Abstract
Background
This systematic review and meta-analysis aimed to investigate the incidence and risk of knee and hip replacement in patients with osteoarthritis (OA) treated with different medications.
Methods
OVID MEDLINE, OVID EMBASE, Cochrane and Web of Science electronic databases were searched from inception to May 4th, 2022. Clinical trials, including randomized controlled trials, cohort studies and case–control studies, were selected. The meta-analysis effect size was estimated using either incidence with 95% confidence intervals (CIs) or odds ratio (OR)/relative risk (RR) with 95% CIs. The risk of bias and heterogeneity among studies were assessed and analyzed.
Results
Forty studies were included, involving 6,041,254 participants. The incidence of joint replacement in patients with OA varied according to the study design and treatments. The incidence of knee arthroplasty varied from 0 to 70.88%, while the incidence of hip arthroplasty varied from 11.71 to 96.43%. Compared to non-users, bisphosphonate users had a reduced risk of knee replacement (RR = 0.71, 95% CI: 0.66–0.77; adjusted hazard ratio [aHR] = 0.76, 95% CI: 0.70–0.83). Compared to intra-articular corticosteroid users, hyaluronic acid (HA) users had a higher risk of knee arthroplasty (RR = 1.76, 95% CI: 1.38–2.25). No publication bias was observed.
Conclusions
Bisphosphonate treatment is associated with a reduced risk of knee replacement. More studies are needed to validate our results due to the limited number of eligible studies and high heterogeneity among studies.
Similar content being viewed by others
Background
Osteoarthritis (OA) is a degenerative disease involving the cartilage and surrounding tissues, usually manifesting common clinical signs such as pain, stiffness, and swelling, which may lead to functional disability. The most commonly involved joints are those of the knee, hip, hand, facet, and foot. The age-standardized global prevalence of knee OA is 3.8%, while that of hip OA is 0.85% [1]. Approximately 10% of men and 13% of women aged over 60 years are diagnosed with symptomatic knee OA [2]. OA occurs more commonly in women than in men, with a female-to-male ratio ranging from 1.5 to 4. Since its prevalence increases with age, it is highly prevalent in the population aged over 50 years [3]. Obesity, age, female sex, and genotype are risk factors for the development of hip and knee OA [2, 4, 5].
Knee and hip OA are ranked as the top 11th contributor to global disability and the top 38th contributor to disability-adjusted life years (DALYs), which significantly affects patients’ psychological state [3] and places a substantial economic burden on the family and society [1]. Pharmacological treatment for OA includes acetaminophen, nonsteroidal anti-inflammatory drugs (NSAIDs), cyclooxygenase-2 (COX-2) inhibitors, intra-articular steroid injections, viscosupplementation, chondroitin, glucosamine, and bisphosphonates [5,6,7]. Acetaminophen and NSAIDs are major choices for OA to relieve pain, while COX-2 inhibitors are used if NSAIDs are contraindicated. Intra-articular steroid injections are effective in reducing pain and improving function through anti-inflammatory and antinociceptive actions. Intra-articular injection of hyaluronic acid (HA) or its derivatives, is a form of viscosupplementation that is used to alleviate symptoms and improve function. Chondroitin and glucosamine are disease-modifying agents in OA [8, 9]. Bisphosphonates effectively reduce pain and slow structural progression in patients with OA [10, 11].
Globally, symptomatic OA most commonly develops in large weight-bearing joints such as the knee and hip. Arthroplasty is an effective way to improve pain, disability, physical activity, and quality of life when conservative measures fail to control pain and improve joint function [6, 12, 13]. Patients with OA has a higher risk for arthroplasty. Among females patients, the incidence of hip replacement is 52.7%, while the incidence of knee replacement is 17.9%. Among male patients, the incidence of hip replacement is 37.7%, while the incidence of knee replacement is 11.8%. In general population, the incidence of hip replacement and knee replacement is 2.34% and 4.55%, respectively [14, 15]. However, it is unclear whether the increased arthroplasty rate in patients with OA is related to drug treatment. Accumulating evidence is available on the incidence and risk of arthroplasty in patients with OA who are on different pharmacological treatments. Hence, this systematic review and meta-analysis was performed to evaluate the incidence and risk of knee or hip joint replacement in patients with OA treated with NSAIDs, HA, glucosamine, chondroitin, bisphosphonate, or corticosteroids.
Materials and methods
We conducted a systematic review and meta-analysis to investigate the incidence and risk of knee or hip joint replacement in patients with OA treated pharmacologically, while adhering to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines [16]. The predefined study protocol can be solicited from the supplementary attach (Additional file 2).
Eligibility criteria
We included studies that met the following criteria: (1) the study population included patients with OA of the knee or hip; (2) treatment intervention including HA, NSAIDs, glucosamine, chondroitin, bisphosphonates, and corticosteroids; (3) comparator treatment including placebo, no comparator treatment, or any treatment; (4) outcomes including arthroplasty of the knee or hip, such as total knee arthroplasty, total hip arthroplasty, unicompartmental knee arthroplasty, and patellofemoral joint arthroplasty; (5) study design including a randomized controlled trial (RCT), cohort study, or case–control study.
Duplicate studies, letters, correspondences, and study protocols were excluded. Studies that were not reported in English or Chinese were excluded during selection.
Search strategy
To perform systematic retrieval, the electronic databases OVID MEDLINE, OVID EMBASE, Cochrane and Web of Science were searched from inception to May 4th, 2022 by using a Medical Subject Headings term and a keyword. The search terms were “osteoarthritis,” “hyaluronic acid,” “NSAIDs,” “glucosamine,” “chondroitin,” “bisphosphonate,” “corticosteroid,” “arthroplasty,” “RCT,” “cohort study,” and “case–control study.” The detailed search strategy is provided in the Additional file 1. The reference lists of the included studies were manually checked to identify potentially eligible studies.
Study selection
Studies were selected using a two-step screening process. First, the studies were screened using titles and abstracts, following which they were screened by full-text review. The references retrieved from the electronic databases were introduced to Endnote (USA). After removing duplicates, the studies were exported to Microsoft Office Access 2013 (USA) for preliminary screening by titles and abstracts based on our study selection criteria. The full texts of the remaining studies from the first screening were downloaded for further screening based on the study eligibility criteria. Reference lists of the included studies were manually checked. Two authors independently screened the studies, and any disagreement was resolved via discussion or adjudication by a third reviewer, if necessary.
Data extraction
Two authors independently collected data on the first author’s family name, country, study design, OA site, follow-up time, number of arthroplasty cases, number of participants, and treatments. If a study reported results at different time points, data from the longest follow-up period were used. Any disagreement on data extraction was resolved via discussion or adjudication by a third reviewer, if necessary.
Methodological quality assessment
The risk of bias of RCTs was assessed using the Jadad scale, which focuses on randomization, double blinding, drop out, and loss of follow-up [17]. For randomization and double blinding, reporting with an appropriate method scored as 2, reporting without an appropriate method scored as 1, and no reporting was scored as 0. For drop-out and loss of follow-up, detailed reporting was scored as 1, while no reporting was scored as 0. Therefore, the highest score was 5, and a score of ≥ 3 was considered as being at a low risk of bias.
The methodological quality assessment of cohort studies and case–control studies was conducted using the Newcastle–Ottawa quality assessment scale (NOS) [18]. A total of three domains—selection, comparability, and exposure—with eight numbered items yielded the highest total score of 9. For selection and exposure, each of seven numbered items was scored as 1 if the answer was yes, while for comparability, a maximum score of 2 was given for a numbered item. Studies with a score ≥ 6 were considered high-quality studies.
Two authors performed the methodological quality assessment, and any disagreement was resolved via discussion or adjudication by a third reviewer, if necessary.
Data analysis
We performed data analyses using RevMan software (version 5.1.3, the Nordic Cochrane Centre, The Cochrane Collaboration, Copenhagen), and a random effect model was applied regardless of heterogeneity. The incidence of athroplasty in each study was listed. We used the random effect inverse variance model to pool the risks of arthroplasty in different treatments. Adjusted estimates namely adjusted hazard ratio (aHR) and adjusted OR (aOR), and their 95% CIs reported from cohort and case–control studies were pooled using the random effect inverse variance model. We first log-transformed the point estimate and 95% CIs and pooled the log-estimate and its associated standard error in such analyses. Data from more than 2 studies were summarized.
According to the Cochrane Handbook recommendations, we assessed clinical diversity across studies through statistical heterogeneity using I2 and p values. I2 values of 25%, 50%, and 75% represented low, moderate, and high heterogeneity, respectively [19]. For each of the above analyses, we conducted stratified subgroup analyses according to the arthroplasty site and treatment. Sensitivity analysis was performed by excluding studies one by one to identify the potential source of heterogeneity. We assessed the risk of publication bias using funnel plots and used Egger’s test to quantify the p value when the funnel plot was visually asymmetrical by Stata (version 16.0, USA).
Results
Study selection
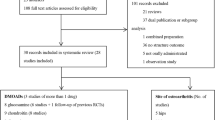
A total of 4642 studies were retrieved from the electronic databases of OVID MEDLINE (n = 598), OVID EMBASE (n = 2141), Cochrane (n = 1528) and Web of Science (n = 375). After excluding 1797 duplicates, 2845 studies underwent the first screening by titles and abstracts. After excluding 2,703 irrelevant studies, 142 reviews underwent full-text review. Finally, 40 studies were included [20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59]. (Fig. 1).
Characteristics of the included studies
Of the 40 eligible studies, eight were RCTs [33, 40, 42, 46, 50, 57,58,59] comprising 231 arthroplasty cases and 4790 participants; 27 were cohort studies [20,21,22,23,24,25,26,27,28, 31, 32, 34,35,36,37,38,39, 43, 44, 48, 49, 52,53,54,55,56] including over 597,451 arthroplasty cases and over 5,959,704 participants; and 5 were case–control studies [29, 41, 45, 47, 51] including 27,045 arthroplasty cases and 76,760 participants. Fourteen studies were from the USA, five were from Canada, four were from France, and four were from the Netherlands. The remaining studies were reported from other countries, such as Finland, Belgium, China, Italy, Japan, Norway, Romania, Thailand, and the UK. While 22 studies reported on knee OA, 11 studies reported on hip OA, and 7 studies reported on knee and hip OA. The follow-up time ranged from 0.3 years in an RCT to 9 years in a cohort study. The number of arthroplasty cases varied from 0 in an RCT to 6706 in a cohort study. The number of participants ranged from 12 in an RCT to 123,791 in a cohort study (Additional file 1: Tables S1–S3).
Methodological quality
Four RCTs had a Jadad score of ≥ 3, indicating a low risk of bias, while the remaining 4 RCTs had a Jadad score of < 3, showing a high risk of bias. Of the 27 cohort studies, 25 studies had a NOS score of ≥ 6, indicating high study quality, while 2 studies were rated as being of low quality (NOS score < 6). All five case–control studies were considered high-quality studies (Additional file 1: Tables S1–S3).
Demographic data
Among the 40 included studies, only 5 studies were conducted in Asian. In Asian patients with knee/hip osteoarthritis, the incidence of knee arthroplasty varied from 0 to 22.3%. Only one RCT demonstrated the incidence of hip arthroplasty, which was 23.33%. Among European knee/hip osteoarthritis population, the incidence of knee arthroplasty varied from 0 to 70.88%, while the incidence of hip arthroplasty varied from 4.61 to 96.43%. In most studies, female patients were dominant, with the proportion of female patients ranging from 49.1 to 91.9%.
Incidence of arthroplasty
Since the heterogeneity of the meta-analysis of the incidence of arthroplasty was high and could not be reduced by subgroup analysis, we enumerated the incidence rate reported in each study rather than combine them.
Intra-articular corticosteroids
Five studies, including 5 cohort studies and 1 case–control studies, were involved to present the incidence of knee/hip arthroplasty in patients with intra-articular corticosteroids treatment. Since the subjects of Villoutreix’s study were patients with rapidly destructive hip osteoarthritis, the incidence of hip athroplasty was 96.43% [54]. In other studies, the incidence of knee athroplasty varied from 6.9 to 37.1%, while the incidence of hip athroplasty was from 43.96 to 72.22%. (shown in Table 1 and Additional file 1: Table S1).
Hyaluronic acid
The incidence of knee/hip arthroplasty in patients with intra-articular hyalurionic acid treatment was demonstrated in 15 studies (14 cohort studies and 1 RCT). The incidence of knee athroplasty varied from 4.96 to 39.21%, while the incidence of hip athroplasty was from 18.18 to 49.17%. In Gaston’s cohort study, the invention treatment was synthetic hyaluronic acid (Suplasyn™) [53]. Sodium Hyaluronate was used in Turajane’s and Migliore’s studies, but the molecular weight of sodium hyaluronate was different (500–730 kDa in Turajane’s study and 1500–2000 kDa in Migliore’s study) [43, 48]. In three cohort studies, Hylan G-F 20 was used [22, 37, 44]. (Shown in Table 1 and Additional file 1: Table S1).
Bisphosphonates
The incidence of knee/hip arthroplasty in patients with bisphosphonates treatment was demonstrated in 4 studies (2 cohort studies and 2 RCT). The incidence of knee athroplasty varied from 3.66 to 15.00%, while the incidence of hip athroplasty was 23.33%. In Turajane’s and Nishii’s RCT study, patients in intervention group was treated with Alendronate combined with calcium [33, 42]. In Fu’s study, Alendronate, Ibandronate and Zoledronate users were enrolled [35]. The types of bisphosphonates were not mentioned in Neogi study [27]. (Shown in Table 1 and Additional file 1: Table S1).
Symptomatic slow acting drugs for osteoarthritis (SYSADOA)
The incidence of knee/hip arthroplasty in patients with SYSADOA treatment was demonstrated in 4 studies (1 cohort study, 1 case–control study and 2 RCTs). The incidence of knee athroplasty varied from 0 to 31.10%. Only one study demonstrated the incidence of hip arthroplasty, which was 11.71%. Among the 4 studies, patients in Bruyere’s and Rozendaal’s studies were treated glucosamine sulfate (1500 mg daily), while chondroitin sulphate (Condrosan, 800 mg/day) was used in Wildi’s study [46, 50, 52]. In Dorais’ study, patients were treated glucosamine or chondroitin sulfate [29]. (Shown in Table 1 and Additional file 1: Table S1).
NSAIDs
The incidence of knee/hip arthroplasty in patients with NSAIDs treatment was demonstrated in 12 studies (3 cohort studies, 5 case–control studies and 4 RCTs). The incidence of knee athroplasty varied from 1.49 to 70.88%. The incidence of hip athroplasty varied from 4.61 to 69.29%. The incidence of hip/knee athroplasty varied from 0.47 to 67.53%. Coxibs were the intervention drug in one study, and the incidence of knee athroplasty in this study was 10.94% [45]. Licofelone was the intervention drug in another study, and the incidence of knee and hip athroplasty in this study was 70.88% and 69.29% respectively [47]. Naproxen was the intervention drug in 3 studies [47, 57, 58]. The types of NSAIDs were not available in other 7 studies. (Shown in Table 1 and Additional file 1: Table S1).
Risk of arthroplasty
Evidence from RCTs
Compared to tanezumab, NSAIDs (OR = 1.21, 95% CI: 0.74–1.97, I2 = 0), or naproxen (OR = 2.00, 95% CI: 0.21–19.3, I2 = 0, 1/417 vs. 1/834, n = 2) did not increase the overall risk of arthroplasty, regardless of OA site. The number of arthroplasties and the total number of participants were 26 and 956, respectively, in the NSAID group and 44 and 1,917, respectively, in the tanezumab group. Compared to the placebo, NSAIDs (OR = 1.07, 95% CI: 0.29–3.96, I2 = 41, 83/1495 vs. 47/1500, n = 3) and naproxen (OR = 0.35, 95% CI: 0.05–2.30, I2 = 0, 1/417 vs. 4/417, n = 2) did not elevate the risk of knee or hip arthroplasty in patients with OA (Table 2, Additional file 1: Fig. S5, Additional file 1: Fig. S7).
Evidence from cohort studies
Compared to non-users, bisphosphonate users had a 29% decreased risk of knee arthroplasty (RR = 0.71, 95% CI: 0.66–0.77, I2 = 0, 733/18,282 vs. 6876/125,797, n = 2). Compared to non-users, HA was not associated with the risk of arthroplasty (RR = 2.27, 95% CI: 0.86–5.94, n = 5). Compared to intra-articular corticosteroid users, hyaluronic acid (HA) users had a higher risk of knee arthroplasty (RR = 1.76, 95% CI: 1.38–2.25). Nevertheless, glucocorticoid users did not have a decreased risk of arthroplasty (RR = 1.96, 95% CI: 0.57–6.75, n = 2) compared to non-users. (Table 2, Figs. 2, 3, 4, 5).
Evidence from case–control studies
With respect to knee/hip OA, compared to non-users, NSAID users did not evaluate the risk of arthroplasty (OR = 1.68, 95% CI: 0.69–4.08, I2 = 97, n = 4). (Table 2, Additional file 1: Fig. S4) Naproxen users did not reduce the risk of hip/knee arthroplasty (OR = 0.08, 95% CI: 0.17–3.65, I2 = 87, n = 2). With respect to knee OA, compared to non-users, NSAID users had an increased risk of arthroplasty (OR = 2.96, 95% CI: 1.13–7.79, I2 = 96, 807/1272 vs. 9155/27170, n = 2) (Table 2).
Publication bias
Funnel plots were asymmetrical in the analysis of the association of NSAIDs treatment in case–control studies as well as HA treatment in cohort studies, and the values of Egger’s test > 0.05, respectively. Other funnel plots of the association between the incidence of knee/hip arthroplasty and pharmacological treatments were symmetrical. Therefore, publication bias was considered unlikely (Additional file 1: Figs. S1–S3).
Heterogeneity source
Heterogeneity was observed in meta-analysis of cohort studies. Excluding studies one by one did not reveal any apparent possible heterogeneity.
Discussion
This systematic review and meta-analysis scrutinized all available evidence to investigate the incidence and risk of knee or hip arthroplasty in patients with OA treated with NSAIDs, HA, SYSADO, bisphosphonates, or corticosteroids. The incidence of arthroplasty varied across study design and treatment, with the highest incidence of knee replacement of 70.88% reported by a case–control study in coxib-treated patients with OA, and the lowest incidence of knee arthroplasty of 0%, reported by a RCT in Condrosan-treated patients. Compared to non-users, bisphosphonate users had a reduced risk of knee replacement (RR = 0.71, 95% CI: 0.66–0.77; aHR = 0.76, 95% CI: 0.70–0.83). Compared to intra-articular corticosteroid users, hyaluronic acid (HA) users had a lower risk of knee arthroplasty (RR = 1.76, 95% CI: 1.38–2.25). NSAID use was associated with an increased risk of knee replacement (OR = 2.96, 95% CI: 1.13–7.79).
We found that bisphosphonate users had a reduced risk of knee replacement compared to non-users. Bisphosphonates, commonly indicated as osteoporosis treatment, inhibit the activity of osteoclasts by inhibiting the development of osteoclast progenitors and suppressing local bone turnover after attaching to hydroxyapatite binding sites on bony surfaces, particularly those undergoing active bone resorption, thus repressing bone resorption [60, 61]. In OA, subchondral bone metabolism is defective, and increased subchondral bone turnover may lead to pain, which could be alleviated by targeting osteoclasts. However, the use of bisphosphonates in reducing knee arthroplasty is controversial [62]. Li et al. stated that Neogi et al. ignored the sociocultural factor in their study, which might affect the choice and accessibility of arthroplasty for patients with OA. Further investigations are needed to clarify the beneficial role of bisphosphonates in reducing arthroplasty due to the limited number of eligible studies in this meta-analysis.
Our study demonstrated that compared to the non-users, NSAID users have a higher risk of knee arthoplasty. This may be because NSAIDs users had a lower perception in joint pain and disease activity, resulting in poor joint protection from hazardous positions, activities and weight bearings. In addition, patients who are willing to use NSAIDs may be more inclined to receive joint replacement therapy [37].
Our study demonstrated that HA could not reduce the risk of knee/hip arthroplasty. And compared with intra-articular CS therapy, HA treatment elevated the risk of joint replacement. Some studies reported HA could delay the time of arthroplasty [36, 42]. According to a previous study, HA combined with intra-articular CS could reduce joint pain earlier than HA alone. Though clinical parameters improved after combined therapy, the cartilage damage remained [63].
We included three study designs in our systematic review and meta-analysis. While the incidence of arthroplasty was low in RCTs, it was high in case–control studies despite the use of the same drug. RCTs provided imprecise estimates due to the very low event rate and short follow-up duration, while cohort and case–control studies provided accurate information on the incidence and potential risk of arthroplasty given their ability to capture large patient data and outcomes over a long duration [64]. A retrospective cohort study can detect more adverse events than other study designs, such as a cross-sectional design [65].
This study has several limitations. High heterogeneity existed among the cohort and case-control studies. Subgroup analysis according to treatment and OA site did not significantly reduce heterogeneity, which could be explained by the diverse study populations and treatments. As participants from all over the world were represented in the study, there were economic, racial and cultural disparities, which greatly influenced the patients’ choice for arthroplasty [61]. The differences in the female-to-male ratios and disease severity of the studied patients with OA might have also contributed to the high heterogeneity [66]. Therefore, additional investigations such as subgroup analysis by follow-up time, sex ratio, and disease severity could not be performed.
Conclusion
In conclusion, the incidence of knee and hip arthroplasty was found to vary across different treatments and study designs. Compared with no treatment, treatment with bisphosphonates reduced the risk of knee replacement, while NSAIDs and HA users had an increased risk of knee replacement. However, more studies are needed to validate our results due to the limited number of eligible studies and high heterogeneity among studies.
Availability of data and materials
All data are available in the manuscript and Additional materials.
Abbreviations
- OA:
-
Osteoarthritis
- DALYs:
-
Disability-adjusted life years
- NSAIDs:
-
Nonsteroidal anti-inflammatory drugs
- SYSADOA:
-
Symptomatic slow acting drugs for osteoarthritis
- HA:
-
Hyaluronic acid
References
Cross M, Smith E, Hoy D, Nolte S, Ackerman I, Fransen M, et al. The global burden of hip and knee osteoarthritis: estimates from the global burden of disease 2010 study. Ann Rheum Dis. 2014;73(7):1323–30. https://doi.org/10.1136/annrheumdis-2013-204763.
Zhang Y, Jordan JM. Epidemiology of osteoarthritis. Clin Geriatr Med. 2010;26(3):355–69. https://doi.org/10.1016/j.cger.2010.03.001.
Litwic A, Edwards MH, Dennison EM, Cooper C. Epidemiology and burden of osteoarthritis. Br Med Bull. 2013;105:185–99. https://doi.org/10.1093/bmb/lds038.
Prieto-Alhambra D, Judge A, Javaid MK, Cooper C, Diez-Perez A, Arden NK. Incidence and risk factors for clinically diagnosed knee, hip and hand osteoarthritis: influences of age, gender and osteoarthritis affecting other joints. Ann Rheum Dis. 2014;73(9):1659–64. https://doi.org/10.1136/annrheumdis-2013-203355.
Taruc-Uy RL, Lynch SA. Diagnosis and treatment of osteoarthritis. Prim Care. 2013;40(4):821–36, vii. https://doi.org/10.1016/j.pop.2013.08.003.
Chinese Orthopaedic Association. Diagnosis and treatment of osteoarthritis. Orthop Surg. 2010;2(1):1–6. https://doi.org/10.1111/j.1757-7861.2009.00055.x.
Yu SP, Hunter DJ. Managing osteoarthritis. Aust Prescr. 2015;38(4):115–9. https://doi.org/10.18773/austprescr.2015.039.
Reginster JY, Deroisy R, Rovati LC, Lee RL, Lejeune E, Bruyere O, et al. Long-term effects of glucosamine sulphate on osteoarthritis progression: a randomised, placebo-controlled clinical trial. Lancet. 2001;357(9252):251–6. https://doi.org/10.1016/S0140-6736(00)03610-2.
Kahan A, Uebelhart D, De Vathaire F, Delmas PD, Reginster JY. Long-term effects of chondroitins 4 and 6 sulfate on knee osteoarthritis: the study on osteoarthritis progression prevention, a 2-year, randomized, double-blind, placebo-controlled trial. Arthritis Rheum. 2009;60(2):524–33. https://doi.org/10.1002/art.24255.
Laslett LL, Kingsbury SR, Hensor EM, Bowes MA, Conaghan PG. Effect of bisphosphonate use in patients with symptomatic and radiographic knee osteoarthritis: data from the Osteoarthritis Initiative. Ann Rheum Dis. 2014;73(5):824–30. https://doi.org/10.1136/annrheumdis-2012-202989.
Iwamoto J, Takeda T, Sato Y, Matsumoto H. Effects of risedronate on osteoarthritis of the knee. Yonsei Med J. 2010;51(2):164–70. https://doi.org/10.3349/ymj.2010.51.2.164.
Ones CA, Voaklander DC, Johnston DW, Suarez-Almazor ME. Health related quality of life outcomes after total hip and knee arthroplasties in a community based population. J Rheumatol. 2000;27(7):1745–52.
Hunter DJ, Bierma-Zeinstra S. Osteoarthritis. Lancet. 2019;393(10182):1745–59. https://doi.org/10.1016/S0140-6736(19)30417-9.
Quintana JM, Arostegui I, Escobar A, Azkarate J, Goenaga JI, Lafuente I. Prevalence of knee and hip osteoarthritis and the appropriateness of joint replacement in an older population. Arch Intern Med. 2008;168(14):1576–84. https://doi.org/10.1001/archinte.168.14.1576.
Maradit Kremers H, Larson DR, Crowson CS, Kremers WK, Washington RE, Steiner CA. Prevalence of Total Hip and Knee Replacement in the United States. J Bone Jt Surg Am. 2015;97(17):1386–97. https://doi.org/10.2106/JBJS.N.01141.
Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535. https://doi.org/10.1136/bmj.b2535.
Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996;17(1):1–12. https://doi.org/10.1016/0197-2456(95)00134-4.
Wells GA, Shea B, O'Connell J. The Newcastle–Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. 2012.
Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–60. https://doi.org/10.1136/bmj.327.7414.557.
Ward MM. Osteoarthritis care and risk of total knee arthroplasty among medicare beneficiaries: a population-based study of regional covariation. Arthritis Rheumatol. 2021;73(12):1–28. https://doi.org/10.1002/art.41878.
Ong KL, Runa M, Lau E, Altman RD. Cost-of-illness of knee osteoarthritis: potential cost savings by not undergoing arthroplasty within the first 2 years. Clinicoecon Outcomes Res. 2019;11:245–55. https://doi.org/10.2147/CEOR.S170119.
Concoff A, Niazi F, Farrokhyar F, Alyass A, Rosen J, Nicholls M. Delay to TKA and costs associated with knee osteoarthritis care using intra-articular hyaluronic acid: analysis of an administrative database. Clin Med Insights Arthritis Musculoskelet Disord. 2021;14:1–8. https://doi.org/10.1177/1179544121994092.
Zeng C, Lane NE, Hunter DJ, Wei J, Choi HK, McAlindon TE, et al. Intra-articular corticosteroids and the risk of knee osteoarthritis progression: results from the Osteoarthritis Initiative. Osteoarthr Cartil. 2019;27(6):855–62. https://doi.org/10.1016/j.joca.2019.01.007.
Walter WR, Bearison C, Slover JD, Gold HT, Gyftopoulos S. Clinical and patient-reported outcomes after image-guided intra-articular therapeutic hip injections for osteoarthritis-related hip pain: a retrospective study. Skeletal Radiol. 2019;48(5):713–9. https://doi.org/10.1007/s00256-018-3113-3.
Latourte A, Rat AC, Sime WN, Omorou A, Eymard F, Sellam J, et al. Do corticosteroids or hyaluronic acid intra-articular injections impact the risk of total knee replacement? Real-life data from the Khoala cohort. Osteoarthr Cartil. 2019;27:S509–10. https://doi.org/10.1007/10.1016/j.joca.2019.02.577.
Schwappach J, Schultz J, Salottolo K, Bar-Or D. Incidence of total knee replacement subsequent to intra-articular injection of the anti-inflammatory compound LMWF-5A versus saline: a long-term follow-up study to a randomized controlled trial. Patient Saf Surg. 2018;12:14. https://doi.org/10.1186/s13037-018-0162-4.
Neogi T, Li S, Peloquin C, Misra D, Zhang Y. Effect of bisphosphonates on knee replacement surgery. Ann Rheum Dis. 2018;77(1):92–7. https://doi.org/10.1136/annrheumdis-2017-211811.
Hung CC, Wang CY, Fu SH, Yang RS, Hsiao FY. Effects of anti-osteoporosis medications on total hip arthroplasty risks in osteoporotic patients with hip osteoarthritis in Taiwan: a nationwide cohort study. Arch Osteoporos. 2018;13(1):107. https://doi.org/10.1007/s11657-018-0522-9.
Dorais M, Martel-Pelletier J, Raynauld JP, Delorme P, Pelletier JP. Impact of oral osteoarthritis therapy usage among other risk factors on knee replacement: a nested case-control study using the Osteoarthritis Initiative cohort. Arthritis Res Ther. 2018;20(1):172. https://doi.org/10.1186/s13075-018-1656-2.
Dasa V, Lim S, Heeckt P. Real-world evidence for safety and effectiveness of repeated courses of hyaluronic acid injections on the time to knee replacement surgery. Am J Orthop (Belle Mead NJ). 2018;47(7):058. https://doi.org/10.12788/ajo.2018.0058.
Bowman EN, Hallock JD, Throckmorton TW, Azar FM. Hyaluronic acid injections for osteoarthritis of the knee: predictors of successful treatment. Int Orthop. 2018;42(4):733–40. https://doi.org/10.1007/s00264-017-3731-8.
Annaniemi JA, Pere J, Giordano S. Platelet-rich plasma versus hyaluronic acid injections for knee osteoarthritis: a propensity-score analysis. Scand J Surg. 2019;108(4):329–37. https://doi.org/10.1177/1457496918812218.
Turajane T, Chaveewanakorn U, Fongsarun W, Aojanepong J, Papadopoulos KI. Avoidance of total knee arthroplasty in early osteoarthritis of the knee with intra-articular implantation of autologous activated peripheral blood stem cells versus hyaluronic acid: a randomized controlled trial with differential effects of growth factor addition. Stem Cells Int. 2017;2017:1–10. https://doi.org/10.1155/2017/8925132.
Shewale AR, Barnes CL, Fischbach LA, Ounpraseuth ST, Painter JT, Martin BC. Comparative effectiveness of intra-articular hyaluronic acid and corticosteroid injections on the time to surgical knee procedures. J Arthroplasty. 2017;32(12):3591-3597.e24. https://doi.org/10.1016/j.arth.2017.07.007.
Fu SH, Wang CY, Yang RS, Wu FL, Hsiao FY. Bisphosphonate use and the risk of undergoing total knee arthroplasty in osteoporotic patients with osteoarthritis. J Bone Jt Surg. 2017;99(11):938–46. https://doi.org/10.2106/JBJS.16.00385.
Delbarre A, Amor B, Bardoulat I, Tetafort A, Pelletier-Fleury N. Do intra-articular hyaluronic acid injections delay total knee replacement in patients with osteoarthritis—a Cox model analysis. PLoS ONE. 2017;12(11):e0187227. https://doi.org/10.1371/journal.pone.0187227.
Boutefnouchet T, Puranik G, Holmes E, Bell KM. Hylan GF-20 viscosupplementation in the treatment of symptomatic osteoarthritis of the knee: clinical effect survivorship at 5 years. Knee Surg Relat Res. 2017;29(2):129–36. https://doi.org/10.5792/ksrr.16.061.
Hafezi-Nejad N, Guermazi A, Roemer FW, Eng J, Zikria B, Demehri S. Long term use of analgesics and risk of osteoarthritis progressions and knee replacement: propensity score matched cohort analysis of data from the Osteoarthritis Initiative. Osteoarthr Cartil. 2016;24(4):597–604. https://doi.org/10.1016/j.joca.2015.11.003.
Demehri S, Nejad NH, Roemer F, Guermazi A, Demehri S. Chondroitin sulfate and glucosamine supplementation is associated with higher incidence of radiographic knee osteoarthritis and subsequent knee replacement: 9 years of follow-up data from the osteoarthritis initiative. Osteoarthr Cartil. 2016;24:S307. https://doi.org/10.1016/j.joca.2016.01.554.
Schnitzer TJ, Ekman EF, Spierings EL, Greenberg HS, Smith MD, Brown MT. Efficacy and safety of tanezumab monotherapy or combined with non-steroidal anti-inflammatory drugs in the treatment of knee or hip osteoarthritis pain. Ann Rheum Dis. 2015;74(6):1202–11. https://doi.org/10.1136/annrheumdis-2013-204905.
Arends RHGP, Karsdal MA, Verburg KM, West CR, Bay-Jensen AC, Keller DS. Identification of serological biomarker profiles associated with total joint replacement in osteoarthritis patients. Osteoarthr Cartil. 2017;25(6):866–77. https://doi.org/10.1016/j.joca.2017.01.006.
Nishii T, Tamura S, Shiomi T, Yoshikawa H, Sugano N. Alendronate treatment for hip osteoarthritis: prospective randomized 2-year trial. Clin Rheumatol. 2013;32(12):1759–66.
Migliore A, et al. The impact of treatment with hylan G-F 20 on progression to total hip arthroplasty in patients with symptomatic hip OA: a retrospective study. Curr Med Res Opin. 2012;28(5):755–60. https://doi.org/10.1007/s10067-013-2338-8.
Migliore A, Bella A, Bisignani M, Calderaro M, De Amicis D, Logroscino G, et al. Total hip replacement rate in a cohort of patients affected by symptomatic hip osteoarthritis following intra-articular sodium hyaluronate (MW 1500–2000 kDa) ORTOBRIX study. Clin Rheumatol. 2012;31(8):1187–96. https://doi.org/10.1007/s10067-012-1994-4.
Klop C, de Vries F, Lalmohamed A, Mastbergen SC, Leufkens HG, Noort-van der Laan WH, et al. COX-2-selective NSAIDs and risk of hip or knee replacements: a population-based case-control study. Calcif Tissue Int. 2012;91(6):387–94. https://doi.org/10.1007/s00223-012-9646-x.
Wildi LM, Raynauld JP, Martel-Pelletier J, Beaulieu A, Bessette L, Morin F, et al. Chondroitin sulphate reduces both cartilage volume loss and bone marrow lesions in knee osteoarthritis patients starting as early as 6 months after initiation of therapy: a randomised, double-blind, placebo-controlled pilot study using MRI. Ann Rheum Dis. 2011;70(6):982–9. https://doi.org/10.1136/ard.2010.140848.
Raynauld JP, Martel-Pelletier J, Haraoui B, Choquette D, Dorais M, Wildi LM, et al. Risk factors predictive of joint replacement in a 2-year multicentre clinical trial in knee osteoarthritis using MRI: results from over 6 years of observation. Ann Rheum Dis. 2011;70(8):1382–8. https://doi.org/10.1136/ard.2010.146407.
Turajane T, Amphansap T, Labpiboonpong V, Maungsiri S. Total knee replacement following repeated cycles of intra-articular sodium hyaluronate (500–730 Kda) in failed conservative treatment of knee osteoarthritis: a 54-month follow-up. J Med Assoc Thai. 2009;92(6):S63–8.
van den Bekerom MP, Rys B, Mulier M. Viscosupplementation in the hip: evaluation of hyaluronic acid formulations. Arch Orthop Trauma Surg. 2008;128(3):275–80. https://doi.org/10.1007/s00402-007-0374-z.
Rozendaal RM, Koes BW, van Osch GJ, Uitterlinden EJ, Garling EH, Willemsen SP, et al. Effect of glucosamine sulfate on hip osteoarthritis: a randomized trial. Ann Intern Med. 2008;148(4):268–77. https://doi.org/10.7326/0003-4819-148-4-200802190-00005.
Pope JE, Mccrea K, Stevens A, Ouimet JM. The relationship between NSAID use and osteoarthritis (OA) severity in patients with hip and knee OA: results of a case control study of NSAID use comparing those requiring hip and knee replacements to those in whom surgery was not recommended. Med Sci Monit. 2008;14(12):Cr604–10. https://doi.org/10.1016/j.mehy.2008.07.011.
Pavelka K, Giacovelli G, Bruyere O, Olejarova M, Reginster JY, Deroisy R, et al. Total joint replacement after glucosamine sulphate treatment in knee osteoarthritis: results of a mean 8-year observation of patients from two previous 3-year, randomised, placebo-controlled trials. Osteoarthr Cartil. 2008;16(2):254–60. https://doi.org/10.1016/j.joca.2007.06.011.
Gaston MS, Tiemessen CH, Philips JE. Intra-articular hip viscosupplementation with synthetic hyaluronic acid for osteoarthritis: efficacy, safety and relation to pre-injection radiographs. Arch Orthop Trauma Surg. 2007;127(10):899–903. https://doi.org/10.1007/s00402-007-0363-2.
Villoutreix C, Pham T, Tubach F, Dougados M, Ayral X. Intraarticular glucocorticoid injections in rapidly destructive hip osteoarthritis. Jt Bone Spine. 2006;73(1):66–71. https://doi.org/10.1016/j.jbspin.2005.06.002.
Reijman M, Bierma-Zeinstra SM, Pols HA, Koes BW, Stricker BH, Hazes JM. Is there an association between the use of different types of nonsteroidal antiinflammatory drugs and radiologic progression of osteoarthritis? The Rotterdam Study. Arthritis Rheum. 2005;52(10):3137–42. https://doi.org/10.1002/art.21357.
Gossec L, Tubach F, Baron G, Ravaud P, Logeart I, Dougados M. Predictive factors of total hip replacement due to primary osteoarthritis: a prospective 2 year study of 505 patients. Ann Rheum Dis. 2005;64(7):1028–32. https://doi.org/10.1136/ard.2004.029546.
Alho A, Jaer O, Slungaard U, Holme I. Piroxicam and naproxen in patients with osteoarthritis of the hip waiting for total hip replacement. Clin Rheumatol. 1988;7(2):208–13. https://doi.org/10.1007/BF02204456.
Ekman EF, Gimbel JS, Bello AE, Smith MD, Keller DS, Annis KM, et al. Efficacy and safety of intravenous tanezumab for the symptomatic treatment of osteoarthritis: 2 randomized controlled trials versus naproxen. J Rheumatol. 2014;41(11):2249–59. https://doi.org/10.3899/jrheum.131294.
Balanescu AR, Feist E, Wolfram G, Davignon I, Smith MD, Brown MT, et al. Efficacy and safety of tanezumab added on to diclofenac sustained release in patients with knee or hip osteoarthritis: a double-blind, placebo-controlled, parallel-group, multicentre phase III randomised clinical trial. Ann Rheum Dis. 2014;73(9):1665–72. https://doi.org/10.1136/annrheumdis-2012-203164.
Walsh DA, Chapman V. Bisphosphonates for osteoarthritis. Arthritis Res Ther. 2011;13(5):128. https://doi.org/10.1186/ar3448.
Rodan GA, Fleisch HA. Bisphosphonates: mechanisms of action. J Clin Invest. 1996;97(12):2692–6. https://doi.org/10.1172/JCI118722.
Li HZ, Xu XH, Lu HD. Bisphosphonates reduce the risk of knee replacement: we need more analyses! Ann Rheum Dis. 2019;78(2):e15. https://doi.org/10.1136/annrheumdis-2018-213052.
Ozturk C, Atamaz F, Hepguler S, Argin M, Arkun R. The safety and efficacy of intraarticular hyaluronan with/without corticosteroid in knee osteoarthritis: 1-year, single-blind, randomized study. Rheumatol Int. 2006;26(4):314–9. https://doi.org/10.1007/s00296-005-0584-z.
Hartung DM, Touchette D. Overview of clinical research design. Am J Health Syst Pharm. 2009;66(4):398–408. https://doi.org/10.2146/ajhp080300.
Aranaz Andrés JM, Limón Ramírez R, Aibar Remón C, Gea-Velázquez de Castro MT, Bolúmar F, Hernández-Aguado I, et al. Comparison of two methods to estimate adverse events in the IBEAS Study (Ibero-American study of adverse events): cross-sectional versus retrospective cohort design. BMJ Open. 2017;7(10):e016546. https://doi.org/10.1136/bmjopen-2017-016546.
Skousgaard SG, Skytthe A, Möller S, Overgaard S, Brandt LP. Sex differences in risk and heritability estimates on primary knee osteoarthritis leading to total knee arthroplasty: a nationwide population based follow up study in Danish twins. Arthritis Res Ther. 2016;18:46. https://doi.org/10.1186/s13075-016-0939-8.
Acknowledgements
Not applicable.
Funding
This study is supported by Post-doctoral Research and Development Fund of West China Hospital, Sichuan University (2019HXBH090), Sichuan Science and Technology Program (2021JDRC0045, 2021YFS0164, 2021YJ0472, 2021JDRC0169), and Clinical Research Incubation Project of West China Hospital, Sichuan University (2019HXFH038).
Author information
Authors and Affiliations
Contributions
QX, GY and YC conceived the study, YC and BC designed the study forms, and GY and QX guided this study. BC searched the literature; YC, YT, HL, and YH screened the studies for inclusion and extracted data; YT, HL, and YH assessed methodological quality; YC and GY organized data. All authors drafted and revised the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study does not involve with ethics as it is a systematic review and meta-analysis.
Consent for publication
No patient involved.
Competing interests
All authors do not have any conflicts of interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
The supplementary tables and figures.
Additional file 2.
Predefined protocol of the study.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Cui, B., Chen, Y., Tian, Y. et al. Effects of medications on incidence and risk of knee and hip joint replacement in patients with osteoarthritis: a systematic review and meta-analysis. Adv Rheumatol 62, 22 (2022). https://doi.org/10.1186/s42358-022-00253-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s42358-022-00253-4