Abstract
Background
Forgotten Joint Score (FJS) has become a popular tool for total knee arthroplasty (TKA), but almost all studies had assessment performed 1 year after surgery. There is a need for a sensitive tool for earlier outcome assessment. The aim of this study was to investigate the usefulness of FJS within the first year after TKA.
Methods
This was a cross-sectional study. Patients within the first year after primary TKA were recruited. FJS was translated into the local language with a cross-cultural adaptation and was validated by assessing the correlation with the Western Ontario and McMaster Universities Arthritis Index score (WOMAC). Ceiling and floor effects (highest or lowest 10% or 15%) of both scores were compared. Skewness of scores was assessed with a histogram.
Results
One hundred sixty-three subjects were recruited: 84 (51.5%) had evaluation at 3 months after the operation, 56 (34.4%) at 6 months, and 23 (14.1%) at 12 months. FJS had fewer patients at the highest 10% (10.7% vs. 16.1%, P = 0.046) or 15% (19.6% vs. 32.1%, P = 0.027) at 6 months and within the first year overall (6.7% vs. 13.5%, P <0.001; 14.1% vs. 22.7%, P <0.001). Also, it had more patients at the lowest 10% (16.7% vs. 0%, P <0.001) or 15% (21.4% vs. 0%, P <0.001) at 3 months, 6 months (10.7% vs. 0%, P <0.001), and overall (12.9% vs. 0%, P <0.001; 16.6% vs. 0%, P <0.001). The skewness was much less than WOMAC (0.09 vs. −0.56).
Conclusions
FJS has a low ceiling effect but a high floor effect in the first year after TKA. Such characteristics make it less useful for the general assessment of early patient report outcome after operation.
Similar content being viewed by others
Introduction
Forgotten Joint Score (FJS) has become a popular tool in assessing the outcome of total knee arthroplasty (TKA). It has been shown to have a good correlation with classic outcome scores like the Western Ontario and McMaster Universities Arthritis Index (WOMAC) score, the Knee Injury and Osteoarthritis Outcome Score (KOOS), and the Oxford Knee Score (OKS) [1,2,3,4]. A lower ceiling effect was observed in many studies [1,2,3, 5, 6], which suggests an advantage of this tool in assessing patients with good outcome. However, almost all studies on FJS were performed on patients more than 1 year after surgery [1, 7,8,9,10]. The rationale behind this was likely that the outcome of surgery had not reached plateau for assessment until 1 year after surgery. Nevertheless, Hiyama et al. [11] reported FJS improvement within 6 months after surgery reaching a plateau from 6 to 12 months. Also, with the increasing popularity of fast-track surgery, the need for early outcome assessment has become much greater. Newer surgical techniques, implant design, or perioperative protocol might result in subtle improvement in early outcome but with no long-term effect [12]. Despite this greater need for early and sensitive outcome assessment, appropriate tools for measurement are lacking [13] and evidence on the use of FJS earlier than 1 year is scarce [4, 5].
The aim of this study was to investigate the usefulness of FJS for assessing patients within the first year after TKA. The validity and reliability of FJS for early outcome assessment were investigated. In particular, the ceiling and floor effects of FJS were assessed. The null hypothesis of the study was that there is no difference in the ceiling and floor effects between FJS and WOMAC score at the early months after TKA.
Materials and methods
Subjects
This was a cross-sectional study. Patients who were within the first year after primary knee arthroplasty with post-operative evaluation in the out-patient clinic of our institute between July and September 2018 were recruited. Patients with dementia, psychiatric illness, and post-operative local complications like infection and fracture were excluded. All cases were performed with tourniquet during the whole procedure, medial parapatellar approach, posterior cruciate ligament sacrificed, cementation, and local infiltrative analgesia (30 mg ketorolac, 100 mg levobupivacaine, 0.5 mg adrenaline). Implants used were Attune (Depuy, Warsaw, IN, USA), Evolution (Microport, Arlington, TX, USA), Triathlon (Stryker, Mahwah, NJ, USA), or Legacy or Persona (Zimmer, Warsaw, IN, USA). Patients with four or more questions unanswered were also excluded from the whole study [3] and those with any question unanswered were excluded from testing for internal consistency. Institutional review board approval was obtained from the regional ethics committee (reference number: KW/EX-19-109(142–12)), and informed verbal consent was obtained from all patients.
Outcome
All cases were evaluated by WOMAC score and FJS. Ceiling and floor effects of FJS and WOMAC score were assessed. They were defined as the proportion of patients scoring within the highest and the lowest percentile, respectively. Previous studies used either the 10th percentile [4] or the 15th percentile [3, 10]. The present study used both cutoff points to give a more detailed analysis. Validity of FJS was assessed by correlation with WOMAC score, which is a well-established outcome score widely used for total joint arthroplasty. Internal consistency within the questionnaire was assessed by correlation between all individual questions.
Translation of FJS
Translation and cross-cultural adaptation were performed in the following steps: Two groups of translators were formed. Each group consisted of two bilingual researchers; one was an orthopedic surgeon and the other was an orthopedic nursing specialist. The English FJS was first translated independently by each member of the first group into two Cantonese Chinese versions (CC1 and CC2). The two versions were compared between the two translators and combined into a single Cantonese Chinese version (CC1–2).
Another group of bilingual researchers then “back-translated” the Cantonese Chinese version (CC1–2) into English again. Each of the translators would translate their individual version. The back-translated English versions were then compared with the original English questionnaire for “equivalence” in content, semantics, and concept by all of the involved translators. The process was repeated for those problematic questions whose meanings differ until equivalence was met. The adopted version after the above procedures would be administered to the first 20 subjects as a pilot version (CC-P) to assess its comprehensibility, fluency, and clarity. Owing to the high rate of illiteracy in elderly Cantonese, the questionnaire was to be read out word by word to illiterate patients by their relatives or helpers in the hospital. Since Cantonese Chinese is both a spoken and a written language, there would not be any discrepancy between comprehension by reading and hearing. The feedback from patients and helpers was used to make minor amendments to the final version (CC-F). This final version would then be subjected only to validity and reliability testing.
Cross-cultural adaptation of FJS
In question 5, instead of asking the awareness of their artificial joint while travelling in a car, we have slightly modified the question to the awareness during any kind of traffic given the higher possibility of patients using public transport, which could be minivan, bus, train, and subway. In question 10, owing to the low popularity of gardening in our locality of Cantonese Chinese, the content about gardening was modified. Subjects were asked about awareness of their artificial joint while doing “trivial” activities instead of gardening. The idea was to measure the awareness while the subjects were engaged in activities that were not demanding physically (as in questions 11 and 12) but could distract them from their artificial joint.
Validity and reliability of FJS
The convergent construct validity of the questionnaire was assessed by correlation of FJS with the WOMAC score, which is a well-established outcome score widely used for total joint arthroplasty. The degree of correlation was classified in accordance with Landis and Koch’s guidelines [14] of almost perfect (>0.8), substantial (0.6–0.8), moderate (0.4–0.6), fair (0.2–0.4), slight (0.0–0.2), or poor (0.0). Internal consistency was assessed by computerized calculation of correlation between all individual questions to give a correlation statistic called Cronbach’s α. It was classified as excellent (≥0.9), good (0.8–0.9), acceptable (0.7–0.8), questionable (0.6–0.7), poor (0.5–0.6), or unacceptable (<0.5).
Statistical analysis
Correlation between FJS and WOMAC score was analyzed by Pearson test and reported as the Pearson correlation coefficient (R). Correlation between individual questionnaires was analyzed by Cronbach’s α. The difference in ceiling and floor effects was analyzed by chi-squared test. All tests were performed with IBM SPSS version 20.0 (IBM, Armonk, NY, USA). A P value of less than 0.05 was considered statistically significant.
Results
Validation
One hundred sixty-nine patients were evaluated after TKA during the study period. One case was excluded because of dementia, two because of psychiatric illness, one because of infection, and one because of fracture. Another case was excluded because of missing answers for four questions of FJS. In total, 163 subjects were recruited for validity testing (Fig. 1). Surgical implants used were Attune (24), Evolution (41), Triathlon (33), Legacy (45), and Persona (20). Thirty-eight cases did not complete all answers of FJS and were excluded for analysis for internal consistency. The mean age was 72 ± 7.5 (55–82) years, and 70.1% were female (Table 1). Eighty-four cases (51.5%) had evaluation at 3 months after the operation, 56 (34.4%) at 6 months, and 23 (14.1%) at 12 months. The overall response rate for all questions of FJS was 96.3% (88.4–100).
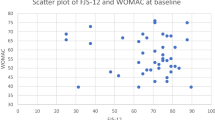
Validity of the FJS was verified by moderate correlation between WOMAC score and FJS (R = −0.52, P <0.001) (Table 2). Excellent internal consistency was found for the 12 questions of FJS (Cronbach’s α: 0.96).
Ceiling, floor effects, and skewness
FJS was found to have a lower ceiling effect than WOMAC score with a significantly lower proportion of patients among the highest 10% and 15% scores at 6 months and within the first year overall (Table 3). There was also a trend of lower percentage of ceiling in FJS at 12 months, although the difference was not statistically significant. On the other hand, a significantly higher floor effect at the first 6 months was found in FJS with a significantly higher proportion of patients scoring the lowest 10% and 15% at 3 months, 6 months, and within the first year overall. The skewness of FJS was significantly lower than WOMAC score (0.09 vs. −0.56) for the whole sample. The histogram of the whole sample showed obvious skewness to the left in WOMAC score and more even distribution in FJS (Fig. 2).
Discussion
The most important finding from the present study is that FJS had a significantly lower ceiling effect and a higher floor effect within the first year after TKA. To the best of our knowledge, only two studies have investigated the use of FJS in the first year after TKA [4, 11]. In one of the studies, Hamilton et al. successfully validated FJS with OKS and noticed a lower ceiling effect [4], defined as scoring maximum 10% in FJS (12.6% vs. 25.5%). A more elaborate definition for ceiling or floor effect (that is, scoring the 10% and 15% highest or lowest score) was used by the present study. Also, this might be the first study to compare FJS with WOMAC score for the first 12 months after TKA. Consistent with the study by Hamilton et al., a lower ceiling effect of FJS was found even at 6 months after surgery. The finding was also consistent with the histogram in the present study, which showed a more even distribution of FJS, while WOMAC score was heavily skewed to the left. The skewness of FJS was much lower than WOMAC score (0.09 vs. −0.56). Other studies have shown a lower ceiling effect at longer post-operative periods. Behrend et al. [1] invented FJS and defined ceiling as scoring maximum in the new outcome scale. They first reported a lower percentage of ceiling in FJS (9.2%) compared with WOMAC score (16.7%–46.7%) in subjects 31 (15–58) months after TKA. Thompson et al. [2] also reported a lower ceiling effect (maximum score) in FJS than WOMAC score in subjects 39 months after TKA (6.8% vs. 9%). Similarly, Thomsen et al. [3] reported a lower ceiling effect in FJS than OKS (16% vs. 37%) in subjects 1–4 years after TKA. Ceiling was defined as scoring the highest 15% in their study. Using the same definition, Thienpont et al. [10] showed a lower ceiling effect of FJS compared with the quality-of-life section of the KOOS (9% vs. 29%). Another study by the same authors [8] showed a very large ceiling effect (maximum score) of 40%. However, more than half of the subjects in that study received partial knee arthroplasty, which could have affected the analysis to a large extent. In short, FJS seems to be a better tool to assess patients with good outcome in TKA even within the first year after surgery.
The floor effect of FJS was less well described in the literature. The present study might be the first to compare the floor effect of FJS with other outcome scores. Thienpont et al. [8] reported a floor effect of 16% of patients at least 1 year after TKA, but as mentioned above, the results of the study were confounded by partial knee arthroplasties. A study by Thienpont and Zorman showed a floor effect of 0–2% [9] at 1 year or more after TKA. However, the results were not compared with other scoring systems. Cao et al. [6] reported no floor effect of FJS in subjects at an average of 28 months (12–94) after TKA. But there was no comparison with other scoring systems. The present study demonstrated a significantly higher floor effect in FJS than WOMAC score in the first 6 months after TKA. This was understandable given the natural course of recovery after TKA, which usually takes 3–6 months for early symptoms due to surgery to resolve. Hiyama et al. [11] attributed this to the presence of pain in the first month. In this regard, FJS seems not to be a good choice to assess patients with worse outcome, particularly in the first 6 months after surgery.
Other findings of the present study included excellent response rate and internal consistency of FJS within 1 year from TKA. These were consistent with other studies on the use of FJS after 1 year from TKA. Also, the validity of the tool was confirmed by significant correlation with WOMAC score. The moderate correlation of 0.52 was not as high as reported in other studies (0.7–0.79) [1, 2]. This could be explained by the large difference in ceiling and floor effect between two scoring systems noticed in the first year in the present study.
Overall, the present study suggests that FJS is a useful tool in assessing the superiority of early results after knee arthroplasty. It might be particularly useful where differences in good outcome are not easily detectable because of subtle differences in prosthesis design, surgical technique, or post-operative regime. It might also be particularly valuable when the differences only lie in the early phase after surgery, such as comparison of the outcome of different practices of fast-track surgery. However, owing to the higher floor effect in the first 6 months after surgery noticed in FJS in the present study, one should be mindful of such limitations of this tool. It is likely not to be a proper tool for early detection or comparison of poor outcome in TKA. A better tool may be required for an overall assessment of early patient report outcome.
There were some limitations of the present study. First, the number of patients having scores at 12 months was small. This might have rendered the absence of significant results at 12 months. Second, owing to the expected increase in FJS during the first 6 months, test-retest reliability was not assessed in the present study [11]. Nevertheless, it has been found to be excellent by other studies [1,2,3]. Also, body mass index, preoperative alignment, and symptom duration might affect the final FJS but they were not analyzed in the present study. This might have affected the ceiling or floor effect should they have deviated grossly from normal distribution in the recruited sample. Another limitation of the present study was that the ceiling and floor effect of individual questions within the FJS was not assessed. The knowledge of this might help the development of a better measurement tool to assess early outcome of knee arthroplasty surgery.
Conclusion
FJS has a low ceiling effect but a very high floor effect in the first year after TKA. Such characteristics make it a useful tool specifically in comparing the superiority of early results after knee arthroplasty but it is less useful for general assessment of early patient report outcome after an operation.
Availability of data and materials
The data that support the findings of this study are available, but consent to share them with the public or a third party has not been obtained.
Abbreviations
- FJS:
-
Forgotten Joint Score
- KOOS:
-
Knee Injury and Osteoarthritis Outcome Score
- OKS:
-
Oxford Knee Score
- TKA:
-
Total knee arthroplasty
- WOMAC:
-
Western Ontario and McMaster Universities Arthritis Index
References
Behrend H, Giesinger K, Giesinger JM, Kuster MS (2012) The “forgotten joint” as the ultimate goal in joint arthroplasty: validation of a new patient-reported outcome measure. J Arthroplast 27(3):430
Thompson SM, Salmon LJ, Webb JM, Pinczewski LA, Roe JP (2015) Construct validity and test re-test reliability of the forgotten joint score. J Arthroplast 30(11):1902
Thomsen MG, Latifi R, Kallemose T, Barfod KW, Husted H, Troelsen A (2016) Good validity and reliability of the forgotten joint score in evaluating the outcome of total knee arthroplasty. Acta Orthop 87(3):280
Hamilton DF, Loth FL, Giesinger JM, Giesinger K, MacDonald DJ, Patton JT et al (2017) Validation of the English language Forgotten Joint Score-12 as an outcome measure for total hip and knee arthroplasty in a British population. Bone Joint J 99-b(2):218
Hamilton DF, Giesinger JM, MacDonald DJ, Simpson AH, Howie CR, Giesinger K (2016) Responsiveness and ceiling effects of the Forgotten Joint Score-12 following total hip arthroplasty. Bone Joint Res 5(3):87
Cao S, Liu N, Han W, Zi Y, Peng F, Li L et al (2017) Simplified Chinese version of the Forgotten Joint Score (FJS) for patients who underwent joint arthroplasty: cross-cultural adaptation and validation. J Orthop Surg Res 12(1):6
Kim MS, Koh IJ, Choi YJ, Lee JY, In Y (2017) Differences in patient-reported outcomes between unicompartmental and total knee arthroplasties: a propensity score-matched analysis. J Arthroplast 32(5):1453
Thienpont E, Opsomer G, Koninckx A, Houssiau F (2014) Joint awareness in different types of knee arthroplasty evaluated with the Forgotten Joint score. J Arthroplast 29(1):48
Thienpont E, Zorman D (2016) Higher forgotten joint score for fixed-bearing than for mobile-bearing total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 24(8):2641
Thienpont E, Vanden Berghe A, Schwab PE, Forthomme JP, Cornu O (2016) Joint awareness in osteoarthritis of the hip and knee evaluated with the ‘Forgotten Joint’ Score before and after joint replacement. Knee Surg Sports Traumatol Arthrosc 24(10):3346
Hiyama Y, Wada O, Nakakita S, Mizuno K (2016) Joint awareness after total knee arthroplasty is affected by pain and quadriceps strength. OrthopTraumatol Surg Res 102(4):435
Baker PN, Deehan DJ, Lees D, Jameson S, Avery PJ, Gregg PJ et al (2012) The effect of surgical factors on early patient-reported outcome measures (PROMS) following total knee replacement. J Bone Joint Surg (Br) 94(8):1058
Strickland LH, Hamilton TW, Jenkinson CC, Murray DW, Pandit HG (2016) Patient-reported outcome measure for early postoperative recovery following lower limb arthroplasty: a systematic review. J Arthroplast 31(12):2933
Landis JR, Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics 33(1):159
Acknowledgments
Not applicable.
Funding
The authors and institute did not receive any funding for the study.
Author information
Authors and Affiliations
Contributions
WYC charted scores and data. QJL analyzed and interpreted data and wrote the manuscript. YCW contributed ideas in methodology and discussion. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Approval from the institutional review board and consent from participants have been obtained for the study.
Consent for publication
The manuscript is not under consideration by another journal, and it has not been previously published. In consideration of the Knee Surgery & Related Research reviewing and editing our submission, the authors convey all copyright ownership to the Knee Surgery & Related Research.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Lee, Q., Chang, W.E. & Wong, Y. Forgotten Joint Score for early outcome assessment after total knee arthroplasty: Is it really useful?. Knee Surg & Relat Res 32, 37 (2020). https://doi.org/10.1186/s43019-020-00049-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43019-020-00049-0