Abstract
Background
To assess the Nickel sensitizing potential of total knee arthroplasty (TKA), explore the relationship between hypersensitivity and clinical outcomes, and evaluate the utility of skin patch testing pre- and/or postoperatively.
Materials and methods
A literature search was performed through EMBASE, Medline and PubMed databases. Articles were screened independently by two investigators. The level of evidence of studies was assessed using the Oxford Centre for Evidence-Based Medicine Criteria and the quality evaluated using the Methodological Index for Non-randomized Studies and Cochrane risk-of-bias tools.
Results
Twenty studies met the eligibility criteria, reporting on 1354 knee arthroplasties. Studies included patients undergoing primary or revision TKA, pre- and/or postoperatively, and used patch testing to identify Nickel hypersensitivity. Prevalence of Nickel hypersensitivity ranged from 0% to 87.5%. One study compared the prevalence of Nickel hypersensitivity in the same patient group before and after surgery and noted newly positive patch test reactions in three patients (4.2%). Three studies reported lower prevalence of Nickel hypersensitivity in postoperative patients compared to preoperative ones. Seven studies suggested that hypersensitivity might cause adverse clinical outcomes, but six did not support any relationship. Seven studies recommended preoperative patch testing in patients with history of metal allergy, and nine concluded that testing may be valuable postoperatively.
Conclusions
Patients undergoing TKA with no prior history of metal hypersensitivity do not seem to be at an increased risk of developing Nickel hypersensitivity, and there is conflicting evidence that patients with pre-existing hypersensitivity are more likely to experience adverse outcomes. Patch testing remains the most commonly used method for diagnosing hypersensitivity, and evidence suggests preoperative testing in patients with history of metal allergy to aid prosthesis selection, and postoperatively in patients with suspected hypersensitivity once common causes of implant failure have been excluded, since revision with hypoallergenic implants may alleviate symptoms.
Similar content being viewed by others
Background
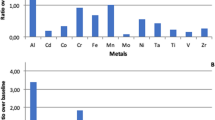
The reported prevalence of metal hypersensitivity in the general population ranges from 10 to 15% [1]. Nickel hypersensitivity is the most common, followed by Chromium and Cobalt, with approximately 14% of the general population having cutaneous sensitivity to Nickel [1]. The prevalence is reported to be four times more prevalent in females [2] and in certain occupations such as hairdressing, catering and bar work [3, 4]. Total knee arthroplasty (TKA) implants are typically composed of Nickel, Cobalt, Chromium, Molybdenum, Zirconium and Titanium alloys [5], and it has been suggested that patients could develop hypersensitivity reactions to these metals and associated complications postoperatively [6]. In total hip arthroplasty (THA), the prevalence of metal hypersensitivity has been reported to be approximately 25% in patients with well-functioning implants and up to 60% in those with failed or poorly functioning implants [5]. Similarly, the reported prevalence of metal hypersensitivity in TKA patients with stable implants is 44%, and 57% in those with loosened implants [7]. However, it remains uncertain whether the relationship between sensitization and implant failure is cause or effect.
Patients with metal hypersensitivity can present in a similar way to joint infection [1, 8]. Symptoms may include persistent pain, swelling and stiffness, with the onset of symptoms occurring between 2 months and 2 years following primary TKA [1, 9]. The patient may develop localized dermatitis, effusions, and reduced range of motion [8, 10]. More generalized eczematous reactions, though less common, can occur [11]. Radiography is typically unremarkable but might demonstrate periprosthetic osteolysis or implant loosening [12].
Metal hypersensitivity is a diagnosis of exclusion once more common causes of implant failure, such as infection and aseptic loosening, have been ruled out [10, 13]. Currently, there is no established or reliable test for detecting metal hypersensitivity, although skin patch testing (PT) is often employed due to ease of application, widespread availability, breadth of evaluation, and rapidity of results [9, 10, 14]. However, there is a lack of consensus over the clinical utility of patch testing patients with TKA [6, 10].
Since metal hypersensitivity occurs most frequently from exposure to Nickel, this systematic review was performed to collate and analyze the current literature on Nickel hypersensitivity in patients undergoing TKA. Previous review articles [1, 5, 6, 9, 10, 13,14,15,16,17,18,19] have been published providing an overview of metal hypersensitivity in total joint arthroplasty, but the current review focuses specifically on Nickel hypersensitivity in TKA patients as well as the usefulness of patch testing. The aims of the study were to evaluate: (1) the Nickel sensitizing potential of TKA, (2) the relationship between Nickel hypersensitivity and clinical outcomes and (3) the utility of skin patch testing in TKA patients pre- and/or postoperatively.
Materials and methods
This review was conducted in accordance with the 2020 Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) guidelines [20].
Eligibility criteria
Clinical studies determining the prevalence of Nickel hypersensitivity by patch testing patients with total knee arthroplasty, pre- and/or postoperatively, were included. Studies which also involved patients undergoing orthopedic interventions other than TKA were not excluded, provided that an appropriate number of TKA patients were included. Full-text articles had to be available and published in English or with translation freely available. Case reports, review articles, conference abstracts and surveys were excluded.
Search strategy
A comprehensive electronic search strategy utilizing a combination of Medical Subject Heading (MeSH)-terms and keywords was developed by one author (CP) and refined with the help of the Department Librarian (PA). The EMBASE and Medline databases were searched using the Healthcare Database Advance Search (HDAS) platform and extended to the native PubMed database, identifying literature from inception until September 2021. The line-by-line strategy run in HDAS and PubMed is outlined in Supplementary Material 1 and Supplementary Material 2, respectively. The only limitation to the search strategy was the ‘search field’, restricted to title and abstract, ensuring the literature search was sensitive and yielded all articles meeting the eligibility criteria.
To supplement the electronic search, a detailed review of the reference lists of the final studies included in the systematic review and in review articles on the same or similar topic was performed. Finally, a search of the grey literature on OpenGrey was performed to identify any published or ongoing research.
Screening
Potentially eligible studies were identified by screening the titles and abstracts of all articles retrieved from the search. The eligibility of each full-text article was then assessed for inclusion. Each stage was performed independently by two investigators (CP, HF), and any inconsistencies were discussed until consensus obtained. Disagreements at either stage were resolved by the senior author (DHS).
Data extraction/Analysis
The following data were extracted from the included studies:
-
Study characteristics (e.g. author, year, country, etc.)
-
Patient characteristics (e.g. sample size, average age, percentage of females etc.)
-
Type of TKA implant (i.e. metallic composition)
-
Details of patch testing (i.e. composition, timing)
-
Prevalence of Nickel hypersensitivity (i.e. number of patients, percentage of population)
-
Relevant clinical results (e.g. complications, implant status, further management etc.)
-
Main conclusions and recommendations
A data collection table in Microsoft Excel was designed by one author (CP) to display the information extracted from each eligible study.
Owing to heterogeneity in study design, participants, interventions and outcome measures, a quantitative meta-analysis was not appropriate.
Methodological quality assessment
Levels of evidence (LE) were assessed using the Oxford Centre for Evidence-Based Medicine (OCEBM) framework [21].
The quality of observational studies was independently assessed by two authors (CP, HF) using the Methodological Index for Non-randomized Studies (MINORS) tool [22]. The ideal global score was 16 for non-comparative studies and 24 for comparative studies.
Any randomized controlled trials were scored using the revised Cochrane risk-of-bias tool for randomized trials (RoB 2) [23].
The assessments provided an overall impression of each study but were not used to weight any studies in the analysis.
Results
Search results
The initial search performed through the EMBASE, Medline and PubMed databases identified 4002 records, of which 1695 records remained after deduplication. Of these, 1666 were excluded after screening titles and abstracts. Eight additional studies were identified by searching the reference lists of articles on the same topic, and no studies were identified by performing a search of the grey literature. As a result, 37 full-text articles were assessed for eligibility for inclusion, of which 17 were excluded (Fig. 1). Twenty studies were deemed eligible for inclusion in the review.
Quality assessment
Nineteen observational studies were included, four having a cohort study design with LE of III [24,25,26,27], and 15 being either case-control or case-series, with LE of IV [7, 28,29,30,31,32,33,34,35,36,37,38,39,40,41]. The average MINORS score was 9.75 and 14.29 for non-comparative and comparative observational studies respectively. There was one randomized-controlled trial (RCT) with LE of II [42] (Table 1).
Study characteristics
Details of the characteristics of each individual study are shown in Table 2.
The 20 studies included a total of 1354 TKAs, with an average of 68 knees per study. Amongst the studies which provided the mean age of all the participants involved (three studies with missing data [25, 26, 28]), the average age was 63.1 years (range, 11–96). The average proportion of females was 70% (two studies with missing data [25, 28]).
Patient characteristics
All patients underwent primary or revision TKA, with the other study participants comprising either control groups (e.g. no implant) or undergoing a different surgical procedure, such as THA. Fifteen studies [7, 25, 26, 30,31,32,33, 35,36,37,38,39,40,41,42] recorded the type of TKA implant used, with 13 noting the metallic composition of the prosthesis [7, 25, 26, 30,31,32,33, 35,36,37,38,39, 42]. The remaining five studies did not clearly document the type of implant used [24, 27,28,29, 34]. The characteristics of each individual patient group, including sample size, mean age, percentage of females, and implant type, are outlined in Table 3.
Patch testing
All 20 studies used patch testing to identify metal hypersensitivity. Details, including the composition and timing of testing in each study, are outlined in Table 4. The substances applied in the patch test, including the precise concentration of Nickel antigen, were documented in 18 studies (Table 4). Thirteen studies used Nickel Sulphate 5% [7, 25,26,27,28,29,30, 32, 36, 38,39,40, 42], one used Nickel Sulphate 2.5% [33], and two used both 2.5% and 5% [24, 34]. Three studies did not record the concentration of Nickel Sulphate used [35, 37, 41], while one did not document any of the substances used [31].
In four studies [26, 27, 30, 42], the same group of participants underwent patch testing before and after surgery. Four studies [7, 24, 28, 34] performed patch testing on one cohort of patients preoperatively and on a different cohort postoperatively. In ten studies [25, 29, 31, 33, 35,36,37,38,39,40], patients were patch tested only postoperatively, whilst in two [32, 41] patch testing was performed only preoperatively. The reported time until patch testing was performed postoperatively ranged from 3 months [29] to 16 years [25], but five studies [34,35,36,37, 39] did not record when the postoperative patch testing was performed.
Prevalence of Nickel hypersensitivity
The prevalence of Nickel hypersensitivity in the individual populations of each study together with relevant clinical outcomes, such as complications, implant status, and further management, is summarized in Table 5. The prevalence of Nickel hypersensitivity across the studied populations ranged from 0% [7, 26, 37] to 87.5% [28]. Four studies [26, 27, 30, 42] analyzed the prevalence in the same patient group before and after surgery. One study [30] noted that three patients (4.2%) who tested negative initially developed a newly positive reaction to Nickel after their operation. One study [26] noted that no patients had developed a newly positive reaction compared to their preoperative baseline. One study [27] did not record a significant increase in prevalence following surgery and another [42] noted that two patients had developed ‘doubtful’ patch test reactions.
Four studies [7, 24, 28, 34] compared the prevalence in different patient groups pre- and postoperatively, and in three of these [24, 28, 34], a lower prevalence was noted in the postoperative cohort. Compared to a control group comprising patients without implants, one study [7] reported a lower prevalence of Nickel hypersensitivity in patients with stable TKA, but a higher prevalence in patients with loosened TKA. Ten studies [25, 29, 31, 33, 35,36,37,38,39,40] performed patch testing only postoperatively and the prevalence ranged from 7.7% [38] to 83.3% [25].
Study conclusions and recommendations
Three main themes were commented on: the sensitizing potential of TKA, the relationship between metal hypersensitivity and adverse clinical outcomes, and the utility of patch testing, with the main conclusions summarized in Table 6.
Discussion
Nickel hypersensitivity and the implications on TKA is a controversial topic. This systematic review analyses the literature specifically focusing on Nickel hypersensitivity in patients undergoing TKA in order to assess the sensitising potential of TKA, the relationship with clinical outcomes, and the utility of skin patch testing.
Sensitizing potential of TKA
There was limited evidence to support the concept that implants used in TKA can elicit Nickel hypersensitivity in patients with no prior history of metal hypersensitivity. Only one study [30] which analyzed the prevalence of Nickel hypersensitivity in the same patient group before and after surgery noted that patients developed a newly positive reaction to Nickel after surgery, and this occurred in only three out of the 72 patients available for follow-up (4.2%). The other studies [26, 27, 42] which followed patients up after surgery did not find a significant increase in prevalence of Nickel hypersensitivity following operation, and three studies in the review [24, 28, 34] noted that Nickel hypersensitivity was in fact lower in postoperative patients with implants compared to preoperative patients without implants. Based on the evidence available, TKA implants do not appear to contribute to the development of Nickel hypersensitivity in patients with no prior history of metal allergy.
Nickel hypersensitivity and clinical outcomes
The literature evaluating the relationship between Nickel hypersensitivity and clinical outcomes was conflicting. Some studies in the review noted that patients with a positive patch test result to a metallic component of their implant developed eczema [39], joint loosening [24], recurrent pain [24, 27], and swelling [27]. They were also more likely to be dissatisfied [29], and a higher prevalence of Nickel hypersensitivity was reported in TKA patients with complications compared to those without [7, 37]. It is conceivable that these symptoms could have been attributable to hypersensitivity, since patients who subsequently had their prosthesis removed, or revised with hypoallergenic implants, experienced resolution of symptoms, whereas those who did not remained symptomatic [24, 28, 34, 35].
Given that up to 20% of patients are not satisfied with the outcome of TKA due to multifactorial reasons [43], it is difficult to ascribe these symptoms to Nickel hypersensitivity alone. Carlsson and Möller [25] followed patients with established preoperative metal allergy up to 16 years after implanting prostheses containing metal to which they were allergic and reported no dermatological or orthopedic complications attributable to contact allergy. Their findings are consistent with other studies which found no significant association between hypersensitivity and pain [29] or radiographic loosening [7, 40]. Furthermore, although Verma et al [39] noted that some patients with a positive patch test developed eczema lateral to the surgical incision, they were unable to correlate their findings, and there is evidence that cutaneous eruptions at this site can develop as a result of resection of the infrapatellar branch of the saphenous nerve when utilizing a medial parapatellar approach [44,45,46].
Patch testing
The literature did not support the routine use of preoperative patch testing in all patients undergoing TKA. The majority of studies which commented on the utility of preoperative testing [24, 26, 28, 31,32,33,34] suggested that surgeons should consider the overall clinical context, performing patch testing only in patients with a history of metal hypersensitivity, with Granchi et al. [7] reporting that TKA failure was four times more likely in this cohort of patients.
The use of a diagnostic algorithm for metal hypersensitivity in patients undergoing TKA has been proposed in previous articles [6, 9, 14, 15] (Fig. 2). Patients with a positive history of metal hypersensitivity, confirmed with a positive patch test, should be assumed to be hypersensitive to metal and the use of hypoallergenic implants should be considered.
Diagnostic algorithm for Nickel hypersensitivity in patients before total knee arthroplasty (TKA) (adapted from Mitchelson et al. [8])
Hypoallergenic TKA implants include coated implants (with Titanium Nitride or Zirconia Nitride), ceramic implants (oxidized Zirconium), pure Titanium implants, and all-polyethylene tibial components [19, 47]. Satisfactory short-to-medium-term outcomes have been demonstrated with these implants. However concerns exist over their longevity and clinical performance [19], so appropriate informed consent should be obtained and shared decision-making should be undertaken.
The evidence suggests that patch testing could be a valuable diagnostic tool postoperatively to screen for metal hypersensitivity in symptomatic patients following TKA. In patients presenting with recent onset of periprosthetic dermatitis, arthralgia, evidence of loosening, or radiolucent lines on radiographs, patch testing seems a reasonable option once other failure mechanisms such as infection, instability and malalignment have been excluded and inflammatory markers (CRP and ESR) and joint aspiration have yielded negative results [6, 14]. A treatment algorithm could be employed to assist with the management of such patients (Fig. 3). Patients with a positive patch test may have their symptoms treated medically (e.g. with topical steroids or NSAIDs [6]) or consider undergoing revision with a hypoallergenic implant. This should again involve discussion, shared decision-making and appropriate consenting.
Treatment algorithm for Nickel hypersensitivity in patients after total knee arthroplasty (TKA) (adapted from Mitchelson et al. [8])
Lymphocyte transformation testing (LTT) was performed in addition to patch testing in a number of studies included in the review [26, 28, 30,31,32,33, 35, 37, 41]. LTT detects metal hypersensitivity by measuring the ratio of lymphocyte proliferation in peripheral blood (that has been incubated for seven days) with an antigen present over lymphocyte proliferation with the antigen absent, which is referred to as the stimulation index [10, 48]. It has been suggested that LTT might be more suitable than patch testing as it is more sensitive, less subjective, and patch testing itself can induce metal hypersensitivity in previously non-sensitive patients [26, 28]. However, there are limitations to its large-scale application including cost [29, 42] and the need for specialized laboratories [24]. The role of LTT remains unclear but appears to be gaining support for its use in conjunction with PT when results are negative and allergy remains strongly suspected [33]. Taking synovial biopsies for histopathological analysis of adverse local tissue reactions to implant materials may further assist with diagnosis [19].
Patch testing remains the most commonly used investigation for diagnosing metal hypersensitivity [9, 14, 49]. It is simple, inexpensive, widely available, and may allow for screening of several metals [10, 48] but debate remains over the correlation between dermal reactions elicited by skin patch testing and deep-tissue sensitivity surrounding an implant [16]. Since the primary antigen-presenting cells responsible for contact dermatitis and implant-related hypersensitivity differ [10, 16], it is uncertain whether PT can reliably predict outcomes associated with total knee arthroplasty [6].
Limitations
This systematic review has several limitations. Firstly, all the included studies had low levels of evidence, with only one [42] scoring above III, based on the OCEBM. In addition, the quality of the studies was poor; none of the observational studies achieving an ideal global MINORS score and the only RCT [42] demonstrating a high risk of bias when assessed using the RoB 2 tool. Caution should therefore be exercised when interpreting and comparing the results of these studies.
Several of the articles analyzed groups of patients undergoing not only knee, but also other orthopedic interventions [24, 27, 30, 31, 34, 36, 37, 41], such as hip and shoulder arthroplasty. However, the results of patch testing in those participants were not stratified by operation, but only as a single patient cohort [24, 25, 27, 30, 31, 34, 36, 37, 50]. Given that specific types of implants, such as metal-on-metal hip prostheses, have a greater propensity to release metal ions and potentially induce hypersensitivity [5], or loosening as the result of a different mechanism from allergy [16], it is difficult to interpret the relationship between Nickel hypersensitivity and total knee arthroplasty in this context.
The utility of late patch test reading at day six after application has been documented [36] and it is possible that many of the studies which interpreted patch tests at day two or three might have missed late positive reactions or been interpreted as false-negative readings. The time until patch testing was performed postoperatively was also highly variable across the studies, and it is thought that shorter periods (e.g. six months) may be insufficient to detect new hypersensitivity reactions to implant components [51].
Conclusions
The current literature does not support the concept that patients undergoing TKA with no prior history of Nickel hypersensitivity are at an increased risk of developing hypersensitivity, and there is conflicting evidence that patients with established Nickel hypersensitivity are more likely to experience dermatological or orthopedic complications such as persistent pain, implant loosening or failure. Despite its limitations, cutaneous patch testing remains the most commonly used method for diagnosing Nickel hypersensitivity. The literature does not support routine patch testing of patients prior to TKA but does support performing this test in patients with a history of metal hypersensitivity. In those with a positive patch test, the choice of implant to use should be made on a case-by-case basis after discussion with the patient, as in the absence of more robust evidence, the careful selection of which device to implant may minimize the potential risk of complications related to metal hypersensitivity. Patients with a clinical presentation suggestive of Nickel hypersensitivity following TKA may benefit from patch testing only after the more common causes of pain, loosening and failure have been excluded, since revision surgery with hypoallergenic implants may alleviate symptoms. To further establish the relationship and importance of Nickel hypersensitivity in patients undergoing TKA, large-scale, appropriately designed studies will be required.
Availability of data and materials
All available data are provided. Additional data, if needed, may be made available from the corresponding author on reasonable request.
Abbreviations
- TKA:
-
Total knee arthroplasty
- THA:
-
Total hip arthroplasty
- PT:
-
Patch testing
- PRISMA:
-
Preferred Reporting Items for Systematic Review and Meta-Analysis
- MeSH:
-
Medical Subject Heading
- HDAS:
-
Healthcare Database Advance Search
- LE:
-
Levels of Evidence
- OCEBM:
-
Oxford Centre for Evidence-Based Medicine
- MINORS:
-
Methodological Index for Non-Randomized Studies
- RoB:
-
Risk of bias
- RCT:
-
Randomized-Controlled trial
- CRP:
-
C-Reactive Protein
- ESR:
-
Erythrocyte sedimentation rate
- LTT:
-
Lymphocyte transformation testing
References
Lachiewicz PF, Watters TS, Jacobs JJ. Metal Hypersensitivity and Total Knee Arthroplasty. J Am Acad Orthop Surg. 2016;24(2):106–12.
Lu LK, Warshaw EM, Dunnick CA. Prevention of Nickel Allergy: The Case for Regulation? Dermatol Clin. 2009;27(2):155–61.
Shum KW, Meyer JD, Chen Y, Cherry N, Gawkrodger DJ. Occupational contact dermatitis to nickel: experience of the British dermatologists (EPIDERM) and occupational physicians (OPRA) surveillance schemes. Occup Environ Med. 2003;60(12):954–7.
Fregert S. Occupational dermatitis in a 10-year material. Contact Dermatitis. 1975;1(2):96–107.
Hallab N, Merritt K, Jacobs JJ. Metal sensitivity in patients with orthopaedic implants. J Bone Joint Surg Am. 2001;83(3):428–36.
Akil S, Newman JM, Shah NV, Ahmed N, Deshmukh AJ, Maheshwari AV. Metal hypersensitivity in total hip and knee arthroplasty: Current concepts. J Clin Orthop Trauma. 2018;9(1):3–6.
Granchi D, Cenni E, Tigani D, Trisolino G, Baldini N, Giunti A. Sensitivity to implant materials in patients with total knee arthroplasties. Biomaterials. 2008;29(10):1494–500.
Baumann CA, Crist BD. Nickel allergy to orthopaedic implants: a review and case series. J Clin Orthop Trauma. 2020;11:S596-603.
Mitchelson AJ, Wilson CJ, Mihalko WM, Grupp TM, Manning BT, Dennis DA, et al. Biomaterial hypersensitivity: is it real? Supportive evidence and approach considerations for metal allergic patients following total knee arthroplasty. BioMed Res Int. 2015;2015:137287.
Teo WZW, Schalock PC. Metal Hypersensitivity Reactions to Orthopedic Implants. Dermatol Ther. 2017;7(1):53–64.
Yoshihisa Y, Shimizu T. Metal Allergy and Systemic Contact Dermatitis: An Overview. Dermatol Res Pract. 2012;2012:1–5.
Gupta R, Phan D, Schwarzkopf R. Total Knee Arthroplasty Failure Induced by Metal Hypersensitivity. Am J Case Rep. 2015;17(16):542–7.
Innocenti M, Vieri B, Melani T, Paoli T, Carulli C. Metal hypersensitivity after knee arthroplasty: fact or fiction? Acta Bio-Medica Atenei Parm. 2017;88(2S):78–83.
Faschingbauer M, Renner L, Boettner F. Allergy in Total Knee Replacement. Does It Exist?: Review Article. HSS J Musculoskelet J Hosp Spec Surg. 2017;13(1):12–9.
Granchi D, Cenni E, Giunti A, Baldini N. Metal hypersensitivity testing in patients undergoing joint replacement: a systematic review. J Bone Joint Surg Br. 2012;94(8):1126–34.
Middleton S, Toms A. Allergy in total knee arthroplasty: a review of the facts. Bone Jt J. 2016;98-B(4):437–41.
Toro G, De Cicco A, Braile A, Landi G, Schiavone Panni A. New insights on metal allergy in total joint arthroplasty. J Biol Regul Homeost Agents. 2020;34(5 Suppl. 1):125–30. IORS Special Issue on Orthopedics.
Pinson ML, Coop CA, Webb CN. Metal hypersensitivity in total joint arthroplasty. Ann Allergy Asthma Immunol. 2014;113(2):131–6.
Matar HE, Porter PJ, Porter ML. Metal allergy in primary and revision total knee arthroplasty: a scoping review and evidence-based practical approach. Bone Jt Open. 2021;2(10):785–95.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;29:n71.
OCEBM Levels of Evidence Working Group. The Oxford 2011 Levels of Evidence. Oxford Centre for Evidence-Based Medicine. http://www.cebm.net/index.aspx?o=5653 (date last Accessed 26 May 2021).
Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological index for non-randomized studies ( MINORS ): development and validation of a new instrument: Methodological index for non-randomized studies. ANZ J Surg. 2003;73(9):712–6.
Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;28:l4898.
Atanaskova Mesinkovska N, Tellez A, Molina L, Honari G, Sood A, Barsoum W, et al. The Effect of Patch Testing on Surgical Practices and Outcomes in Orthopedic Patients With Metal Implants. Arch Dermatol. 2012;148(6). Available from: http://archderm.jamanetwork.com/article.aspx?doi=10.1001/archdermatol.2011.2561. [Cited 2021 Oct 25].
Carlsson A, Möller H. Implantation of orthopaedic devices in patients with metal allergy. Acta Derm Venereol. 1989;69(1):62–6.
Kitagawa A, Chin T, Tsumura N, Iguchi T. Metal sensitivity in patients before and after total knee arthroplasty (TKA): comparison between ceramic surfaced oxidized zirconium and cobalt-chromium implants. Hypersensitivity. 2013;1(1):3.
Kręcisz B, Kieć-Świerczyńska M, Chomiczewska-Skóra D. Allergy to orthopedic metal implants - a prospective study. Int J Occup Med Environ Health. 2012;25(4):463–9.
Carossino AM, Carulli C, Ciuffi S, Carossino R, ZappoliThyrion GD, Zonefrati R, et al. Hypersensitivity reactions to metal implants: laboratory options. BMC Musculoskelet Disord. 2016;17(1):486.
Desai MM, Shah KA, Mohapatra A, Patel DC. Prevalence of metal hypersensitivity in total knee replacement. J Orthop. 2019;16(6):468–72.
Frigerio E, Pigatto PD, Guzzi G, Altomare G. Metal sensitivity in patients with orthopaedic implants: a prospective study. Contact Dermatitis. 2011;64(5):273–9.
Guenther D, Thomas P, Kendoff D, Omar M, Gehrke T, Haasper C. Allergic reactions in arthroplasty: myth or serious problem? Int Orthop. 2016;40(2):239–44.
Innocenti M, Carulli C, Matassi F, Carossino AM, Brandi ML, Civinini R. Total knee arthroplasty in patients with hypersensitivity to metals. Int Orthop. 2014;38(2):329–33.
Sasseville D, Alfalah K, Savin E. Patch Test Results and Outcome in Patients with Complications from Total Knee Arthroplasty: A Consecutive Case Series. J Knee Surg. 2021;34(03):233–41.
Tam I, Yu J, Ko LN, Schalock PC. Clinical factors before or after device implantation in predicting metal hypersensitivity reactions: a retrospective study. Contact Dermatitis. 2020;83(5):398–407.
Thomas P, von der Helm C, Schopf C, Mazoochian F, Frommelt L, Gollwitzer H, et al. Patients with intolerance reactions to total knee replacement: combined assessment of allergy diagnostics, periprosthetic histology, and peri-implant cytokine expression pattern. BioMed Res Int. 2015;2015:910156.
Thomas B, Kulichova D, Wolf R, Summer B, Mahler V, Thomas P. High frequency of contact allergy to implant and bone cement components, in particular gentamicin, in cemented arthroplasty with complications: usefulness of late patch test reading: gentamicin allergy in complicated arthroplasty? Contact Dermatitis. 2015;73(6):343–9.
Thomas P, Ständer S, Stauner K, Schraml A, Banke IJ, Gollwitzer H, et al. Arthroplasty patients and nickel sensitization: what do patch test and lymphocyte transformation test tell us. Semin Arthroplasty. 2013;24(4):261–4.
Treudler R, Simon JC. Benzoyl peroxide: is it a relevant bone cement allergen in patients with orthopaedic implants? Contact Dermatitis. 2007;57(3):177–80.
Verma SB, Mody B, Gawkrodger DJ. Dermatitis on the knee following knee replacement: a minority of cases show contact allergy to chromate, cobalt or nickel but a causal association is unproven. Contact Dermatitis. 2006;54(4):228–9.
Webley M, Kates A, Snaith ML. Metal sensitivity in patients with a hinge arthroplasty of the knee. Ann Rheum Dis. 1978;37(4):373–5.
Zeng Y, Feng W, Li J, Lu L, Ma C, Zeng J, et al. A prospective study concerning the relationship between metal allergy and post-operative pain following total hip and knee arthroplasty. Int Orthop. 2014;38(11):2231–6.
Lützner J, Hartmann A, Dinnebier G, Spornraft-Ragaller P, Hamann C, Kirschner S. Metal hypersensitivity and metal ion levels in patients with coated or uncoated total knee arthroplasty: a randomised controlled study. Int Orthop. 2013;37(10):1925–31.
Scott CEH, Howie CR, MacDonald D, Biant LC. Predicting dissatisfaction following total knee replacement: a prospective study of 1217 patients. J Bone Joint Surg Br. 2010;92(9):1253–8.
Verma SB, Mody BS. Explaining a hitherto nameless condition: ‘SKINTED.’ Clin Exp Dermatol. 2009;34(7):e465–6.
Nazeer M, Ravindran R, Katragadda BC, Muhammed EN, Rema DTJ, Muhammed MN. SKINTED: A Rare Complication After Total Knee Arthroplasty. Arthroplasty Today. 2020;6(4):1028–32.
Sharquie KE, Noaimi AA, Alaboudi AS. Neuropathy Dermatitis following Surgical Nerve Injury. Case Rep Dermatol Med. 2011;2011:1–3.
Ajwani SH, Charalambous CP. Availability of Total Knee Arthroplasty Implants for Metal Hypersensitivity Patients. Knee Surg Relat Res. 2016;28(4):312–8.
Thyssen JP, Menné T, Schalock PC, Taylor JS, Maibach HI. Pragmatic approach to the clinical work-up of patients with putative allergic disease to metallic orthopaedic implants before and after surgery: Clinical work-up of patients with orthopaedic implant failure. Br J Dermatol. 2011;164(3):473-8.
Schalock PC, Menné T, Johansen JD, Taylor JS, Maibach HI, Lidén C, et al. Hypersensitivity reactions to metallic implants - diagnostic algorithm and suggested patch test series for clinical use. Contact Dermatitis. 2012;66(1):4–19.
Elves MW, Wilson JN, Scales JT, Kemp HB. Incidence of metal sensitivity in patients with total joint replacements. BMJ. 1975;4(5993):376–8.
Shanmugham HA, Handa S, De D, Dhillon MS, Aggarwal S. An observational study to determine the sensitizing potential of orthopedic implants. Indian J Dermatol Venereol Leprol. 2021;87(6):826-30.
Acknowledgements
The authors would like to thank Ms. Irrum Afzal, Research Manager at the Academic Surgical Unit of the South West London Elective Orthopedic Centre (SWLEOC), for her guidance and contribution to the research process behind this systematic review. We are also grateful to Ms. Potenza Atiogbe, Multiprofessional Education and Library Services Manager at Epsom and St Helier’s NHS Trust, for her support and help in searching the literature and obtaining some of the publications used in this work.
Funding
This research did not receive any specific grant from any funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
CP: Conception, design, acquisition, analysis, interpretation of data, drafting, submission; HF: Conception, acquisition, analysis, interpretation of data, drafting; VA: Conception, drafting, oversight; NDC: Drafting, oversight; DK: Conception, oversight; DHS: Conception, design, drafting, oversight. Each author has approved the submitted version and has agreed both to be personally accountable for the author's own contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even ones in which the author was not personally involved, are appropriately investigated, resolved, and the resolution documented in the literature.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Search strategy used in HDAS.
Additional file 2.
Search strategy used in PubMed.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Peacock, C.J.H., Fu, H., Asopa, V. et al. The effect of Nickel hypersensitivity on the outcome of total knee arthroplasty and the value of skin patch testing: a systematic review. Arthroplasty 4, 40 (2022). https://doi.org/10.1186/s42836-022-00144-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s42836-022-00144-5