Abstract
Background
Chronic right-ventricular (RV) pacing can exacerbate heart failure in patients with a low ejection fraction (EF). There is little information on the effects of diastolic dysfunction (DD) in patients with preserved EF undergoing permanent pacemaker (PPM) placement. We aimed to investigate the clinical outcomes in these patients.
Methods
This multicenter, retrospective analysis of PPM use in Chonnam, South Korea, included all patients with preserved EF undergoing transvenous PPM implantation for atrioventricular blockage from 2017 to 2019. Patients were divided into two groups according to DD, which were assessed by including mitral flow velocities (E′ velocity, E/E′ ratio), peak velocity of the tricuspid regurgitant, and left atrial maximum volume index. Composite outcomes were defined as (1) cardiovascular death, and (2) hospitalization by heart failure during the follow-up period.
Results
One hundred sixty-seven patients (66 men; overall mean age, 75.3 ± 11.9 years) were divided into two groups: 125 normal versus 42 DD. Compared with normal subjects, the DD group included older patients (mean age, 79.1 ± 9.9 vs. 74.0 ± 12.3; p = 0.016), and had longer paced QTc interval (pQTc, 168.5 ± 20.1 vs. 159.1 ± 16.3 ms; p < 0.001). Fifteen patients were hospitalized and two died. In a Cox proportional regression analysis, DD (hazard ratio [HR], 7.343; 95% confidence interval [CI], 2.035–26.494; p = 0.002) and pQRSd (HR, 1.046; 95% CI, 1.004–1.091; p = 0.033) were independent predictors of composite outcomes.
Conclusion
In patients with DD, RV pacing raised the risk of pacing-induced heart failure despite preserved left-ventricular function. Thus, patients with DD should be monitored intensively.
Similar content being viewed by others
Introduction
Chronic right-ventricular (RV) pacing can cause or worsen heart failure and increase cardiac mortality in patients with a low cardiac ejection fraction (EF) [1,2,3,4]. Therefore, physiologic interventions such as biventricular pacing were recommended in patients with reduced EF in need of ventricular pacing [5, 6]. However, it is controversial as to whether RV pacing is effective in patients with a preserved EF [7, 8]. Chronic RV pacing has shown heterogeneous clinical outcomes in those patients. In addition, the impact of RV pacing on clinical outcomes in patients with and without diastolic dysfunction (DD) has not been explored. We aimed to investigate the clinical outcomes during a long-term follow-up among patients undergoing permanent pacemaker (PPM) placement according to the presence or absence of DD.
Methods
Study population
This was a multicenter, retrospective analysis of PPM use from two tertiary centers in Gwang Ju, South Korea. All patients aged over 18 years undergoing de novo transvenous pacemaker implantation for a persistent atrioventricular block at Chosun University Hospital and Chonnam National University Hospital from January 2017 to December 2019 were recruited. Patients were included if they underwent dual-chamber PPM implantation, in whom the left-ventricular ejection fraction (LVEF) was ≥ 50% and ventricular pacing > 40%. The exclusion criteria were atrial fibrillation or flutter, severe valvular heart disease, cardiomyopathy, congenital heart disease, or terminal conditions with a life expectancy of < 1 year. The patients were divided into two groups according to their DD. Detailed histories and examinations of all patients were recorded at baseline. Their clinical characteristics, 12-lead electrocardiogram (ECG), and echocardiography parameters were evaluated. All patients enrolled in this study were seen as outpatients every 3–6 months and clinical follow-up was performed with respect to hospitalization or cardiac death caused by heart failure. The primary outcome was a composite of cardiovascular death (i.e., sudden death and pump failure death) or HF hospitalization during follow-up period. Pacing-induced cardiomyopathy (PICM) was defined as greater than 10% decrease in LVEF, with a resultant LVEF less than 50%, as previously reported [9].
PPM implantation
All patients received commercially available transvenous PPM systems approved by the Korean Food & Drug Administration. Active can devices and leads from three manufacturers (Abbott, St. Paul, MN, USA; Medtronic, Minneapolis, MN, USA; Boston, St Paul, MN, USA) were used. Pacemaker leads were inserted through the axillary vein using standard implantation techniques. Implantation procedures were performed through a pectoral approach. The RV leads were positioned in the RV apex or RV septum at the operator’s discretion. Electrical measurements were accepted with an R wave > 5 mV and a pacing threshold < 1.5 V. Once satisfactory testing results had been obtained, ventricular lead positions were confirmed by fluoroscopy in both left anterior oblique and right anterior oblique views (to cover the cardiac septum, not the free wall) and by ECG characteristics. Within 24 h, baseline ECG parameters were those acquired closest to PPM implantation; data were acquired at regular intervals (at least 6 months), and the pacing burdens (atrial and ventricular pacing percentages) were recorded at the time of follow-up.
Echocardiography
All patients underwent comprehensive echocardiography evaluations after PPM implantation within 7 days. Images were obtained with a standard ultrasound machine using a 2.5 MHz phased array transducer (Vivid 9; GE Vingmed, Horton, Norway). Standard techniques were used to obtain M mode, two-dimensional, and Doppler measurements following the American Society of Echocardiography guidelines. The LVEF was measured using the modified Simpson’s biplane method, and the LV stroke volume was calculated. Mitral inflow was assessed in an apical four-chamber view using pulsed wave Doppler ultrasonography. Diastolic functions were also evaluated using color tissue Doppler imaging (TDI) [10]. These were assessed by including mitral flow velocities, a mitral annular septal E′ velocity of < 7 cm/, an E/E′ ratio of > 14, peak velocity of the tricuspid regurgitant (TR) jet > 2.8 m/s and left atrial maximum volume index (LAVI) > 34 ml/m2. LV DD was judged to be present if more than half of the available parameters met these cutoff values. Also, we compared clinical outcomes by the earlier 2009 DD criteria. DD was also graded as follows [11]. Normal pattern: E/A, > 0.8; deceleration time (DT), 160–240 ms; isovolumic relaxation time (IVRT), 70–90 ms; E/E′, < 10. Grade I: EA, < 0.8; DT, > 240 ms; IVRT, > 100 ms; E/ E′ < 10. Grade II: E/A, 0.8–2.0; DT, 160–240 ms; IVRT, 70–100 ms; E/E′, 10–14. Grade III: E/A, > 2; DT, < 160 ms; IVRT, < 70 ms; E/E′, > 14.
Statistical analysis
Baseline characteristics are summarized as the mean ± standard deviation for continuous variables, and as frequencies with percentages for categorical variables. We compared the results within a group by testing for normality with the Kolmogorov–Smirnov test. Comparisons between the two groups were analyzed by Student’s t test or the Mann–Whitney nonparametric U test for continuous variables, and the Chi squared test for categorical variables, as appropriate. A Cox proportional regression model was used to determine the predictors of composite clinical outcomes, and a receiver operating characteristic (ROC) curve was plotted to identify the cutoff values for the occurrence of composite clinical outcomes using the area under the curve (AUC) with Youden’s approach in Medcalc (v. 20.0; https://www.medcalc.org/calc/). All statistical tests were two-sided and were performed using IBM SPSS Statistics (v. 24.0; IBM Corp., Armonk, NY, USA). p values < 0.05 were considered significant and the results are presented as the hazard ratio (HR) and 95% confidence.
Results
Study population
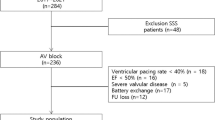
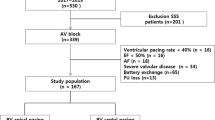
Figure 1 shows the patient flow diagram for this study. Among all patients, 167 with atrioventricular block (66 men, 39.5%; overall mean age 75.3 ± 11.9 years) were included. They were divided into two groups: 42 with DD versus 125 normal. The participants’ baseline clinical characteristics are shown in Table 1. Patients in the DD group were older (79.1 ± 9.9 vs. 74.0 ± 12.3 y; p = 0.016). There were no significant differences in gender or cardiovascular risk factor (diabetes mellitus, hypertension, dyslipidemia, cerebrovascular accident, coronary artery disease). The LVEF was not different between the groups at baseline (58.1 ± 10.2 vs. 58.1 ± 8.9, p = 0.992). Diastolic function variables were greater in the DD group, as expected. Paced QRS duration (pQRSd) was not different between the two groups; however, the paced QTc (pQTc) interval was prolonged in the DD group (516.8 ± 39.3 in the DD vs. 498.3 ± 45.4 in the normal group; p < 0.001).
Device-related parameters
Table 2 lists the device-related characteristics. No complications occurred during PPM implantation. The average P and R wave amplitudes, pacing thresholds, and impedance values were not different between the groups. The percentage of ventricular pacing > 90% was not statistically different between groups and the pacing site was not significantly associated with DD.
Clinical outcomes
The clinical outcomes are listed in Table 3. Over a median of 31-month follow-up, the overall incidence of PPM-induced heart failure was 10.1% (15 hospitalizations and two cardiac deaths). Their ejection fraction was 38.05 ± 7.65%, which were consistent with pacing-induced cardiomyopathy at follow-up echocardiography. More patients with DD were admitted to hospital for heart failure (31.0% vs. 3.2%; p = 0.001). Cox proportional regression analysis was applied to identify the predictors of composite outcomes (Table 4) (Fig. 2). The diastolic dysfunction (HR, 7.343; 95% CI, 2.035–26.494; p = 0.002) and paced QRS duration (pQRSd: HR, 1.046; 95% CI, 1.004–1.091; p = 0.033) were independent predictors of composite clinical outcomes. Most of the patients were classed as having Grade I DD (Fig. 3a) according to the 2009 guideline. On the other hand, the greater the number of DD variables (2016 guideline), the higher the probability of composite clinical outcomes (Fig. 3b). ROC curve analysis (AUC area, 0.721; 95% CI, 0.610–0.833; p = 0.004) showed that a pQRSd of 168 ms had a 75.0% sensitivity and a 64.2% specificity for predicting the occurrence of composite clinical outcomes (Fig. 4).
Discussion
Since the beginning of pacing therapy in 1958, the RV is still the established site for undergoing PPM insertion [1]. Although RV pacing can contract both ventricles relatively effectively, this could induce ventricular dyssynchrony and detrimental hemodynamic effects. In turn, this might lead to progressive adverse remodeling at cellular and heart chamber levels with resultant deterioration in ventricular function [12]. Chronic RV pacing can cause or worsen heart failure and increase cardiac mortality [1,2,3,4]. The adverse clinical outcomes of prolonged RV apical pacing in some patients are increasingly recognized, which ultimately might result in fatal pacing-induced cardiomyopathy, which occurred in 16.1% of patients in a study conducted in South Korea [13]. Here, the overall incidence of pacemaker-induced heart failure was 10.1% during a median of 31-month follow-up.
Earlier studies have shown that a lower EF is a statistically significant factor for the development of PICM [3, 4]. Physiologic pacing is recommended in patients with reduced EF and a high degree of atrioventricular blockage in need of ventricular pacing. However, this method is controversial in patients with preserved EF. One interesting finding of our study is that DD could affect pacemaker-induced heart failure in patients with preserved LV function. Diastolic function is an equally vital component of the cardiac cycle, which is closely linked with systolic function. It indicates a functional abnormality of diastolic relaxation-linked filling or distensibility of the LV, which reflects abnormal mechanical properties of this ventricle [14]. When DD already exists, the additional stress provoked by RV pacing might induce further functional abnormalities, such as electromechanical delay caused by a pacing-induced left bundle branch block pattern and regional perfusion defects [15]. Therefore, it is possible that RV pacing contributes to a further degree of LV systolic dysfunction and more clinical heart failure (HF).
In our study, DD was evaluated by four variables (E′, E/E′ ratio, LAVI, and TR velocity) as recommended by the 2016 American Society of Echocardiography/European Association of Cardiovascular Imaging guidelines, which are simpler and more practical indicators than the 2009 guidelines. In addition to mitral flow pattern and mitral annular velocity, the updated guidelines include left atrium chamber size and TR gradient, which predicting the risk of developing HF on long-term RV pacing in patients with preserved LV function in our study (Fig. 2). The greater the sum of DD variables, the higher the probability of pacemaker-induced HF (Fig. 3b). This is particularly relevant in the population paced for CAVB who are usually older and who will have an age-related decline in diastolic function. According to the 2009 guidelines, most of the elderly patients were assigned to Grade I DD, (Fig. 3a). However, in the revised 2016 guidelines, higher DD variables affect composite clinical outcomes adversely, so it is possible to identify high-risk patients.
In addition, the pQRSd is a known risk factor for pacemaker-induced HF [13, 16,17,18]. Therefore, patients with a longer pQRSd are at higher risk. Khurshid et al. also proposed that a pQRSd of 150 ms was a sensitive indicator for such HF [16]. In our study, ROC analysis showed that a pQRSd of 168 ms had a 75.0% sensitivity and a 64.2% specificity for predicting the occurrence of PPM-induced HF. These findings show that patients with a higher pQRSd (> 168 ms) must be monitored intensively with more periodic echocardiography. This modifiable factor helped to decrease the incidence of PPM-induced HF and efforts should be directed toward minimizing it, such as biventricular pacing and conduction system pacing. The use of biventricular pacing is well accepted for the treatment of patients with systolic HF and prolonged QRS duration, with several clinical trials performed over the past 20 years demonstrating improvements in morbidity and mortality [19]. Unfortunately, the effectiveness of CRT in patients with CAVB and preserved LV function is questionable [7]. Recently, utility of His-Purkinje system pacing including his bundle pacing and left bundle branch pacing was shown to preserve cardiac synchrony [20]. Theoretically, this will reduce the odds that dyssynchrony will occur. His bundle pacing may be beneficial in those with an anticipated high percent of RV pacing and possibly even those who have an indication for cardiac resynchronization therapy (CRT) such as a left bundle branch block [21, 22]. However, HBP is limited by poor ventricular sensing, elevated acute and chronic pacing thresholds necessitating lead reintervention and rapid battery replacement, and failure to reliably normalize the QRS complex in patients with bundle branch block [23]. On the contrary, left bundle branch pacing might be able to overcome more distal conduction disease. It is a feasible and effective method for left bundle branch block in patients with nonischemic cardiomyopathy [24]. However, long-term clinical outcomes of left bundle branch pacing are needed in future randomized clinical trials.
Limitations
This study included a relatively small number of patients in the two referral centers in South Korea, which might limit generalization of the results. First, the small study size and low incidence rate made it difficult to identify the real impact of DD. Second, the nonrandomized nature of the registry data could have resulted in selection bias. Because this was a multicenter observational registry, the influence of different physicians on clinical decision making might have also influenced the clinical variables associated with HF. Third, the primary outcome was a composite of cardiovascular (CV) death (i.e. ,sudden cardiac death and pump failure death) or HF hospitalization during follow-up period. Because follow-up echocardiography was not performed in all patients, we did not check the individual changes in patients’ LVEF. Also, 9 patients who were hospitalized or died from other causes (i.e., 2 sepsis, 1 pacemaker pocket infection, 1 leukemia, 1 lung cancer, 1 rectal cancer, 1 fracture of hand, and 2 coronary artery disease) were excluded from the outcome analysis.
Conclusions
In patients with DD, RV pacing raised the risk of pacing-induced HF during a median of 31 months of follow-up despite preserved LV function. Our results suggest that the patients with DD undergoing PPM placement should be monitored intensively.
Availability of data and materials
The datasets during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- DD:
-
Diastolic dysfunction
- DT:
-
Deceleration Time
- ECG:
-
Electrocardiogram;
- EF:
-
Ejection fraction
- IVRT:
-
Isovolumic relaxation time
- LAVI:
-
Left atrial maximum volume index
- LV:
-
Left-ventricular
- PICM:
-
Pacing-induced cardiomyopathy
- PPM:
-
Permanent pacemaker
- pQRSd:
-
Paced QRS duration
- pQTc:
-
Paced QTc interval
- ROC:
-
Receiver operating characteristic
- RV:
-
Right-ventricular
- TDI:
-
Tissue Doppler imaging
- TR:
-
Tricuspid regurgitant
References
Furman S, Schwedel JB. An intracardiac pacemaker for Stokes-Adams seizures. N Engl J Med. 1959;261(19):943–8.
Tse H-F, Lau C-P. Long-term effect of right ventricular pacing on myocardial perfusion and function. J Am Coll Cardiol. 1997;29(4):744–9.
Wilkoff BL, Cook JR, Epstein AE, Greene HL, Hallstrom AP, Hsia H, Kutalek SP, Sharma A, Dual C. Investigators VVIIDT: Dual-chamber pacing or ventricular backup pacing in patients with an implantable defibrillator: the dual chamber and VVI implantable defibrillator (DAVID) trial. JAMA. 2002;288(24):3115–23.
Sweeney MO, Hellkamp AS, Ellenbogen KA, Greenspon AJ, Freedman RA, Lee KL, Lamas GA, Investigators MOST. Adverse effect of ventricular pacing on heart failure and atrial fibrillation among patients with normal baseline QRS duration in a clinical trial of pacemaker therapy for sinus node dysfunction. Circulation. 2003;107(23):2932–7.
Curtis AB, Worley SJ, Adamson PB, Chung ES, Niazi I, Sherfesee L, Shinn T, Sutton MS. Biventricular versus Right Ventricular Pacing in Heart Failure Patients with Atrioventricular Block Trial I: Biventricular pacing for atrioventricular block and systolic dysfunction. N Engl J Med. 2013;368(17):1585–93.
Glikson M, Nielsen JC, Kronborg MB, Michowitz Y, Auricchio A, Barbash IM, Barrabes JA, Boriani G, Braunschweig F, Brignole M, et al. 2021 ESC Guidelines on cardiac pacing and cardiac resynchronization therapy. Eur Heart J. 2021;42:3427–520.
Funck RC, Mueller HH, Lunati M, Piorkowski C, De Roy L, Paul V, Wittenberg M, Wuensch D, Blanc JJ. Characteristics of a large sample of candidates for permanent ventricular pacing included in the Biventricular Pacing for Atrio-ventricular Block to Prevent Cardiac Desynchronization Study (BioPace). Europace. 2014;16(3):354–62.
Slotwiner DJ, Raitt MH, Del-Carpio Munoz F, Mulpuru SK, Nasser N, Peterson PN. Impact of physiologic pacing versus right ventricular pacing among patients with left ventricular ejection fraction greater than 35%: A systematic review for the 2018 ACC/AHA/HRS guideline on the evaluation and management of patients with bradycardia and cardiac conduction delay: a report of the American college of cardiology/American heart association task force on clinical practice guidelines and the heart rhythm society. J Am Coll Cardiol. 2019;74(7):988–1008.
Khurshid S, Epstein AE, Verdino RJ, Lin D, Goldberg LR, Marchlinski FE, Frankel DS. Incidence and predictors of right ventricular pacing-induced cardiomyopathy. Heart Rhythm. 2014;11(9):1619–25.
Nagueh SF, Smiseth OA, Appleton CP, Byrd BF 3rd, Dokainish H, Edvardsen T, Flachskampf FA, Gillebert TC, Klein AL, Lancellotti P, et al. Recommendations for the evaluation of left ventricular diastolic function by echocardiography: an update from the American society of echocardiography and the European association of cardiovascular imaging. J Am Soc Echocardiogr. 2016;29(4):277–314.
Nagueh SF, Appleton CP, Gillebert TC, Marino PN, Oh JK, Smiseth OA, Waggoner AD, Flachskampf FA, Pellikka PA, Evangelista A. Recommendations for the evaluation of left ventricular diastolic function by echocardiography. J Am Soc Echocardiogr. 2009;22(2):107–33.
Karpawich PP, Justice CD, Cavitt DL, Chang C-H. Developmental sequelae of fixed-rate ventricular pacing in the immature canine heart: An electrophysiologic, hemodynamic, and histopathologic evaluation. Am Heart J. 1990;119(5):1077–83.
Kim JH, Kang KW, Chin JY, Kim TS, Park JH, Choi YJ. Major determinant of the occurrence of pacing-induced cardiomyopathy in complete atrioventricular block: a multicentre, retrospective analysis over a 15-year period in South Korea. BMJ Open. 2018;8(2): e019048.
Kane GC, Karon BL, Mahoney DW, Redfield MM, Roger VL, Burnett JC Jr, Jacobsen SJ, Rodeheffer RJ. Progression of left ventricular diastolic dysfunction and risk of heart failure. JAMA. 2011;306(8):856–63.
Gibson DG, Francis DP. Clinical assessment of left ventricular diastolic function. Heart. 2003;89(2):231–8.
Khurshid S, Liang JJ, Owens A, Lin D, Schaller R, Epstein AE, Marchlinski FE, Frankel DS. Longer paced QRS duration is associated with increased prevalence of right ventricular pacing-induced cardiomyopathy. J Cardiovasc Electrophysiol. 2016;27(10):1174–9.
Chen S, Yin Y, Lan X, Liu Z, Ling Z, Su L, Kiuchi MG, Li X, Zhong B, Krucoff MW, et al. Paced QRS duration as a predictor for clinical heart failure events during right ventricular apical pacing in patients with idiopathic complete atrioventricular block: results from an observational cohort study (PREDICT-HF). Eur J Heart Fail. 2013;15(3):352–9.
Miyoshi F, Kobayashi Y, Itou H, Onuki T, Matsuyama T, Watanabe N, Liu C, Kawamura M, Asano T, Miyata A, et al. Prolonged paced QRS duration as a predictor for congestive heart failure in patients with right ventricular apical pacing. Pacing Clin Electrophysiol. 2005;28(11):1182–8.
Curtis AB, Worley SJ, Adamson PB, Chung ES, Niazi I, Sherfesee L, Shinn T, St John Sutton M. Biventricular pacing for atrioventricular block and systolic dysfunction. N Engl J Med. 2013;368:1585–93.
Strocchi M, Lee AWC, Neic A, Bouyssier J, Gillette K, Plank G, Elliott MK, Gould J, Behar JM, Sidhu B, et al. His-bundle and left bundle pacing with optimized atrioventricular delay achieve superior electrical synchrony over endocardial and epicardial pacing in left bundle branch block patients. Heart Rhythm. 2020;17(11):1922–9.
Kronborg MB, Mortensen PT, Poulsen SH, Gerdes JC, Jensen HK, Nielsen JC. His or para-His pacing preserves left ventricular function in atrioventricular block: a double-blind, randomized, crossover study. Europace. 2014;16(8):1189–96.
Vijayaraman P, Naperkowski A, Ellenbogen K, Dandamudi G. Permanent His bundle pacing in advanced AV block. Electrophysiological insights into site of AV block. JACC Clin Electrophysiol. 2015;1:571–81.
Lewis AJM, Foley P, Whinnett Z, Keene D, Chandrasekaran B. His bundle pacing: a new strategy for physiological ventricular activation. J Am Heart Assoc. 2019;8(6): e010972.
Vijayaraman P, Subzposh FA, Naperkowski A, Panikkath R, John K, Mascarenhas V, Bauch TD, Huang W. Prospective evaluation of feasibility and electrophysiologic and echocardiographic characteristics of left bundle branch area pacing. Heart Rhythm. 2019;16(12):1774–82.
Acknowledgements
None.
Funding
This study was supported by research funds from Korean Heart rhythm Society, 2022.
Author information
Authors and Affiliations
Contributions
Dr. HK Jeong, HY Kim and SS Kim has conceived, designed the study and collected the data. And all authors contributed to the analysis, interpretation of the data, and drafting of the manuscript. All authors have reviewed and approved the submission of the paper to the journal.
Corresponding author
Ethics declarations
Ethical Approval and Consent to participate.
The study protocol was authorized by the Institutional Review Board of each hospitals. This is a retrospective study and informed consent was waived.
Consent for publication
We agree.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Jeong, H.K., Kim, H.W., Kim, S.S. et al. Impact of diastolic dysfunction in patients with preserved ejection fraction undergoing permanent cardiac pacemaker placement. Int J Arrhythm 23, 26 (2022). https://doi.org/10.1186/s42444-022-00078-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s42444-022-00078-8