Abstract
Background
D-dimer is a well-known marker for abnormal hemostasis in acute ischemic stroke (AIS), indicating the presence of fibrin degradation due to thrombus formation and lysis. The diagnostic performance of D-dimer for different AIS types in the Indonesian population has not been established. The aim of this study is to compare the plasma D-dimer levels in three of the most common AIS subtypes in Indonesia; the cardioembolic, large artery atherosclerosis (LAA), and small-vessel occlusion (SVO), and to determine its most optimal diagnostic performance.
Results
In this cross-sectional study, 64 subjects with confirmed AIS diagnosis at the Wahidin Sudirohusodo General Hospital Makassar between June and October 2019 were recruited. Plasma D-dimer levels were measured and grouped according to the subtype of acute ischemic stroke based on the TOAST classification. A significant difference was observed between the D-dimer levels across the three AIS subtypes, with an average D-dimer of 2.93 ± 1.7, 1.27 ± 0.81, and 0.56 ± 0.46 µg/ml in the cardioembolic, LAA, and SVO subtypes, respectively. As a marker of cardioembolic stroke, an optimal cut-off was determined to be 1.52 µg/ml, yielding a sensitivity of 84.44% (CI 71.22–92.25% and specificity of 84.21% (CI 62.43–94.48%).
Conclusion
Plasma D-dimer levels varied significantly between the cardioembolic, LAA, and SVO subtypes of AIS, with the highest D-dimer level in the cardioembolic subtypes. As a marker of cardioembolic stroke, an optimal cut-off was determined to be 1.52 µg/mL, yielding a sensitivity and specificity of 84.44% and 84.21%, respectively.
Similar content being viewed by others
Introduction
Stroke continues to place a major burden on healthcare systems worldwide. Indonesia currently has the second highest mortality rate (193.3/100.000 person-years), and number of DALYs lost in Asia (3382.2/100.000 people) [1]. Acute ischemic stroke constitutes 87% of all strokes [2], and based on The Trial Of Org 10172 in Acute Stroke Treatment (TOAST), AIS can be classified into 5 subtypes [3,4,5]. In Indonesia, subtypes with the highest incidence include the cardioembolic, large artery atherosclerosis (LAA), and small-vessel occlusion (SVO) [6].
The speed and accuracy of decision-making in determining both the diagnosis and therapy of acute ischemic stroke (AIS) is essential, and helps forecast prognosis. The non-contrast computed tomography scan (CT scan) and magnetic resonance imaging (MRI) modalities have been used widely to assess AIS patients, with good sensitivity and specificity. However, examination is not always possible at the golden time of treatment, rendering many cases too late to receive intravenous thrombolytic therapy [7]. Additionally, for many low resource settings without adequate imaging facilities, alternative modalities may be needed to support the diagnosis.
One crucial aspect in the pathophysiology of ischemic stroke is hemostatic abnormality and thrombosis [8, 9]. As thrombosis and fibrin degradation occurs, the level of certain soluble markers may increase. An ideal biomarker of AIS should have sufficient sensitivity and specificity, can be detected at the point-of-care cost-effectively and quantitatively, and allow for prognostic assessment [10]. One marker is D-dimer, a soluble protein formed by the cross-linked fibrin network as it is degraded by plasmin [11, 12]. The D-dimer assay typically utilize monoclonal antibodies that recognize specific epitopes of D-dimer fragments using methods such as enzyme linked immunosorbent assay (ELISA), immunometric flow-through, whole blood agglutination (WBA), and latex agglutination (LA) [13]. Results below the reference value (500 ng/mL or 0.5 µg/mL) is often used to rule out suspicion of a thrombus [14,15,16], while higher levels indicate the presence of thrombus breakdown. The D-dimer test has a 100% sensitivity within 15 days after the onset of symptoms, meaning that it is more appropriate to utilize the test within acute settings [14].
The use of D-dimer in AIS has been evaluated extensively. Levels were significantly increased in patients with ischemic stroke compared to controls and relates with severity and the extent of infarct volume [2]. Some studies have also demonstrated the capacity of the D-dimer as a biomarker of the cardioembolic stroke subtype [17]. In Indonesia, studies on D-dimer as a marker of ischemic stroke has shown it to be correlated with infarct volume, NIHSS, mRS, and CNS scores [18, 19], although observations on the significance of the relationship have been inconsistent. The studies have also focused on its associations with clinical outcome, but has not extensively explored its patterns in relation to stroke classification, which may benefit the diagnostic process, clinical research, diagnosis, and can serve as a foundation for exploration of population specific genetic markers and risk factors [20]. In this study, we aimed to compare the levels of D-dimer among the three most common TOAST classes of AIS in the Indonesian population; the cardioembolic, LAA, and SVO subtypes. This study also aimed to determine the diagnostic performance of the assay for the detection of cardioembolic stroke.
Methods
Study design, participants, and clinical assessment
This was a cross-sectional study conducted at the Dr. Wahidin Sudirohusodo Hospital, in Makassar, Indonesia, between June and October 2019. The study has been approved by the Human Research Ethics Committee of the Medical Faculty of Hasanuddin University, South Sulawesi, Indonesia (Ethics number 513/UN4.6.4.5.31/PP36/2019).
The inclusion criteria in this study were: (1) patients with acute first-time ischemic stroke with an onset of ≤ 72 h based on history, physical examination, and CT-scan of the head; (2) age ≥ 18 years and ≤ 70 years; (3) has agreed to participate in the study with a signed consent letter by the patient or patient’s guardian. Clinical evaluation to obtain the acute ischemic stroke diagnosis includes history of neurological symptoms, confirmed with comprehensive neurological examination to detect neurological deficits by board-certified neurologists. The National Institute of Health Stroke Scale (NIHSS) was used to quantify the clinical evaluation. The radiological findings used to support the diagnosis were any signs of ischemia on CT-scan examination of the brain assessed by board-certified radiologists in our hospital.
Criteria for exclusion include: (1) patients diagnosed with sepsis upon hospital admission; (2) heart failure; (3) malignant disease; (4) severe malnutrition; (5) hemostasis disorders; (6) pregnant female patients; (7) patients diagnosed with deep vein thrombosis; (8) patients on anti-coagulants, or patients with heavy bleeding or severe anemia. Subjects were categorized based on previously described three TOAST categories of large artery atherosclerosis, cardioembolism, and small-vessel occlusion [5].
Laboratory analysis
Sample collection was performed on eligible subjects by first collecting 3 mL of venous blood into a vacutainer (BD vacutainer). Samples were then sent to the Clinical Pathology Laboratory at the Wahidin Sudirohusodo General Hospital in Makassar, Indonesia. The samples were centrifuged at 3500 rpm for 15 min and supernatants were used to measure D-dimer levels using latex agglutination (Sysmex 2500).
Statistical analysis
All data were analyzed using Graphpad Prism Version 9. Comparison of plasma D-dimer levels in ischemic stroke subtypes based on TOAST classification was assessed using the Kruskal–Wallis test, followed by post hoc Dunn’s multiple comparisons test. The Chi-square analysis was used to assess associations between normal or elevated D-dimer status with stroke subtypes, using previously established D-dimer cut-off levels for thromboembolism at 500 ng/mL or 0.5 µg/mL [14,15,16].
Upon establishing the differences across the three subtypes, we assessed the diagnostic value of D-dimer specifically for cardioembolic stroke using the receiver operating curve (ROC) analysis. A cut-off was determined based on the Youden’s index [21], and the sensitivity and specificity of D-dimers for cardioembolic stroke was measured based on said cut-off. A p-value < 0.05 was considered to indicate statistical significance for all tests.
Results
A total of 64 subjects were recruited for the study (Table 1) consisting of 34 (53.1%) males and 30 (46.9%) females. The mean age of the sample population was 58.5 ± 9.1 years of age, with 27 (42.2%) of subjects aged under 60 and 37 (57.8%) aged 60 years or above. The subjects were grouped based on the TOAST classification, with 19 (29.7%) samples classified as cardioembolic stroke, 24 (37.5%) as large artery atherosclerosis, and 21 (32.8%) as small-vessel occlusion. A majority (69%) of the patients in this population were smokers. When assessed based on the NIHSS stroke scale level of severity, we found that patients had either minor (25%), moderate (55%), or severe stroke (20%). The worst severity was found in the cardioembolic subtype, with a mean NIHSS score of 15.42 ± 3.42, followed by the LAA (7.7 ± 3.07) and SVO (4.57 ± 1.93) subtypes.
Table 2 shows that the mean plasma D-dimer level for AIS in general within the study population was 1.509 ± 1.44 µg/mL. The highest average D-dimer level was observed in the cardioembolic subtype (2.93 ± 1.7 µg/mL), followed by the atherosclerosis (1.27 ± 0.81 µg/mL) and lacunar (0.56 ± 0.46 µg/mL) types.
A significant difference was observed between the D-dimer levels across the three AIS subtypes (p < 0.0001, Kruskal–Wallis ANOVA). On post hoc Dunn’s multiple comparisons test, the most significant difference was observed between the cardioembolic versus lacunar subtypes (p < 0.0001), followed by the thrombosis versus lacunar (p = 0.0096) and the cardioembolic versus thrombosis (p = 0.0125) subtypes.
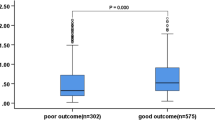
D-dimer levels within each ischemic stroke subtype were then further classified as normal (< 0.5 µg/mL) or elevated (≥ 0.5 µg/mL) based on the conventional normal values [14,15,16]. Results can be seen in Table 3, wherein the cardioembolic subtype had the least number (2 patients, 8.7%) of normal D-dimer levels, while the small-vessel occlusion had the highest number of normal D-dimer levels (Fig. 1).
Since results indicated that D-dimer levels were highest in the cardioembolic subtype, we performed a receiver operating curve (ROC) analysis regarding the diagnostic performance of D-dimer levels specifically for cardioembolic AIS detection. As shown in Fig. 2, the D-dimer marker showed an area under the curve (AUC) value of 0.87 (p < 0.0001). The optimal cut-off specifically for cardioembolic AIS was determined to be two times higher than the general cut-off at 1.52 µg/mL, yielding a sensitivity of 84.44% (CI 71.22–92.25% and specificity of 84.21% (CI 62.43–94.48%).
Discussion
Stroke is a major global health burden, with high incidence of mortality and morbidity. The outcome of stroke is highly influenced by the health system’s capacity to perform prompt diagnosis and management. Plasma D-dimer levels have been previously stipulated as a potential biomarker for the differentiation between patients with ischemic stroke and healthy controls. One of the first reports were by Osman et al. which showed that the mean D-dimer of AIS patients was more than twice the level of healthy controls (377.867 ± 113.289 ng/mL versus 142.000 ± 17.808) [22]. In Indonesia, research conducted by Mayke et al. was limited to whether the level of D-dimer can be used as a diagnostic parameter for acute ischemic stroke [23], but has not examined the relationship with stroke subtypes. Subsequent reports have demonstrated differences between D-dimer levels among AIS subtypes, although variations have been observed across different geographical and clinical subpopulations. In this study, we aimed to characterize the plasma D-dimer levels in three of the most common ischemic stroke subtypes in our Indonesian population.
The population in this study consisted of individuals with a mean age of 58.4 years old, with a slightly higher proportion of subjects in the age group of > 60 years old. This is consistent with studies such as Goldstein et al., which states that ischemic stroke risk increase with age, while the risk of intracerebral hemorrhage doubles every decade after the age of 55 years [24]. A slightly larger proportion of the subjects in this study were men. While this is consistent with previous studies [6] which associated the male gender with higher stroke occurrence due to the higher rates of other stroke risk factors in men suh as such as hypertension, smoking habits, coronary heart disease, dyslipidemia, and atrial fibrillation. However, the relationship between gender and AIS subtypes still requires further elucidation using epidemiological data with a larger dataset.
Out of the three AIS subtypes sampled in this study, the highest incidence was found for LAA (37.5%), followed by SVO (32.8%), and cardioembolic (29.7%) subtypes. This is consistent with previous local reports in Indonesia, reporting higher incidence for LAA relative to other subtypes [6]. Several other population-based studies have also confirmed increasing trends of LAA and SVO, associated with with increased smoking and high blood pressure [25]. However, studies in other populations have reported differently, showing that the cardioembolic subtype was most common [26].
In this study, we observed that plasma D-dimer levels were highest in the cardioembolic AIS subtype. In fact only two out of the 19 cardioembolic stroke subjects had a normal D-dimer level, while the rest were classified as high. This confirms the finding of previous studies, such as the study by Osman et al. who reported increased D-dimer in cardioembolic AIS and atrial fibrillation relative to other etiologies. In said study, the mean D-dimer of cardioembolic stroke subjects were 475 ± 82.88 ng/mL [22]. We have established the optimal D-dimer cut-off for cardioembolic stroke in the Indonesian population to be 1.52 µg/ml, which is similar albeit slightly lower than a previously established cut-off for predicting cardioembolic stroke in an Italian population which was found to be 2.00 µg/mL [27],
The cardioembolic subtypes differ from the LAA and SVO subtypes wherein in the last two subtypes, a higher percentage of subjects had a normal D-dimer level. The lowest D-dimer levels were found in the small-vessel occlusion subtypes. This is consistent with the theory stating that in lacunar subtypes of AIS ischemic stroke lacunar subtypes, a thrombus is too small to produce elevated D-dimers rendering levels that are within normal limits, and due to other causal possibilities for non-thrombotic mechanisms such as vascular degeneration, arterial hypertension, or diabetes [27, 28].
The findings confirm that higher D-dimer levels can be used as a marker for cardioembolic stroke. While this has been expressed by previously [26], this study confirms it in an Asian population. Until now, race-based differences in D-dimer levels still require further exploration, as some studies have emphasized the need for ethnicity-based approaches in the use of thrombogenicity markers [29]. Hence, this study contributes to the current discussion with particular focus on D-dimer levels in ischemic stroke within the South-East Asian population.
D-dimer is the final product of plasmin hydrolysis, following the cross-linking between fibrin monomers and thrombin activator XIII [15]. Under normal physiologic conditions, D-dimer levels are low in the peripheral circulation, but will rise in the event of thrombosis and secondary fibrinolysis, normalizing within 15–20 days of the thrombotic event and decrease gradually [30]. When an ischemic stroke occurs, the coagulation system's increased activity reflects thrombus formation. In the atrial or ventricular thrombus, locally stagnant circulation may lead to thrombus due to formation of fibrin-rich clots by clotting factors, which differs from the platelet-rich states of arterial thrombus formation wherein the formation of fibrin occurs secondary to the platelet activation [26, 31]. This may explain why more D-dimers are produced by fibrin degradation in the cardioembolic subtype [26].
Traditionally, small-vessel occlusion stroke subtypes are mainly caused by hyaline lipid changes in arterial damage due to hypertension or diabetes, with several studies suggesting that small-vessel occlusion subtype strokes are caused by atherosclerotic thrombotic occlusion in damaged arteries [6, 32]. However, the mechanism of secondary fibrinolysis is considered to be inferior to atherosclerotic thrombotic occlusion of the main arteries. Therefore, the highest D-dimer level is found in cases of ischemic stroke of cardioembolic type, and the lowest is in the case of ischemic stroke of the small-vessel occlusion subtype [27, 33].
This is the first study to determine the diagnostic performance of D-dimer specifically for cardioembolic stroke in Indonesia after first characterizing the D-dimer levels across the three most common AIS types in the region. There are several limitations to this study. Firstly, the sample size is relatively small and requires further confirmation in future studies with a larger set of subjects. Secondly, we only used 3 out of the 5 TOAST subtypes, and future studies may need to compare with the rest of the subtypes. Finally, no serial measurements were performed, and we only measured the D-dimer levels within 72 h of onset. Future studies will need to assess how the diagnostic performance stands after further progression of the AIS.
Conclusions
Plasma D-dimer levels varied significantly between the cardioembolic, LAA, and SVO subtypes of acute ischemic stroke. The highest D-dimer levels were observed in the cardioembolic subtype. As a marker of cardioembolic stroke, an optimal cut-off was determined to be 1.52 µg/ml, yielding a sensitivity of 84.44% (CI 71.22–92.25% and specificity of 84.21% (CI 62.43–94.48%).
Availability of data and materials
All datasets generated during the study are available by request to the corresponding author.
Abbreviations
- AIS:
-
Acute ischemic stroke
- CT-scan:
-
Computed tomography scan
- CNS:
-
Canadian neurological scale
- DALY:
-
Disability-adjusted life year
- ELISA:
-
Enzyme-linked immunosorbent assay
- LA:
-
Latex agglutination
- LAA:
-
Large artery atherosclerosis
- MRI:
-
Magnetic resonance imaging
- mRS:
-
Modified Rankin scale
- NIHSS:
-
National Institute of Health stroke scale
- ROC:
-
Receiver operating characteristics
- SVO:
-
Small-vessel occlusion
- TOAST:
-
The trial of org 10172 in acute stroke treatment
- WBA:
-
Whole blood agglutination
References
Venketasubramanian N, Yoon BW, Pandian J, Navarro JC. Stroke epidemiology in south, east, and south-east Asia: a review. J Stroke. 2017;19(3):286.
Abd-Elhamid YA, Tork MA, Abdulghani MO. Prognostic value of D-dimer measurement in patients with acute ischemic stroke. Egypt J Neurol Psychiatry Neurosurg. 2016;53(3):146.
Adams HP, Biller J. Classification of subtypes of ischemic stroke: history of the trial of org 10172 in acute stroke treatment classification. Stroke. 2015;46(5):e114-117.
Amarenco P, Bogousslavsky J, Caplan LR, Donnan GA, Hennerici MG. Classification of stroke subtypes. Cerebrovasc Dis. 2009;27(5):493–501.
Adams Jr HP, Bendixen BH, Kappelle LJ, Biller J, Love BB, Gordon DL, et al. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke. 1993;24(1):35–41.
Harris S, Sungkar S, Rasyid A, Kurniawan M, Mesiano T, Hidayat R. Stroke Research and Treatment. 2018 [cited 2019 May 8]. TOAST Subtypes of Ischemic Stroke and Its Risk Factors: A Hospital-Based Study at Cipto Mangunkusumo Hospital, Indonesia. Available from: https://www.hindawi.com/journals/srt/2018/9589831/.
Whiteley W, Tseng MC, Sandercock P. Blood biomarkers in the diagnosis of ischemic stroke: a systematic review. Stroke. 2008;39(10):2902–9.
Berge E, Friis P, Sandset PM. Hemostatic activation in acute ischemic stroke. Thromb Res. 2001;101(2):13–21.
Barber M, Langhorne P, Rumley A, Lowe GD, Stott DJ. Hemostatic function and progressing ischemic stroke: D-dimer predicts early clinical progression. Stroke. 2004;35(6):1421–5.
Guo Y, Li P, Guo Q, Shang K, Yan D, Du S, et al. Pathophysiology and biomarkers in acute ischemic stroke–a review. Trop J Pharm Res. 2013;12(6):1097–105.
Yao T, Tian BL, Li G, Cui Q, Wang CF, Zhang Q, et al. Elevated plasma D-dimer levels are associated with short-term poor outcome in patients with acute ischemic stroke: a prospective, observational study. BMC Neurol. 2019;19(1):175.
Adam SS, Key NS, Greenberg CS. D-dimer antigen: current concepts and future prospects. Blood J Am Soc Hematol. 2009;113(13):2878–87.
Tripodi A. D-dimer testing in laboratory practice. Clin Chem. 2011;57(9):1256–62.
Soomro AY, Guerchicoff A, Nichols DJ, Suleman J, Dangas GD. The current role and future prospects of D-dimer biomarker. Eur Heart J-Cardiovasc Pharmacother. 2016;2(3):175–84.
Johnson ED, Schell JC, Rodgers GM. The D-dimer assay. Am J Hematol. 2019;94(7):833–9.
Favresse J, Lippi G, Roy PM, Chatelain B, Jacqmin H, Ten Cate H, et al. D-dimer: preanalytical, analytical, postanalytical variables, and clinical applications. Crit Rev Clin Lab Sci. 2018;55(8):548–77.
Zi WJ, Shuai J. Plasma D-dimer levels are associated with stroke subtypes and infarction volume in patients with acute ischemic stroke. PLoS ONE [Internet]. 2014;9(1).
Sitepu M, Nasution D, Arina C. Hubungan D-dimer, Gula Darah, dan Asam Urat dengan Volume Infark dan Keluatan Pada Stroke Iskemik. Neurona. 2014;4(31):240–5.
Darmawaty, Arif M, Pakasi R, Muis A, Bahar B. Hubungan kadar d-dimer dengan skor Canadian neurological scale (cns) pada penderita strok iskemik akut. Pasca Sarj Unhas. 2011.
Chen P, Gao S, Wang Y, Xu A, Li Y, Wang D. Classifying ischemic stroke, from TOAST to CISS. CNS Neurosci Ther. 2012;18(6):452–6.
Fluss R, Faraggi D, Reiser B. Estimation of the Youden Index and its associated cutoff point. Biom J J Math Methods Biosci. 2005;47(4):458–72.
Osman L, Gad K, Fathy M, Sobh M, Iman M, Fauad A. Assessment of ischemic stroke subtypes using D dimer. AAMJ. 2013;4:295–306.
Mayke Y, Aman AK, Anwar Y. D-dimer plasma levels in ishemic stroke. Indones J Clin Pathol Med Lab. 2015;21(2):183–6.
Goldstein LB, Bushnell CD, Adams RJ, Appel LJ, Braun LT, Chaturvedi S, et al. Guidelines for the primary prevention of stroke: a guideline for healthcare professionals from the American heart association/American stroke association. Stroke. 2011;42(2):517–84.
Krishnamurthi RV, Barker-Collo S, Parag V, Parmar P, Witt E, Jones A, et al. Stroke incidence by major pathological type and ischemic subtypes in the Auckland regional community stroke studies. Stroke. 2018;49(1):3–10.
Montaner J, Perea-Gainza M, Delgado P, Ribó M, Chacón P, Rosell A, et al. Etiologic diagnosis of ischemic stroke subtypes with plasma biomarkers. Stroke. 2008;39(8):2280–7.
Ageno W, Finazzi S, Steidl L, Biotti MG, Mera V, d’Eril GM, et al. Plasma measurement of D-dimer levels for the early diagnosis of ischemic stroke subtypes. Arch Intern Med. 2002;162(22):2589–93.
Park YW, Koh EJ, Choi HY. Correlation between serum d-dimer level and volume in acute ischemic stroke. J Korean Neurosurg Soc. 2011;50(2):89–94.
Kim HK, Tantry US, Park HW, Shin ES, Geisler T, Gorog DA, et al. Ethnic difference of thrombogenicity in patients with cardiovascular disease: a Pandora box to explain prognostic differences. Korean Circ J. 2021;51(3):202–21.
Kelly J, Rudd A, Lewis RR, Hunt BJ. Plasma D-dimers in the diagnosis of venous thromboembolism. Arch Intern Med. 2002;162(7):747–56.
Nagao T, Hamamoto M, Kanda A, Tsuganesawa T, Ueda M, Kobayashi K, et al. Platelet activation is not involved in acceleration of the coagulation system in acute cardioembolic stroke with nonvalvular atrial fibrillation. Stroke. 1995;26(8):1365–8.
Yaghi S, Raz E, Yang D, Cutting S, Grory BM, Elkind MS, et al. Lacunar stroke: mechanisms and therapeutic implications. J Neurol Neurosurg Psychiatry. 2021;92(8):823–30.
Melake MS, El-Kabany RA, Al-Emam AI, El-Shereef AM, Okda M. The role of D-dimer, fibrinogen and C-reactive protein as plasma biomarkers in acute ischemic stroke. J Neurol Res. 2016;5(6):277–82.
Acknowledgements
We would like to thank all families who have participated in this study
Funding
The study received no specific funding.
Author information
Authors and Affiliations
Contributions
MA conceptualized and supervised the study, analyzed the data, drafted and finalized the manuscript. FD performed the data collection and analysis. GVS performed the data analysis, revised, and finalized the manuscript. JT, AKB, and SA supervised the study and revised the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was conducted according to the guidelines of the Declaration of Helsinki and was approved by the Ethics Committee of the Faculty of Medicine, Hasanuddin University.
Consent for publications
All subjects have provided consent for publication.
Competing interests
The authors declare no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Akbar, M., Damayanti, F., Tammasse, J. et al. Plasma D-dimer as a biomarker for the early classification of common acute ischemic stroke subtypes in Indonesia. Egypt J Neurol Psychiatry Neurosurg 59, 115 (2023). https://doi.org/10.1186/s41983-023-00720-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41983-023-00720-9