Abstract
Background
Epilepsy and primary headache disorders are two relatively common neurological disorders and their relationship is still a matter of debate. We aimed to estimate the prevalence and clinical features of primary headache disorders in patients with epilepsy.
Methods
62 subjects aged ≥ 18 years were recruited from the hospital’s neurology outpatient clinic in the period from January to April 2018. The subjects were further divided into two equal groups, epileptics and non-epileptics. They underwent a semi-structured interview including the ILAE 2017 epilepsy classification and the ICHD III-beta criteria for headache. Patients' demographic data and clinical characteristics of epilepsy and headache and temporal relationships between them were assessed. Patients who experienced headaches were grouped based on the type of headaches and on whether their headaches occurred in the pre-ictal, post-ictal or inter-ictal period.
Results
Primary headache disorders were more common in epileptic group (61.3%) than the non-epileptic group (32.2%) (p = 0.021). The tension-type headache was the most common (45.2%) followed by migraine-type headache (12.9%) in the epileptic group. Post-ictal headache was the most common type (29%). Inter-ictal headaches were significantly related to "focal to bilateral tonic–clonic" seizures (p = 0.046). The prevalence of headache among patients on polytherapy (69.2%) was higher than that of patients on monotherapy (52.9%).
Conclusions
In this study, headache was more common in epileptic patients. TTH was the most represented type of headache in patients with epilepsy. Headache occurred in patients with epilepsy most frequently during the post-ictal period.
Similar content being viewed by others
Introduction
Primary headache disorders and epilepsy are two of the most common neurological disorders. They both do share some similarities as being episodic in nature and could be triggered by the same triggers, such as as sleep deprivation. The pathogenesis of both conditions includes the modification of membrane channel functions and the imbalance of excitatory and inhibitory factors [1]. Several studies were done to test the relation between headache and epilepsy but with the main focus on migraine [2,3,4,5].
Headache and epilepsy can be classified according to their temporal relation into inter-ictal headache (inter-IH) or peri-ictal headache (peri-IH). Inter-IH is not temporally related to seizures, whereas peri-IH manifests in their time frame (pre-ictal, ictal and post-ictal) [6, 7].
El-Sherbiny et al. reported the one-year prevalence of primary headache disorders to be 51.4 with episodic tension-type headache the most common [8]. Several studies were done to estimate the prevalence of epilepsy in different governorates in Egypt, it ranged from 5.5/1000 to 6.9/1000 [9, 10].
The purpose of this study is to investigate the prevalence and characteristics of primary headache disorders in patients with epilepsy, and how it differs when compared to the prevalence of primary headache disorders in the non-epileptic population which can lead to a better understanding of the relationship between those conditions which can reflect on management.
Methods
The study was carried out as a case–control cross-sectional analytic study at the neurology outpatient clinic. The target population included adults attending outpatient neurology clinic from January to April 2018.
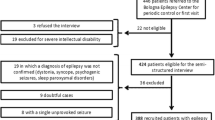
Sixty-two subjects were recruited and divided into two equal groups, one for subjects with epilepsy and the other for non-epileptic subjects. We excluded patients who had arrived for a first visit and proved not to be affected by epilepsy (i.e., psychogenic non-epileptic seizures, syncope), patients with a doubtful epilepsy diagnosis, patients who had only a single seizure, patients who had secondary headaches, and patients with severe mental retardation, behavioral abnormalities, and learning disabilities. The control (non-epileptic) group of age and sex-matched, who had no objective clinical nor paraclinical symptoms/signs of epilepsy.
A diagnosis of epilepsy and epileptic syndromes according to the 2017 International League Against Epilepsy (ILAE) Commission report [11] and types of seizures were classified as primary generalized, focal with or without impaired awareness and focal to bilateral tonic–clonic.
Headache was then classified according to the International Classification of Headache Disorders, 3rd b-version (ICHD-3b) [12] into tension-type headache (TTH) and migraine. Headache severity was assessed using the headache impact test (HIT-6) [13]. If the patient had more than one type of headache, all were assessed and included. If the patient has had previous or recurrent headaches, the previous diagnosis (if any) was identified.
Patients’ demographics, epilepsy duration, frequency of seizures, types of headache, the current antiepileptic drugs (AEDs) used, and electroencephalography (EEG) findings. Seizures’ severity was assessed using the seizure severity index (SSI) [14].
The temporal relationship between headaches and seizures was recorded. Timing of headache in epileptic subjects in relation to seizures is classified into inter-ictal headache (inter-IH) or peri-ictal headache (peri-IH). Peri-IH is further divided into pre-ictal, ictal, and post-ictal headache [6, 15]. A pre-ictal headache was defined as a headache starting not more than 24 h before the seizure and lasting until the onset of a seizure. Ictal headache was present exclusively during the seizure. A post-ictal headache was defined as a headache starting within 3 h after a seizure and ceasing within 72 h after the attack. Inter-ictal (inter-IH) headache is defined as all headaches that manifested within a time of the epileptic seizures and whose attacks were not temporally related to an epileptic seizure (more than 24 h before or more than 72 h after the epileptic seizure) [6, 15].
The study protocol was approved by the ethics committee of the faculty of Medicine in September 2017. The purpose of the study was explained and informed written consent was taken before taking any data or doing any investigations. The participants were informed that their participation was voluntary and that they could withdraw from the study at any time without consequences. The participants were assured that all data will be considered confidential and will not be used outside this research.
The data were transferred to IBM SPSS Statistics software, version 20. The assessment of the study data included descriptive statistics (mean, standard deviation) for numeric variables, and frequency distribution for categorical variables. The relationship between two categorical variables was assessed with the Chi-squared test. p-value is considered as significant when p < 0.05 and highly significant when p < 0.01.
Results
The study comprised 62 patients (32 females, 30 males). The patient’s demographics and clinical characteristics relevant to epilepsy and headaches are shown in Tables 1 and 2, respectively.
Headache has a higher prevalence (61.3%) in the epileptic group than the non-epileptic group (32.2%) which is statistically significant (p = 0.021) (Table 3). Of those patients with epilepsy who experienced headaches, post-ictal headaches were most frequent (29%) followed by inter-ictal headaches (19.4%). In the epileptic group, we found the prevalence of tension-type headache (TTH) being the most frequent (45.5%) followed by migraine (12.9%).
When considered based on seizure type, inter-ictal headaches were significantly higher (p = 0.04) in patients with focal to bilateral tonic–clonic seizures, compared to those with focal and primary generalized seizures; there was no relationship between the types of seizure and post-ictal or pre-ictal headaches (Table 4).
Seventeen subjects (56.7%) were on monotherapy, 13 subjects (43.3%) were on polytherapy and one subject wasn’t receiving any medication. Sodium valproate (53.3%) is the most commonly used followed by carbamazepine (40%), lamotrigine (26.7%), phenytoin (16.7%), oxcarbazepine (10%), and levetiracetam (6.7%).
Headache was more common in subjects on polytherapy (69.2%) than those on monotherapy (52.9%). There is no statistically significant relationship between the type of medication and type of headache. According to the headache severity index (HIT-6), substantial impact of headache was more common in the monotherapy group (44.4%) than the polytherapy group (11.1%), with no statistical significance (p = 0.48) (Table 5).
There is no statistically significant relationship between the type of headache and seizures severity (p = 0.189). There is no statistically significant relation between EEG findings and type of headache (p = 0.865).
Discussion
Although headaches are a typical symptom in patients with epilepsy, they are usually overlooked by patients and physicians. Understanding both conditions as comorbidities and establishing their true prevalence is expected to increase the awareness of patients and physicians, and to establish new treatment strategies in this regard.
Primary headache disorders had a higher prevalence (61.3%) in the epileptic group than the non-epileptic group (32.2%) which is statistically significant (p = 0.021). This is similar to what Wang et al. found in 2014 reporting almost the same prevalence of primary headaches among patients with epilepsy (60.1%) [16]. This was slightly higher than what Mainieri et al. found in their 2015 study that was 54% [17]. Cilliler et al. at 2017 also found the prevalence of primary headaches among patients with epilepsy to be 56.4% [5].
Tension-type headache was the most frequent primary headache disorder (45.2%) among epileptic subjects in this study and that was much higher than its prevalence in the non-epileptic group (22.6%). Seo et al. in their 2016 study found the prevalence of TTH among epileptics to be 50% [18] while Mameniskiene et al. reported a 39% prevalence of TTH [19]. On the other hand, Cilliler et al. and Mainieri et al. reported a much lower incidence of TTH (17.2%) [5] and (18.56%) [17], respectively.
Few studies have addressed TTH and epilepsy and no hypotheses on the relation between the two diseases have been put forward.
The second most common type of primary headache in our study was migraine (12.9%) which is slightly higher than the non-epileptic group (9.6%), but not statistically significant. The prevalence of migraine in patients with epilepsy varied markedly in the literature and was reported as 8–24% [2,3,4, 20, 21]. Another study reported migraine-type headaches in up to 32.9% of the patients [22]. The low prevalence of migraine headaches may be explained by the frequent use of valproate (53.3%) in our study sample, which is prescribed as one of the preventive treatments for migraine. Cortical spreading depression (CSD) is postulated as the mechanism linking both migraine and epilepsy [23].
Post-ictal headache was the most common type in our study reported in nine subjects (29%), all of them had a tension-type headache. This suggests that TTH could develop due to proprioceptive stimulants from muscles caused by motor symptoms that occur during a seizure [3]. The post-ictal headache frequency reported in our study was consistent with the post-ictal headache percentages of 19.7–41% reported by previous studies [5, 16, 17].
Pre-ictal headache was found in one case (3.2%). Pre-ictal headaches may be under-reported by patients as a result of being masked by the epileptic seizure itself, so the patients are unable to recall precisely the preceding events.
We found a significant relationship between the type of seizure and timing of headache with inter-ictal headaches were significantly related to “focal to bilateral tonic–clonic” seizures (p = 0.046). There was no relationship between the types of seizure and post-ictal or pre-ictal headaches. Cilliler et al. found that pre-ictal headaches were significantly higher (p = 0.016) in patients with primary generalized seizures [5].
The prevalence of headaches among patients on polytherapy (69.2%) was higher than of the monotherapy group (52.9%). This is consistent with previous studies reporting that the frequency of headaches was higher in patients receiving polytherapy, and suggested that headaches could be frequent in refractory patients using multidrug therapies [17, 24].
According to the seizures severity index (SSI), most of the cases were mild (58.2%); five were moderate (41.75), and one was a severe case. There was no significant relationship between the type of headache and seizures' severity (p = 0.189).
Limitations of the study were relatively small sample size. The retrospective assessment of headaches can lead to a recall bias, especially for peri-IH in patients who had their last seizure a long time before the interview. For this reason, the prevalence of pre-IH may be underestimated in the current study.
Conclusions
In conclusion, the prevalence of primary headaches is high among epileptic patients. Although headache may have any temporal relationship with one seizure attack, post-ictal headache is more common in patients with active epilepsy and undertreated. Physicians should ask for PIH and offer specific analgesic treatment. Considering such kind of co-morbidity can result in an appropriate drug selection for both epilepsy and headache.
Availability of data and materials
The paper is a part of thesis conducted in the Faculty of Medicine, Suez Canal University, and approved by its ethical committee. The data can be publicly available at the Faculty of Medicine, Suez Canal University.
Change history
12 July 2022
A Correction to this paper has been published: https://doi.org/10.1186/s41983-022-00519-0
Abbreviations
- Inter-IH:
-
Inter-ictal headache
- Peri-IH:
-
Peri-ictal headache
- ILAE:
-
International League Against Epilepsy
- ICHD-3b:
-
International Classification of Headache Disorders, 3rd b-version
- HIT-6:
-
Headache impact test
- AED:
-
Antiepileptic drugs
- EEG:
-
Electroencephalography
- SSI:
-
Seizure severity index
- TTH:
-
Tension-type headache
References
Mainieri G, Cevoli S, Giannini G, Zummo L, Leta C, Broli M, et al. Headache in epilepsy: prevalence and clinical features. J Headache Pain. 2015;16:556.
Bauer PR, Carpay JA, Terwindt GM, Sander JW, Thijs RJ, Haan J, Visser GH. Headache and epilepsy. Curr Pain Headache Rep. 2013;17(8):351. https://doi.org/10.1007/s11916-013-0351-x.
Caminero A, Manso-Calderon R. Links between headaches and epilepsy: current knowledge and terminology. Neurologia (Barcelona, Spain). 2014;29(8):453–63.
Leniger T, Isbruch K, von den Driesch S, Diener HC, Hufnagel A. Seizure-associated headache in epilepsy. Epilepsia. 2001;42(9):1176–9. https://doi.org/10.1046/j.1528-1157.2001.37500.x.
Çilliler AE, Güven H, Çomoğlu SS. Epilepsy and headaches: further evidence of a link. Epilepsy Behav. 2017;70(Pt A):161–5. https://doi.org/10.1016/j.yebeh.2017.03.009.
Ito M, Nakamura F, Honma H, Takeda Y, Kobayashi R, Miyamoto T, et al. A comparison of post-ictal headache between patients with occipital lobe epilepsy and temporal lobe epilepsy. Seizure. 1999;8(6):343–6.
Ito M, Schachter SC. Frequency and characteristics of interictal headaches in patients with epilepsy. J Epilepsy. 1996;9:223.
El-Sherbiny NA, Masoud M, Shalaby NM, Shehata HS. Prevalence of primary headache disorders in Fayoum Governorate, Egypt. J Headache Pain. 2015;16.
El-Tallawy HN, Farghaly WM, Shehata GA, Abdel-Hakeem NM, Rageh TA, Abo-Elftoh NA, et al. Epidemiology of epilepsy in New Valley Governorate, Al Kharga District. Egypt Epilepsy Res. 2013;104(1–2):167–74.
Hashem S, Al-Kattan M, Ibrahim SY, Shalaby NM, Shamloul RM, Farrag M. Epilepsy prevalence in Al-Manial Island, Egypt. A door-to-door survey. Epilepsy Res. 2015;117:133–7.
Scheffer IE, Berkovic S, Capovilla G, Connolly MB, French J, Guilhoto L, et al. ILAE classification of the epilepsies: position paper of the ILAE Commission for Classification and Terminology. Epilepsia. 2017;58(4):512–21.
Headache Classification Committee of the International Headache Society (IHS). The International Classification of Headache Disorders, 3rd edition (beta version). Cephalalgia. 2013;33(9):629–808. https://doi.org/10.1177/0333102413485658.
Kosinski M, Bayliss MS, Bjorner JB, Ware JE, Garber WH, Batenhorst A, et al. A six-item short-form survey for measuring headache impact: the HIT-6™. Qual Life Res. 2003;12(8):963–74.
Sancho J, Pena P, Rufo M, Palacios G, Masramon X, Rejas J. Health and non-health care resources use in the management of adult outpatients with drug-resistant epilepsy in Spain: a cost-of-illness study (LINCE study). Epilepsy Res. 2008;81(2–3):176–87.
Ito M, Schachter SC. Frequency and characteristics of interictal headaches in patients with epilepsy. J Epilepsy. 1996;9(2):83–6.
Wang XQ, Lang SY, He MW, Zhang X, Zhu F, Dai W, et al. High prevalence of headaches in patients with epilepsy. J Headache Pain. 2014;15.
Mainieri G, Cevoli S, Giannini G, Zummo L, Leta C, Broli M, et al. Headache in epilepsy: prevalence and clinical features. J Headache Pain. 2015;16(1):72.
Seo JH, Joo EY, Seo DW, Hong SB. Correlation between headaches and affective symptoms in patients with epilepsy. Epilepsy Behav. 2016;60:204–8.
Mameniskiene R, Karmonaite I, Zagorskis R. The burden of headache in people with epilepsy. Seizure. 2016;41:120–6.
Lipton RB, Ottman R, Ehrenberg BL, Hauser WA. Comorbidity of migraine: the connection between migraine and epilepsy. Neurology. 1994;44(10 Suppl 7):S28-32.
Velioğlu SK, Ozmenoğlu M. Migraine-related seizures in an epileptic population. Cephalalgia. 1999;19(9):797–801. https://doi.org/10.1046/j.1468-2982.1999.1909797.x.
Gameleira FT, Ataíde L Jr, Raposo MC. Relations between epileptic seizures and headaches. Seizure. 2013;22(8):622–6. https://doi.org/10.1016/j.seizure.2013.04.016.
Parisi P. Why is migraine rarely, and not usually, the sole ictal epileptic manifestation? Seizure. 2009;18(5):309–12.
Duchaczek B, Ghaeni L, Matzen J, Holtkamp M. Interictal and periictal headache in patients with epilepsy. Eur J Neurol. 2013;20(10):1360–6.
Acknowledgements
Not applicable.
Funding
No funding was received.
Author information
Authors and Affiliations
Contributions
AO was responsible for the design of the study and guidance, follows up the final revision, and prepares the paper’s final revision. IY was responsible for the guidance and follows up the final revision. MO was responsible for the guidance and follows up the final revision. MA was responsible for the practical work, was involved in the design of the study, and performed the statistical analysis. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study protocol was approved by the ethics committee of the faculty of Medicine of Suez Canal University September, 2017. The purpose of the study was explained and an informed written consent was taken before taking any data or doing any investigations. The participants were informed that their participation was voluntary and that they could withdraw from the study at any time without consequences. The participants were assured that all data will be considered confidential and will not be used outside this research. At the end of this study, records will be destroyed appropriately.
Consent for publication
All participants had signed an informed consent to participate and for the data to be published.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Osama, A., Orabi, M., Yassine, I. et al. Primary headache disorders in epileptic adults. Egypt J Neurol Psychiatry Neurosurg 58, 65 (2022). https://doi.org/10.1186/s41983-022-00498-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41983-022-00498-2