Abstract
Background
significance of incidental thyroid 2-deoxy-2-[18F]fluoro-D-glucose ([18F]FDG) uptake on positron emission tomography/computed tomography (PET/CT) scans remains controversial. We aimed to evaluate the ability of [18F]FDG-PET/CT texture analysis to predict final diagnosis in thyroid incidentaloma.
Methods
We retrospectively evaluated medical records of all patients who performed a [18F]FDG-PET/CT from January 2012 to October 2016. Those patients who presented a thyroid incidentaloma described in the medical records and performed a fine needle aspiration in our institution were considered for the analysis. Cytological and/or histological results were used as reference standard to define the final diagnosis. In case of negative cytology, the nodule was considered benign. In case of non-diagnostic or inconclusive results ultrasound, follow-up and further cytology/histology were used as final diagnosis. For suspected or positive cytological result, histology was used as reference standard. PET images were segmented using a General Electric AW workstation running PET VCAR software (GE Healthcare, Waukesha, WI, USA) settled with a threshold of 40% SUVmax. LifeX software (http://www.lifexsoft.org) was used to perform texture analysis. Statistical analysis was performed with R package (https://www.r-project.org).
Results
We identified 55 patients with incidental thyroid [18F]FDG uptake. Five patients were excluded from the analysis because a final diagnosis was not available. Thirty-two out of 50 patients had benign nodules while in 18/50 cases a malignancy (primary thyroid cancer = 15, metastases = 3) was diagnosed. Conventional PET parameters and histogram-based features were calculated for all 50 patients, while other matrices-based features were available for 28/50 patients. SUVmax and skewness resulted significantly different in benign and malignant nodules (p = 0.01 and = 0.02, respectively). Using ROC analysis, seven features were identified as potential predictors. Among all the textural features tested, skewness showed the best area under the curve (= 0.66). SUV-based parameters resulted in the highest specificity while MTV, TLG, skewness and kurtosis, as well as correlationGLCM resulted better in sensitivity.
Conclusions
[18F]FDG-PET/CT texture analysis seems to be a promising approach to stratify the patients with thyroid incidentaloma identified on PET scans, with respect to the risk of the diagnosis of a malignant thyroid nodule and thus, could refine the selection of the patients to be referred for cytology.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Background
Incidentalomas are findings on an imaging test performed for other reasons, for which there are no matching symptoms in the patient (Davies et al. 2016). Published reports estimated the prevalence of thyroid incidentalomas on [18F]FDG-PET images between 1.2% and 4.3% (Rigo et al. 1996; Mitchell and Parangi 2005; Liu et al. 2010). These data are in line with a recent meta-analysis which reported a prevalence of thyroid incidentalomas of 1.8% (3659 cases out of 197,296 [18F]FDG-PET/CT examinations), of which a third (36.6%) were evaluated with cytopathology or histopathology (Nayan et al. 2014). Although the overall incidence of thyroid incidentalomas detected on PET imaging is low, the chance of malignancy among incidentalomas detected by [18F]FDG is higher than incidental nodules discovered with other imaging modalities, with a chance for malignancy ranging from 14 to 59% (Gavriel et al. 2015; Lee et al. 2014; Demir et al. 2016; Chun et al. 2015; Are et al. 2007; Pagano et al. 2011; Cohen et al. 2001; Nilsson et al. 2011). Nonetheless, we have a limited understanding of the incidentaloma natural history (Davies et al. 2016). Therefore, the differentiation between malignant and benign thyroid lesions is crucial to avoid unnecessary procedures, to improve the quality of life of patients, and to reduce healthcare costs.
Many researchers postulated that malignant lesions tend to show higher [18F]FDG uptake (i.e., SUVmax) than that of benign lesions (Soelberg et al. 2012). However, it is not easy to differentiate malignancy from benignity using maximum standardized uptake value (SUVmax) only (Demir et al. 2016; Chun et al. 2015). Some authors proposed the evaluation of other parameters in addition to SUVmax of the thyroid incidentaloma, such as the target/background, the target/blood-pool, and the target/liver ratios (Barrio et al. 2016). Also the pattern of [18F]FDG uptake (focal versus diffuse) together with the elastography score (≥ 4) and some ultrasound findings (echogenicity, spot microcalcifications, color-flow Doppler pattern) have been tested (Demir et al. 2016). Dual time point PET imaging has been proposed as alternative method to overcome the low specificity of SUVmax in the differentiation of benign from malignant lesions, including thyroid incidentalomas (Lee et al. 2014). However, all these approaches were not validated and, they are not generally accepted. Therefore, fine-needle aspiration (FNA) remains the procedure of choice to define the diagnosis. If the nodule is benign on cytology, further immediate diagnostic studies or treatment are not required; while if cytology results diagnostic for malignancy, surgery is generally recommended. For a nodule with a non-diagnostic cytology result, FNA should be repeated (Haugen et al. 2016).
In the past years, interest has grown in texture analysis of medical images that provide numerous quantitative and semi-quantitative parameters capturing the inhomogeneity of the tissues. This analysis seems able to provide a better characterization of cancer lesions, and some prognostic information about the aggressiveness of disease using conventional medical imaging (Buvat et al. 2015). No data on [18F]FDG-PET/CT images texture analysis in thyroid have been reported in the literature, with the exception of Kim et al. (Kim and Chang 2015). They evaluated some parameters, including a feature named “heterogeneity factor”, derived from the histogram of intensities of uptake within the lesion, in patients with a thyroid nodule (Kim and Chang 2015).
The aim of this study was to investigate the ability of texture analysis on [18F]FDG-PET/CT to predict final diagnosis in thyroid incidentalomas.
Methods
Patients
We retrospectively evaluated the medical records of all the patients who performed a [18F]FDG-PET/CT from January 2012 to October 2016. Those patients who presented thyroid [18F]FDG uptake (described in the medical record) and performed a cytological examination in our institution were considered for the analysis. According to good clinical practice in use in our institution, cytological examination was performed in case of doubtful or suspected ultrasound findings (i.e., solid nodule, microcalcifications; hypoechogenicity; increased nodular vascularity; irregular or infiltrative margins; taller than wide on transverse view).
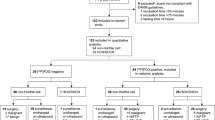
Demographics, data relating to [18F]FDG-PET/CT scan and its findings, cytological results, biochemical data, surgery details and histopathology (when available) were reviewed. Among all subjects who underwent a [18F]FDG-PET/CT examination (17,104 scans) and had a thyroid uptake on the images (453 subjects), we identified 55 patients (male:female = 20:35; age 62 ± 15 years) that performed a cytological examination in our institution. Indication for [18F]FDG-PET/CT was oncological in 50 cases and non-oncological in the remaining 5 cases (2 vasculitis, 1 sarcoidosis, 1 fever of unknown origin, 1 suspected orthopedic infection). In the oncologic group, [18F]FDG-PET/CT was performed for diagnosis or staging in 26 cases, re-staging in 14 cases, and follow-up in 10 cases.
Ultrasound-guided FNA was performed according to the standard procedure in use in our institution. Cytological results were reported according to the SIAPEC-IAP 2007 classification, and grouped in 5 diagnostic categories defined as TIR1 or non-diagnostic, TIR2 or negative for malignant cells, TIR3 or inconclusive/indeterminate, TIR4 or suspicious for malignancy, TIR5 or diagnostic of malignancy (i.e., papillary, medullary and anaplastic carcinomas, lymphomas and metastasis) (Fadda et al. 2010). All cytological results reported according the update version of the SIAPEC-IAP 2014 classification (Nardi et al. 2014), were reclassified for the present analysis using the SIAPEC-IAC 2007 classification. Cytology and/or histology was used as reference standard to define the final diagnosis. In case of negative cytology (TIR2), no further studies were immediately performed, and the nodule was considered benign. In case of non-diagnostic (TIR1) or doubtful (TIR3) results, ultrasound follow-up and further cytological samples or histology were used as final diagnosis. In the case of suspected (TIR4) or positive (TIR5) cytological result, histology was used as reference standard. All cases resulted as TIR1 (n = 1) or TIR3 (n = 4) in which a further cytology/histology was not available (3 patients lost at follow-up and 2 patients had progressive disease for breast cancer and multiple myeloma, respectively), were excluded from the analysis, therefore 50 patients (male:female = 18:32; age 63 ± 15 years) were overall included. This retrospective observational study was reviewed and approved by the Local Ethics Committee.
[18F]FDG PET/CT acquisition protocol
[18F]FDG-PET/CT image acquisition was performed according to the European Association of Nuclear Medicine (EANM) guidelines (Boellaard et al. 2014). Images were acquired 60 ± 5 min after [18F]FDG administration, in the fasting state using an integrated PET/CT scanner, either a Siemens Biograph LS 6 scanner (Siemens, Munich, Germany) equipped with LSO crystals and a six-slice CT scanner, or a GE Discovery PET/CT 690 equipped with LYSO crystals and a 64-slice CT scanner (General Electric Healthcare, Waukesha, WI, USA). Both scanners are EARL certified (http://www.eanm.org) and images were processed in order to minimize differences between semi-quantitative evaluation.
Image analysis
Whole-body [18F]FDG-PET/CT images were interpreted visually by two experienced nuclear medicine physicians in consensus. Thyroid incidentaloma was defined as focal thyroid uptake (i.e., increased [18F]FDG uptake compared to surrounding or contralateral thyroid parenchyma) identified on [18F]FDG-PET/CT study incidentally and was described as unilateral (i.e., occurred in less than one lobe) and bilateral (i.e., involving both thyroid lobes) according to the thyroid uptake pattern.
PET images were segmented using a General Electric AW workstation running PET VCAR software (GE Healthcare, Waukesha, WI, USA) settled with a threshold of 40% SUVmax. The region of interest (ROI), set in the target tissue (i.e., incidentaloma), was saved in 3D. Segmented images were saved in DICOM-RT format together with the corresponding [18F]FDG-PET/CT images. The entire dataset was then analyzed to extract a number of textural features by means of the LifeX package (http://www.lifexsoft.org) (Orlhac et al. 2016). LifeX was set up using the following input parameters for calculation of features: 64 Gy levels to resample the ROI content which was performed in absolute terms between a minimum of 0 and a maximum of 20 (Orlhac et al. 2015). A total of 43 features were extracted from the analysis of the volumes inspected. These indices included conventional parameters, shape and size features, histogram-based features, second and high order-based features. The correction for the partial volume effect was not applied. In the analysis were included all incidentalomas, irrespectively of their volume but LifeX calculates the shape and size indices as well as second order (gray-level co-occurrence matrix) and high order-based (neighborhood gray-level different matrix, gray-level run-length matrix, and gray-level zone-length matrix) features only for ROI of at least 64 voxels due to technical reasons. The features calculated are summarized in Table 1. For the features resulted significant, the formula is provided.
Statistical analysis
Statistical analysis was performed using the open source R platform (https://www.r-project.org). Continuous normally distributed data were expressed as mean ± standard deviation. Conventional PET parameters and textural features were compared to SIAPEC-IAP categories and final diagnosis, using the Anova test. A p-value < 0.05 was considered statistically significant.
Receiver operating characteristic (ROC) curves for each parameter were determined and the corresponding area under the curve (AUC) computed for each of those. A preliminary selection of the predictors was computed excluding those with an AUC < 0.55. The mutual correlation between features was evaluated for those metrics, preliminarily selected, in order to assess potential result redundancy.
Among the pre-selected predictors, a further analysis was performed to identify those with statistically significant (or with a tendency to significance) capability to stratify between positive (malignant) and negative (benign) cases. The dichotomization was performed by means of an iterative process aiming to identify the predictor’s threshold minimizing the p-value of the Fisher’s test. The final predictors were selected if p < 0.08.
For each predictor in the final list, the truth table (true and false positive and negative values) was determined at the optimal cutoff value and from this the standard predictive scores were computed.
Results
Table 2 summarizes the descriptive characteristics of the cohort of the patients included in the analysis.
FNA was non-diagnostic in 2 cases, negative in 26 cases, doubtful in 7 cases, suspected in 4 cases, and positive for malignant tumor cells in 11 cases. Patients classified as TIR1, repeated the FNA which resulted negative (TIR2) in both cases. Therefore, considering the re-classification of TIR1 cases, the number of patients belonging to the TIR2 category increased overall to 28. Among the TIR3 cases, 3 were positive and 4 were negative (follicular adenoma = 2, oxyphil cell adenoma = 1, and colloid cystic goiter = 1); while all TIR4 or TIR5 were proven to be malignant. Nodules resulted malignant (n = 18) included 15 thyroid cancers (papillary thyroid cancer = 13, poor differentiated thyroid cancer n = 1, medullary thyroid cancer = 1), 2 metastases from bladder cancer and breast cancer respectively, and 1 lymphoma.
Biochemical data are summarized in Table 3.
Thyroid stimulating hormone (TSH) resulted lower than the low normal limit (< 0.25 mIU/L) in 5 cases (3 benign and 2 malignant). High TSH value (> 4.2 mIU/L, i.e., higher than the upper normal limit) was observed in 4 cases (3 benign and 1 malignant). Anti-thyroid peroxidase antibodies (TPOAb), anti-thyroglobulin antibodies (TgAb), and calcitonin (hCT) were not available for all the patients (Table 2). hCT resulted abnormal in 2/28 cases (both diagnosed as papillary thyroid cancer), while it was normal in the remaining 26/28 cases (including the patient with medullary thyroid cancer).
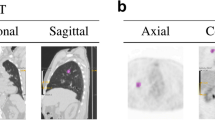
Thyroid [18F]FDG uptake was unilateral in the majority of patients (94%) occurring in the right and the left lobe in 24 and 23 cases, respectively. In the remaining 3 cases (6%) thyroid [18F]FDG uptake involved both lobes. Figures 1 and 2 shows examples of [18F]FDG-PET/CT findings in patients diagnosed as having benign and malignant thyroid nodule. Conventional PET parameters, and histogram-based features were calculated for all patients. Twenty-two patients had small ROI (i.e., < 64 voxels), therefore features extracted from shape and size, GLCM, GLZLM, NGLDM, and GLRLM were available only for 28/50 patients (TIR2 = 15, TIR3 = 4, TIR4 = 2, TIR5 = 7). According to the final diagnosis, 12 out of 28 patients for whom all features were available, resulted positive for malignancy, while in the remaining 16 cases the nodule was diagnosed as benign.
Additional file 1: Table S1 summarizes conventional PET parameters and textural features tabulated according to FNA categories and final diagnosis. Compacity (shape and size-based) was the only feature statistically significant to differentiate the TIR categories (p = 0.03). SUVmax and skewness were significantly different in benign and malignant nodules (p = 0.01 and =0.02, respectively).
Examples of pattern of [18F]FDG uptake at PET/CT images of 2 thyroid incidentalomas identified by the region of interest (red circle). Moderate [18F]FDG uptake was observed in a benign nodule (TIR2 at cytology) of the right thyroid lobe (a) and in a differentiated thyroid cancer (TIR3 at cytology) of the left thyroid lobe (b)
Examples of pattern of [18F]FDG uptake at PET/CT images of 2 thyroid incidentalomas identified by the region of interest (red circle). Intense [18F]FDG uptake was observed in a benign nodule (TIR3 at cytology) of the left thyroid lobe (a) and in a differentiated thyroid cancer (TIR5 at cytology) of the right thyroid lobe (b)
Table 4 summarizes the 7 final features identified as potential predictors (SUVstd, SUVmax, MTV, TLG, Skewness, Kurtosis, CorrelationGLCM) with their mean values, the AUC, the best threshold for the dichotomization of the cohort and the final p value.
Figure 3 shows the box-plots of the 7 final features stratified for the two subgroups in the cohort. Figure 4 shows the ROC curves (together with the reference 50% AUC line) for the volume and the texture related features. Among the potential predictors a mutual correlation was found between SUVstd and SUVmax (0.967), TLG and MTV (0.970), as well as skewness and kurtosis (0.830), as shown in Table 5.
None of the features which presented a mutual correlation were excluded from further analysis.
Table 6 summarizes the predictors and their power in the identification of the negative or positive subgroups in the cohort. SUVstd and SUVmax showed the highest specificity while MTV, TLG, skewness and kurtosis, as well as correlationGLCM resulted better in sensitivity.
The average positive predictive value of the 7 features resulted 54% while the average negative predictive value 85%.
Discussion
The current study, although in a limited number of patients, showed that PET-derived metrics could be used to characterize incidentalomas. Both SUVmax (conventional parameter) and skewness (histogram-based feature) differed significantly in benign and malignant thyroid nodules. In our cohort, we report prevalence of thyroid incidentaloma in line with literature data (2.6% versus 1.2–4.3%) (Rigo et al. 1996; Mitchell and Parangi 2005; Liu et al. 2010), with a low rate (i.e., < 55% (Gavriel et al. 2015)) of additional workup (ultrasound and cytology available in 19% and 12% of subjects, respectively), but a relatively high rate of malignancy (36%).
Our results confirmed data reporting that malignant nodules had higher [18F]FDG uptake (SUVmax) than those resulted benign (Gavriel et al. 2015; Demir et al. 2016; Chun et al. 2015; Kim and Chang 2015). However, although SUVmax is the conventional PET parameter most used in clinical practice, there are several sources of bias and variability including patients’ status (e.g., blood glucose level, impaired renal function), that affect its measurement (Kinahan and Fletcher 2010; Huang 2000).
Radiomics is a post-processing approach correlating image texture parameters to clinical, genetic and prognostic variables, and it is applicable to all types of images. Time for texture processing varies among software used for both images segmentation and features extraction. In this series of patients we spent few minutes from thyroid nodule segmentation (about 3 min/patient including also time to retrieve and download images) to features extraction (about 2 min/patient depending on ROI volume). Once texture analysis tool will be implemented in the workstation used for clinical purpose, texture features extraction will be faster as it is currently for conventional parameters. Texture analysis of [18F]FDG-PET/CT images provides quantitative parameters describing tissue metabolic heterogeneity and seems to perform better than the conventional PET metrics in several malignances, but data on [18F]FDG-PET/CT radiomics in thyroid nodules are limited. Kim et al. (Kim and Chang 2015) investigated the intratumoral heterogeneity of [18F]FDG uptake, defined as the heterogeneity factor (HF) obtained from the derivative (dV/dT) of a volume-threshold function – a first order statistical-based approach. The authors found that HF represented a promising method for prediction of malignant thyroid nodule in 200 patients with [18F]FDG-PET/CT incidentaloma (Kim and Chang 2015). The global tumor heterogeneity may be described by using first order histogram-based features; the second-order GLCM-features that quantify local heterogeneity at the scale of a voxel; the features derived from high-order which quantify regional heterogeneity based on the neighborhood, the respective sizes and intensities of groups of voxels (Sollini et al. 2017). In the present work these parameters have been tested. In our series of patients, skewness was the only textural feature which showed a trend to differentiate benign from malignant nodules. Skewness, measuring the asymmetry of the probability distribution of intensity values about its mean, provides information about lesion heterogeneity. Considering the predictors selected in our population, SUVmax resulted in the highest specificity (81% versus 66%, 69%, and 31%) while TLG, skewness, as well as correlationGLCM resulted better in sensitivity (100% versus 50% for SUVmax and 72% for both TLG and skewness). Therefore, based on its high negative predictive value, correlationGLCM could be used to rule out a diagnosis of a malignant nodule, although its low specificity.
[18F]FDG uptake distribution has been associated with underlying physiopathological characteristics such as vascularization, perfusion, tumor aggressiveness, necrosis, hypoxia and gene expression (Tixier et al. 2014; Basu et al. 2011; Kunkel et al. 2003). Therefore, it is reasonable to hypothesize that significantly different values of PET image-derived heterogeneity quantification features may be observed in benign and malignant thyroid nodules, based on the different underlying physiopathological properties.
The parameters derived from routinely performed PET images may impact on clinical practice. In fact, up to 20% of FNA samples fall into category of insufficient/inadequate cytology, and approximately 15% to 30% of thyroid FNAs fall in an interpretive gray zone, in which the probability of malignancy is considered too high for watchful waiting but insufficient to propose a total thyroidectomy (Wise and Howard 2016; Bongiovanni et al. 2012; Cibas and Ali 2009; Nishino 2016). Aspirates in the “follicular neoplasm/suspicious for a follicular neoplasm” category (category TIR3B according to the update version of the SIAPEC-IAP (Nardi et al. 2014)) are typically associated with a 15%–30% risk of malignancy, therefore patients are generally referred for diagnostic thyroid lobectomy. Repeat FNA is the usual management for aspirates in the category of “atypia of undetermined significance/follicular lesion of undetermined significance” (TIR3A according to the update version of the SIAPEC-IAP (Nardi et al. 2014)) due to a 5%–15% risk of malignancy, with diagnostic lobectomy considered for nodules with repeatedly indeterminate FNA cytology (Nishino 2016). Therefore, the possibility to identify thyroid nodule with a high risk of malignancy, using texture analysis of conventional imaging on which the incidentaloma has been discovered, would have a great impact in clinical practice, determining better selection of patients proposed for FNA and guide patient management. The 2015 American Thyroid Association Management Guidelines (Haugen et al. 2016) recommend FNA in case of focal [18F]FDG uptake within a sonographically confirmed thyroid nodule ≥ 1 cm (strong recommendation, moderate-quality evidence). It is true that a focal [18F]FDG uptake within a thyroid nodule has an increased risk of malignancy, but it is also true that not all thyroid nodules characterized by a focal [18F]FDG uptake are malignant. Additionally, the number of passes for an adequate thyroid FNA can vary considerably, and a variety of factors, including operator’s skill, can influence its adequacy (Pitman et al. 2008). Therefore, the chance to identify through texture analysis patients who can benefit from additional workup for thyroid incidentaloma, could result in fewer FNA procedures and possibly fewer diagnostic thyroid lobectomies, decreasing consequently the cost for the healthcare system, and improving patients’ quality of life.
The present study has some limitations. Firstly, it is retrospective and evaluated a limited number of patients. In fact, only a small percentage of patients performed FNA and had a final diagnosis (12% and 11%, respectively) among all those for whom a focal [18F]FDG uptake was described in the PET/CT report. This is partly related to the fact that in our institution sonographers have a high expertise, thus cytological examinations are reserved only to patients presenting doubtful or suspected ultrasound findings; secondly to the fact that many patients who performed a PET/CT scan in our hospital were followed-up in other institutions. Therefore, we limited the analysis only to patients who performed the additional workup (i.e., ultrasound, FNA and histology) in our center. Conventional parameters and textural features were not tested within malignant nodules to differentiate thyroid cancer from other malignancies due to the disproportion of sample size in the two subsets of patients. Some features, including shape and size, GLCM, GLZLM, NGLDM, and GLRLM-based metrics, were available for approximately a half of cases, potentially underestimating the potentiality of this innovative approach. This limitation is related to the fact that the software used for texture doesn’t calculate features for volumes smaller than 64 voxels, as can be thyroid nodule. A validation of our results was not done. Finally, correction for the partial volume effect has not been performed.
Conclusions
PET texture-derived features seem able to stratify the patients with thyroid incidentaloma identified on [18F]FDG-PET/CT scans, with respect to the risk of the diagnosis of a malignant thyroid nodule. Thus, the patients to be referred for FNA may be properly selected using post-processing techniques on routinely performed imaging on which the thyroid incidentaloma has been discovered.
Abbreviations
- [18F]FDG:
-
2-deoxy-2-[18F]fluoro-D-glucose
- 3D:
-
Tridimensional
- AUC:
-
Area under the curve
- EAMN:
-
European Association of Nuclear Medicine
- EARL:
-
EANM Research Ltd.
- FNA:
-
Fine-needle aspiration
- GLCM:
-
Gray-level co-occurrence matrix
- GLRLM:
-
Gray-level run-length matrix
- GLZLM:
-
Gray-level zone-length matrix
- hCT:
-
Calcitonin
- Hist:
-
Histogram
- MTV:
-
Metabolic tumor volume
- NGLDM:
-
Neighborhood gray-level different matrix
- PET:
-
Positron emission tomography
- PET/CT:
-
Positron emission tomography/computed tomography
- ROC:
-
Receiver operating characteristic
- ROI:
-
Region of interest
- SIAPEC-IAP:
-
Italian Society for Anatomic Pathology and Cytology joint with the Italian Division of the International Academy of Pathology
- SUVmax :
-
Maximum standardized uptake value
- TgAb:
-
Anti-thyroglobulin antibodies
- TLG:
-
Total lesion glycolysis
- TPOAb:
-
Anti-thyroid peroxidase antibodies
- TSH:
-
Thyroid stimulating hormone
References
Are C, Hsu JF, Schoder H, Shah JP, Larson SM, Shaha AR (2007) FDG-PET detected thyroid incidentalomas: need for further investigation? Ann Surg Oncol 14:239–247
Barrio M, Czernin J, Yeh MW, Palma Diaz MF, Gupta P, Allen-Auerbach M et al (2016) The incidence of thyroid cancer in focal hypermetabolic thyroid lesions: an 18F-FDG PET/CT study in more than 6000 patients. Nucl Med Commun 37:1290–1296
Basu S, Kwee TC, Gatenby R, Saboury B, Torigian DA, Alavi A (2011) Evolving role of molecular imaging with PET in detecting and characterizing heterogeneity of cancer tissue at the primary and metastatic sites, a plausible explanation for failed attempts to cure malignant disorders. Eur J Nucl Med Mol Imaging 38:987–991
Boellaard R, Delgado-Bolton R, Oyen WJG, Giammarile F, Tatsch K, Eschner W et al (2014) FDG PET/CT: EANM procedure guidelines for tumour imaging: version 2.0. Eur J Nucl Med Mol Imaging 42:328–354
Bongiovanni M, Spitale A, Faquin WC, Mazzucchelli L, Baloch ZW (2012) The Bethesda system for reporting thyroid Cytopathology: a meta-analysis. Acta Cytol 56:333–339
Buvat I, Orlhac F, Soussan M (2015) Tumor texture analysis in PET: where do we stand? J Nucl Med 56:1642–1644
Chun AR, Jo HM, Lee SH, Chun HW, Park JM, Kim KJ et al (2015) Risk of malignancy in thyroid Incidentalomas identified by Fluorodeoxyglucose-positron emission tomography. Endocrinol Metab 30:71–77
Cibas ES, Ali SZ (2009) The Bethesda system for reporting thyroid Cytopathology. Am J Clin Pathol 132:658–665
Cohen MS, Arslan N, Dehdashti F, Doherty GM, Lairmore TC, Brunt LM et al (2001) Risk of malignancy in thyroid incidentalomas identified by fluorodeoxyglucose-positron emission tomography. Surgery 130:941–946
Davies L, Pichiotino E, Black WC, Tosteson AN (2016) Developing a registry for thyroid Incidentalomas: lessons learned and the path forward. Thyroid 26:650–656
Demir Ö, Köse N, Özkan E, Ünlütürk U, Aras G, Erdoğan MF (2016) Clinical significance of thyroid incidentalomas identified by 18F-FDG PET/CT: correlation of ultrasonograpy findings with cytology results. Nucl Med Commun 37:715–720
Fadda G, Basolo F, Bondi A, Bussolati G, Crescenzi A, Nappi O et al (2010) Cytological classification of thyroid nodules. Proposal of the SIAPEC-IAP Italian consensus working group. Pathologica 102:405–408
Gavriel H, Tang A, Eviatar E, Chan SW (2015) Unfolding the role of PET FDG scan in the management of thyroid incidentaloma in cancer patients. European archives of Oto-rhino-Laryngology. Springer. Berlin Heidelberg 272:1763–1768
Haugen BR, Alexander EK, Bible KC, Doherty GM, Mandel SJ, Nikiforov YE et al (2016) 2015 American Thyroid Association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: the American Thyroid Association guidelines task force on thyroid nodules and differentiated thyroid cancer. Thyroid 26:1–133
Huang SC (2000) Anatomy of SUV. Standardized uptake value. Nucl Med Biol 27:643–646
Kim SJ, Chang S (2015) Predictive value of intratumoral heterogeneity of F-18 FDG uptake for characterization of thyroid nodules according to Bethesda categories of fine needle aspiration biopsy results. Endocrine Springer US 50:681–688
Kinahan PE, Fletcher JW (2010) PET/CT standardized uptake values (SUVs) in clinical practice and assessing response to therapy. Semin Ultrasound CT MR 31:496–505
Kunkel M, Reichert TE, Benz P, Lehr H-A, Jeong J-H, Wieand S et al (2003) Overexpression of Glut-1 and increased glucose metabolism in tumors are associated with a poor prognosis in patients with oral squamous cell carcinoma. Cancer 97:1015–1024
Lee S, Park T, Park S, Pahk K, Rhee S, Cho J et al (2014) The clinical role of dual-time-point (18)F-FDG PET/CT in differential diagnosis of the thyroid Incidentaloma. Nucl Med Mol Imaging 48:121–129
Liu Y, Ghesani NV, Zuckier LS (2010) Physiology and pathophysiology of incidental findings detected on FDG-PET scintigraphy. Seminars Nuclear Med 40:294–315
Mitchell J, Parangi S (2005) The thyroid incidentaloma: an increasingly frequent consequence of radiologic imaging. Semin Ultrasound CT MR. 26:37–46
Nardi F, Basolo F, Crescenzi A, Fadda G, Frasoldati A, Orlandi F et al (2014) Italian consensus for the classification and reporting of thyroid cytology. Journal of Endocrinological investigation. Springer Int Publishing 37:593–599
Nayan S, Ramakrishna J, Gupta MK (2014) The proportion of malignancy in incidental thyroid lesions on 18-FDG PET study: a systematic review and meta-analysis. Otolaryngol Head Neck Surg 151:190–200
Nilsson I-L, Arnberg F, Zedenius J, Sundin A (2011) Thyroid incidentaloma detected by fluorodeoxyglucose positron emission tomography/computed tomography: practical management algorithm. World J Surg 35:2691–2697
Nishino M (2016) Molecular cytopathology for thyroid nodules: a review of methodology and test performance. Cancer Cytopathol 124:14–27
Orlhac F, Soussan M, Chouahnia K, Martinod E, Buvat I (2015) 18F-FDG PET-derived textural indices reflect tissue-specific uptake pattern in non-small cell lung cancer. PLoS One 10:1–16
Orlhac F, Nioche C, Buvat I. Technical appendix — local image features extraction — — LIFEx —. 2016
Pagano L, Samà MT, Morani F, Prodam F, Rudoni M, Boldorini R et al (2011) Thyroid incidentaloma identified by 18F-fluorodeoxyglucose positron emission tomography with CT (FDG-PET/CT): clinical and pathological relevance. Clin Endocrinol 75:528–534
Pitman M, Abele J, Ali S, Diuck D, Elsheikh T, Jeffrey R et al (2008) Techniques for thyroid FNA: a synopsis of the National Cancer Institute thyroid fine-needle aspiration state of the science conference. Diagn Cytopathol 36:407–424
Rigo P, Paulus P, Kaschten BJ, Hustinx R, Bury T, Jerusalem G et al (1996) Oncological applications of positron emission tomography with fluorine-18 fluorodeoxyglucose. Eur J Nucl Med 23:1641–1674
Soelberg KK, Bonnema SJ, Brix TH, Hegedüs L (2012) Risk of malignancy in thyroid incidentalomas detected by 18F-fluorodeoxyglucose positron emission tomography: a systematic review. Thyroid 22:918–925
Sollini M, Cozzi L, Antunovic L, Chiti A, Kirienko M (2017) PET Radiomics in NSCLC: state of the art and a proposal for harmonization of methodology. Scic Rep 7:358
Tixier F, Groves AM, Goh V, Hatt M, Ingrand P, Cheze Le Rest C et al (2014) Correlation of intra-tumor18F-FDG uptake heterogeneity indices with perfusion CT derived parameters in colorectal cancer. PLoS One 9:8–9
Wise O, Howard MR (2016) Thyroid cytology: a review of current international reporting systems and emerging developments. Cytopathology 27:161–167
Funding
None.
Author information
Authors and Affiliations
Contributions
The manuscript has been seen and approved by all authors, whose individual contributions were as follows: MK and MS conceptualized the paper; AL contributed to patient selection and management; LA and GP performed and interpreted nuclear medicine imaging; PM performed ultrasound images and FNA; LDT provided cytological results; MS and GP contributed to data selection; MS and CL performed the images and statistical analysis; MS and CL wrote the paper and provided figures and tables; PAE supervised the project and paper writing.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Local Ethics Committee (authorization number 1706). A specific informed consent was not required according to Local Ethics Committee rules for retrospective and observational study design (the patient management was not influenced or changed).
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional file
Additional file 1: Table S1.
Conventional PET parameters and textural features tabulated according FNA categories and final diagnosis. (DOCX 84 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Sollini, M., Cozzi, L., Pepe, G. et al. [18F]FDG-PET/CT texture analysis in thyroid incidentalomas: preliminary results. European J Hybrid Imaging 1, 3 (2017). https://doi.org/10.1186/s41824-017-0009-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41824-017-0009-8