https://doi.org/10.1186/s12967-019-2019-8
Devine K, Roth L. 2020. Genetic testing of embryos. Shady grove fertility. Available at https://www.shadygrovefertility.com/treatments-success/advanced-treatments/genetic-testing-embryos.
Treff NR, Fedick A, Tao X, Devkota B, Taylor D, Scott RT (2013) Evaluation of targeted next-generation sequencing-based preimplantation genetic diagnosis of monogenic disease. Fertil Steril. 99:1377–1384. https://doi.org/10.1016/j.fertnstert.2012.12.018
Acknowledgments
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
TOY conceptualized and did literature searches, article writing, and correspondence. UUL, HA, YSK, SSR, ZA, and SA did literature searches, sorting, and referencing. All authors proofread and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Yahaya, T.O., Liman, U.U., Abdullahi, H. et al. Genes predisposing to syndromic and nonsyndromic infertility: a narrative review. Egypt J Med Hum Genet 21, 46 (2020). https://doi.org/10.1186/s43042-020-00088-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43042-020-00088-y